Abstract
This paper outlines the development of a distinctive, full-time, 3-year postgraduate Master of Science (MSc) program in Orofacial Pain and Dysfunction (OPD), which integrates advanced clinical training, interdisciplinary care and research publication.
Keywords: orofacial pain, bruxism, tooth wear, obstructive sleep apnea, dental education
Evolution of a dental discipline
Over the past decades, the dental discipline of orofacial pain and dysfunction (OPD) has evolved globally from a rather narrow, mainly dental domain with a major focus on temporomandibular disorders (TMDs) to a much broader, more medical domain that encompasses not only TMDs, but also other (non-dentoalveolar) types of orofacial pain (including neuropathic pain and headaches), oral movement disorders (including one of their most common and sometimes debilitating consequences, i.e., tooth wear in association with bruxism) and dental sleep disorders (including obstructive sleep apnea (OSA), gastroesophageal reflux (GER) and oral moistening disorders). Due to the multifactorial nature of the numerous conditions that are part of the OPD discipline, some of them partly overlapping with other dental disciplines (e.g., endodontology, oral and maxillofacial surgery) and many of them also being part of several medical disciplines (e.g., neurology, otolaryngology, anesthesiology, rheumatology), OPD requires dentists with specialized knowledge and skills to assess and manage the patients affected by OPD conditions in interdisciplinary settings. In 2020, the National Commission on Recognition of Dental Specialties recognized orofacial pain as the 12th dental specialty in the USA.1 Notably, also elsewhere in the world, there is an increasing focus on more and better OPD training. This global evolution of the OPD discipline has paved the way for new educational programs.
A new postgraduate OPD program
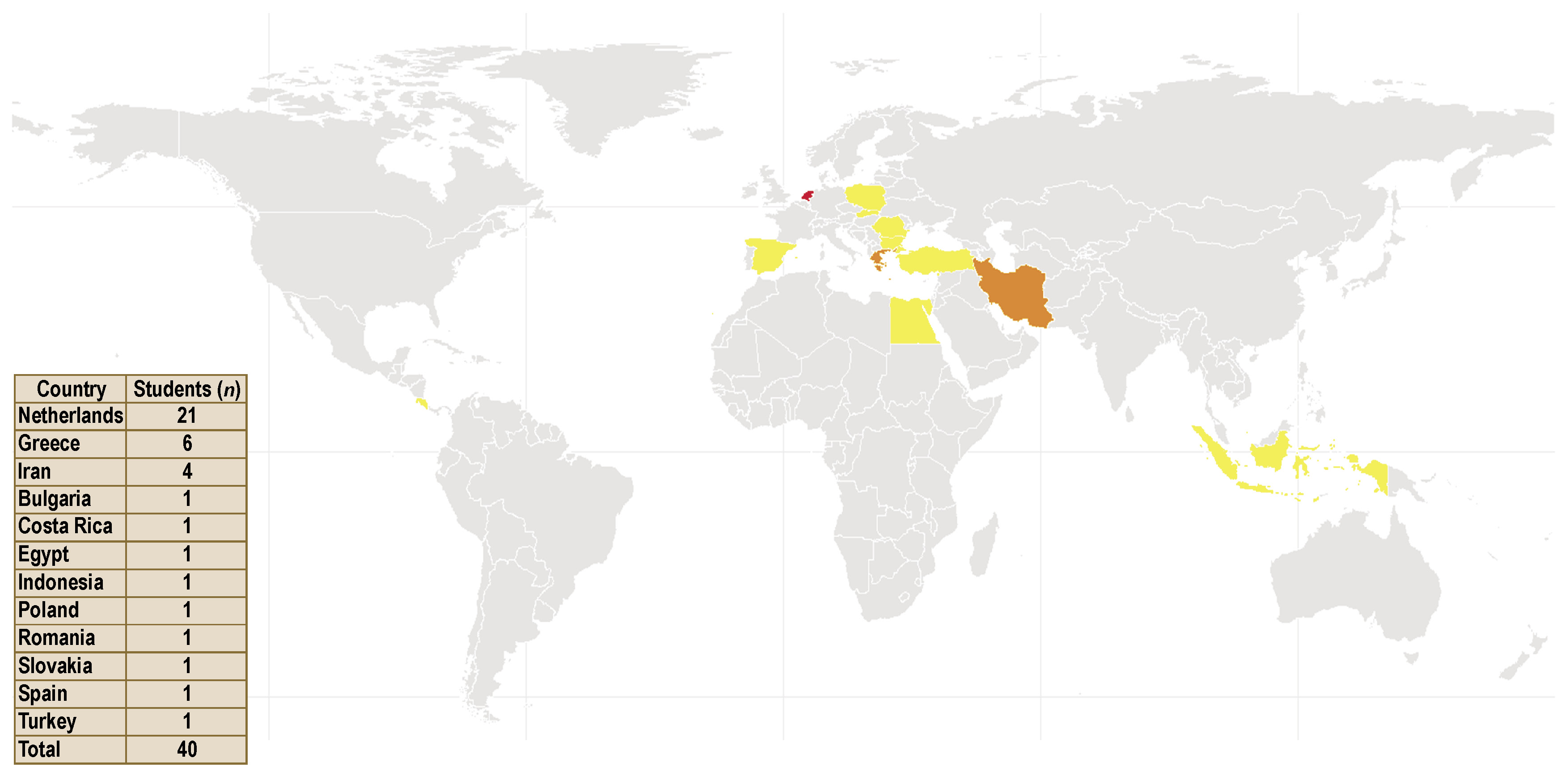
In anticipation of this global evolution, a 3-year postgraduate OPD program was developed at the Academic Centre for Dentistry Amsterdam (ACTA), the Netherlands. In September 2003, the first student was admitted to the program. From the start, the program was officially recognized by the University of Amsterdam as a postgraduate Master of Science (MSc) program. Information on the background and design of this new program was published previously.2 The program had a director (Prof. Frank Lobbezoo) and a co-director (Dr. Jacques van der Zaag), and attracted students from many different countries – most of them from the Netherlands, but also significant numbers from Greece, other European countries, and beyond (Figure 1). The program’s graduates, the first one finalizing in June 2006, pursued different careers. Some stayed at the Department of Orofacial Pain and Dysfunction of ACTA to obtain their PhD degree and/or to become a teacher/clinician, while others started a career as an orofacial pain specialist at another academic institution, in a center for special dental care or in a private practice, either in the Netherlands or outside. Yet others returned to their home country for the next phase in their careers.
Oral Health Sciences program
Around the time of the start of the OPD program in 2003, ACTA had several other postgraduate programs to offer. Some of them were well-established, like the ones for Periodontology and Endodontology; others, including the OPD program, were more in their infancies, like the ones for Pediatric Dentistry and Implantology/Prosthodontics. All programs had their own design, management and, in some cases, accreditation. It was ACTA’s ambition to create a single postgraduate program, with several graduation profiles (i.e., OPD, Periodontology, Endodontology, Pediatric Dentistry, and Implantology/Prosthodontics). The overarching postgraduate program was named Oral Health Sciences (OHS): A 3-year full-time program, taught in English, with 60 European Credits (ECs) per year – hence 180 ECs in total. The postgraduate OHS program started in September 2015. The OPD profile continued with a structure that was comparable to the early days, but now embedded in the larger OHS structure with its additional modules and activities. From the start of the newly structured program, the profile director was Dr. Peter Wetselaar, with Prof. Frank Lobbezoo as the co-director. In 2022, the role of profile director was taken over by Dr. Michail Koutris.
Uniqueness of the program
The OPD profile of the postgraduate OHS program,3 or the OPD-OHS program in short, is unique for several reasons. It is one of the few full-time programs worldwide that train dentists in all aspects of OPD (supervisors: Dr. Michail Koutris, Prof. Frank Lobbezoo, Dr. Marisol Reyes-Sevilla, and Prof. Corine M. Visscher), including dental sleep disorders (supervisors: Prof. Ghizlane Aarab and Dr. Marisol Reyes-Sevilla) and tooth wear (supervisors: Dr. Ruud H. Kuijs, Dr. Chryssa Papagianni and Dr. Peter Wetselaar). For the latter condition, a specialized clinic was founded at the Department of Orofacial Pain and Dysfunction that focuses on the assessment, management and – when indicated – restorative treatment of the worn dentition, using non- or minimally invasive techniques whenever possible. Also the patients referred with a diagnosis of OSA are treated in a specialized departmental clinic, where, besides counseling, mandibular advancement appliances are offered. And obviously, a large clinic for OPD is part of the department’s clinical realm. In that clinic, an interdisciplinary team is active, including orofacial pain specialists (in training), orofacial physical therapists, and health psychologists. In such a rich clinical environment, the postgraduate students are immersed in the complex and interconnected problems of the patients living with OPD conditions, which contributes enormously to the students’ development as orofacial pain specialists. Of important notice is the fact that in all parts of the clinic, clinicians work according to the newest insights and guidelines, including those for orofacial pain and TMDs,4, 5, 6, 7, 8, 9, 10 bruxism,11, 12, 13, 14, 15 tooth wear,16, 17, 18 and OSA.19, 20
Apart from the clinical and educational components of the OPD-OHS program, the postgraduate students are required to perform a research project as part of their training. The project is preferably of such a level that the publication of the outcomes in an international peer-reviewed journal is possible. Indeed, most students manage to have their work published, while all students produce a postgraduate master’s thesis that includes a detailed description of their research. In Table 1, some examples of the published works of the postgraduate students of the OPD profile are provided. From the listed co-authors of these publications, the team of supervisors of the various projects can be gathered.
Finally, at the end of the program, the students are examined by an external examiner and an (independent) internal examiner. During a full examination day, the students present selected patient cases to the examiners to show their competence in clinical decision-making in interdisciplinary work. In addition, the students present their portfolio, which includes not only their research report/international publication, but also the output of all the teaching components. Based on their performance, students can fail, pass, or pass with distinction, based on rubrics that guide the examiners with their grading. The international examiners are invited based on their expertise, international reputation and profile. They are always affiliated with reputable academic dental institutions from all over Europe. Table 2 provides an overview of the external examiners who were invited between 2006 and 2025.
Conclusion
The international English-language postgraduate Oral Health Sciences (OHS) program, profile Orofacial Pain and Dysfunction (OPD), offers full-time, 3-year training for dentists specializing in an evolving dental/medical discipline that includes conditions like orofacial pain, TMDs, oral movement disorders, tooth wear, and dental sleep disorders. Since its start in 2003, 40 OPD specialists have graduated from the program. Most of them have continued (and continue) to work in the field of OPD and contribute, in various capacities, to the further growth and development of this highly interdisciplinary discipline. We look back on 2 decades of a successful program that continues to evolve toward a bright future.