Abstract
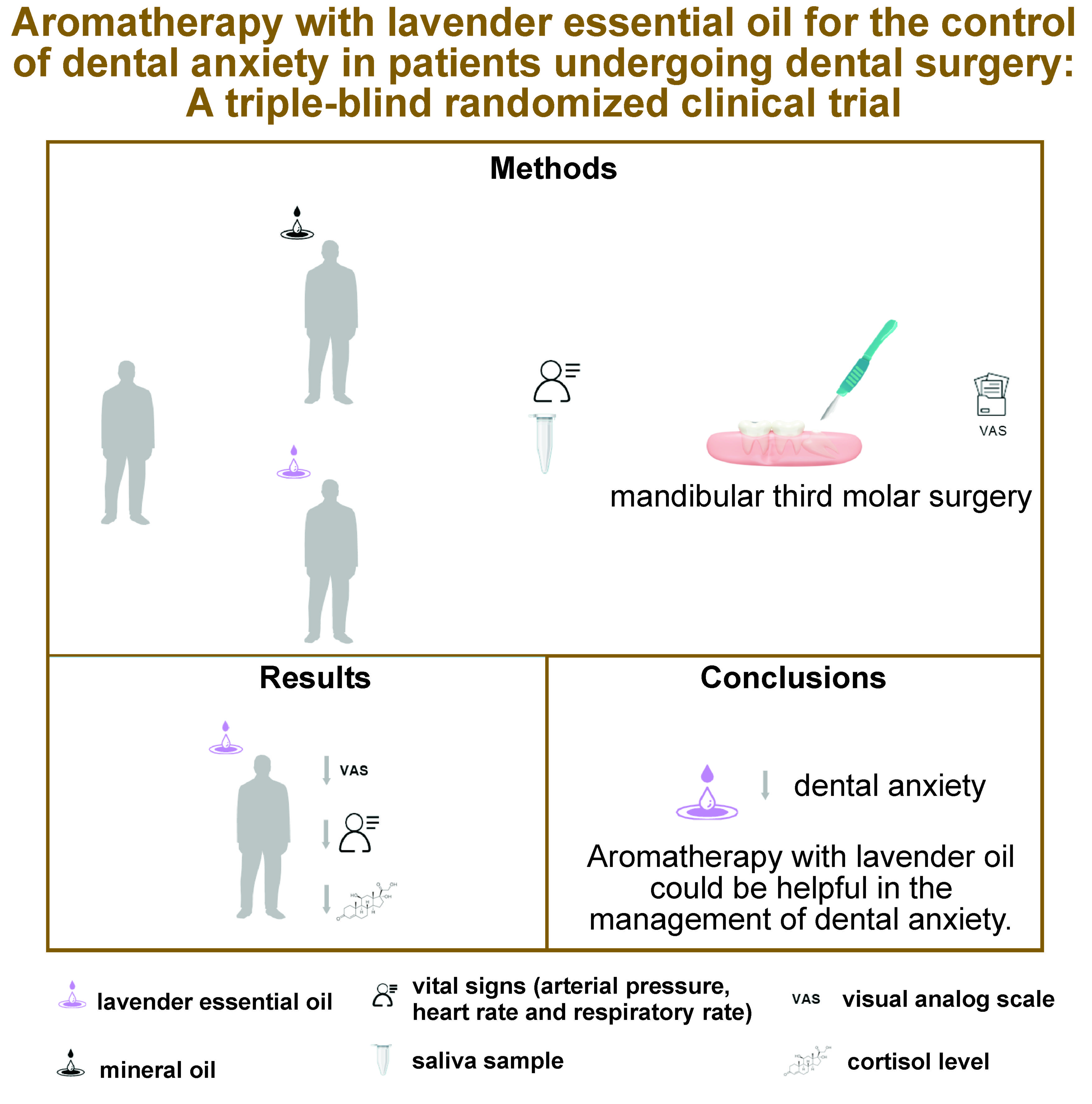
Background. Anxiety resulting from dental treatment often leads to avoidance of dental appointments and consequently has a negative impact on oral health. Non-pharmacological approaches have been identified as suitable alternatives for the management of dental anxiety. In this context, lavender oil has traditionally been used in aromatherapy (AT) due to its sedative, carminative, antidepressive, anti-inflammatory, and antimicrobial properties.
Objectives. The aim of the study was to perform a triple-blind randomized clinical trial to address the effectiveness of AT with lavender essential oil (ATL) on the dental anxiety of patients undergoing mandibular third molar surgery.
Material and methods. Participants scheduled to undergo mandibular third molar surgery were enrolled in the study and randomly assigned to either the ATL group or the control group. Dental anxiety was assessed using the preoperative Modified Dental Anxiety Scale (MDAS). Vital signs were evaluated before and after the intervention. Cortisol levels were measured by enzyme-linked immunosorbent assay (ELISA). Additionally, a visual analog scale (VAS) was used, and the requirements for anesthesia were determined.
Results. A comparison of the pre-operative MDAS scores between the ATL and control groups revealed no statistically significant differences (p = 0.268). The levels of respiratory rate (RR) (p = 0.011) and heart rate (HR) (p = 0.021) significantly decreased in the ATL group after the intervention. Also, the number of local anesthetic cartridges needed (p = 0.030) and cortisol levels (p < 0.0001) were significantly lower in the ATL group.
Conclusions. The evidence suggests that ATL could be helpful in the management of dental anxiety.
Keywords: dentistry, dental anxiety, complementary medicine
Introduction
Herbal medicines encompass both unprocessed natural herbs and finished products that incorporate active ingredients derived from plants. The World Health Organization (WHO) has established that 80% of the global population relies on herbal medicine for their primary healthcare needs. Moreover, a quarter of pharmaceuticals used in developed countries include herbal compounds and their derivatives.1 Herbal medicine, ozone and acupuncture have begun to be used as complementary therapies (CTs) in dentistry to relieve dental pain and pain associated with temporomandibular joint dysfunctions.2 Also, CTs have been employed as coadjutants in the treatment of gingivitis, aphthous ulcers, and integrative head and neck cancer management.3, 4
Aromatherapy (AT) is a CT that uses essential oils extracted from fresh plants for therapeutic purposes.5 Aromatherapy consists of the application of essential oils to the skin through massage or inhalation of their vapors. Lavender oil is traditionally used in AT due to its sedative, carminative, antidepressive, anti-inflammatory, and antimicrobial effects.6 The genus Lavandula encompasses 32 species, which fall into 4 main categories: L. latifolia; L. angustifolia; L. stoechas; and L. intermedia. These species share similar ethnobotanical properties and main chemical constituents, as evidenced by the sedative properties exhibited by both linalool and floral monoterpene.7 Pharmacological studies in mice have associated the linalool odor with anxiolytic effects mediated by γ-aminobutyric acid (GABA)ergic transmission at the central nervous system (CNS).8 Besides, linalool has demonstrated antidepressant and anti-stress effects mediated by an augmentation of serotonin and a diminution of cortisol levels in a rapid eye movement (REM) sleep-deprived model.9 Likewise, linalool odor could modulate cortisol levels in humans subjected to experimental stress.10
Dental anxiety, defined as an irrational fear of undergoing dental treatment, is a prevalent condition that has been classified as a phobia.11 The anxious behavior triggered by dental treatment leads patients to miss appointments and, therefore, has a negative impact on their oral health. The methods used to manage dental anxiety include psychophysiological therapy, premedication with anxiolytics, conscious sedation, and, on occasion, general anesthesia.12 However, these approaches frequently have considerable adverse effects, making nonpharmacological methods potentially advisable options for treating dental anxiety.13
The present study aimed to perform a triple-blind randomized clinical trial to address the effectiveness of aromatherapy with lavender essential oil (ATL) on dental anxiety of patients undergoing third molar surgery.
Material and methods
Sample calculation and experimental group distribution
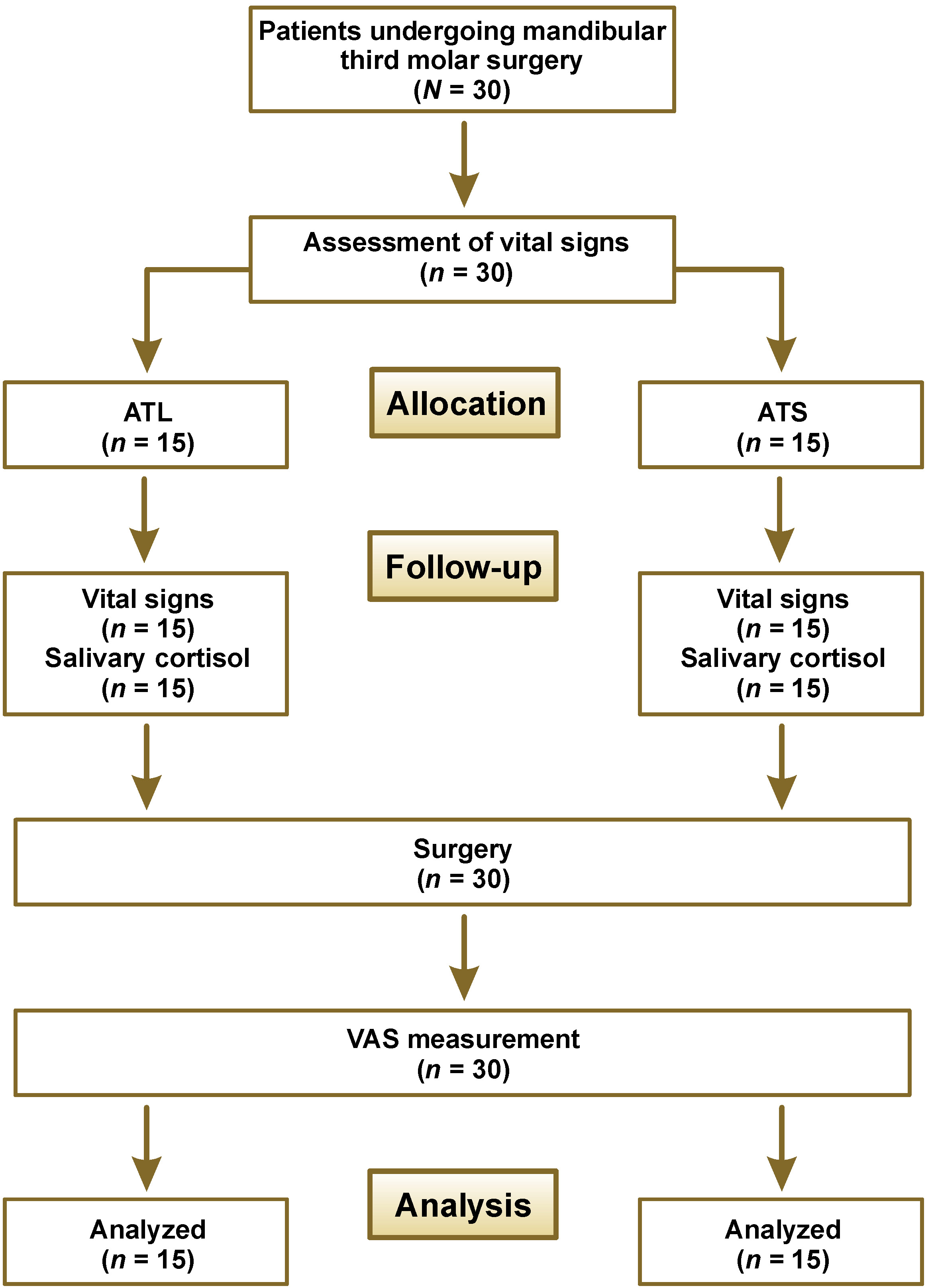
Power analysis was performed using G*Power software (v. 3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) to calculate the size of the study sample (input: two tails, effect size (d) = 0.5, α error probability = 0.05, power (1−β error probability) = 0.90, allocation ratio N2/N1 = 1).14 The sample size of 90 individuals per group was determined. Patients undergoing mandibular third molar surgery were randomly allocated by the principal investigator (RTR) to one of 2 groups using random number generation with QuickCalcs in GraphPad Prism 9 software (GraphPad Software, La Jolla, USA). Another researcher enrolled the participants (CJSM), and a third researcher assigned the subjects to the interventions (EMVJ). The experimental group received ATL, while the control group received a placebo consisting of mineral oil (ATS) (Figure 1).
Eligibility criteria
The included patients were apparently healthy participants of any sex, aged between 18 and 40 years, who required mandibular third molar surgery and agreed to participate in the study by signing the informed consent form. The exclusion criteria encompassed patients who did not meet the inclusion criteria or who had mental conditions, heart disease, upper respiratory tract infections, an allergy to lavender, or those undergoing drug treatment for mental disorders. Additionally, patients who presented any complication of the surgical procedure and those who voluntarily withdrew from the study were excluded.
Intervention
Following previous reports, a medical patch containing 100 µL of lavender essential oil was placed in close proximity to the nose of each participant (avoiding skin contact) for 40 min before the dental surgery.15, 16 The essential oil of lavender (L. angustifolia), which had been marketed for clinical use, was obtained from PACALLI (Monterrey, México). The ATS group inhaled pure mineral oil in the same conditions.
Primary outcomes
Dental anxiety
Each participant completed the Modified Dental Anxiety Scale (MDAS) 45 min before the dental treatment. The MDAS is a questionnaire comprising 5 questions that are rated on a 5-point Likert scale. The total score is used to classify the level of anxiety, as follows: null anxiety; low anxiety; moderate anxiety; high anxiety; and severe anxiety. The precoded responses range from “null anxiety” (score 1) to “severe anxiety” (score 5).
Cortisol quantification
Saliva samples were collected 30 min after the administration of ATL or ATS. The samples were preserved at −80°C in polypropylene tubes before cortisol was quantified using the enzyme-linked immunosorbent assay (ELISA) (K008B; R&D Systems Inc., Minneapolis, USA) according to the manufacturer’s instructions. The measurements were performed by a researcher who was blinded (LAF) regarding allocation to study groups.
Secondary outcomes
Vital signs
Heart rate (HR), respiratory rate (RR) and arterial pressure (AP) were assessed 5 min before ATL or ATS (denoted by the letter b next to the variable’s abbreviation) and 30 min after the beginning of ATL or ATS (denoted by the letter a next to the variable’s abbreviation) by a dental assistant who was blinded to study group allocation.
Pain
The surgeon, unaware of the study group allocation, used the visual analog scale (VAS) to assess pain levels. This continuous scale is represented by a horizontal line of 10 cm in length. At one extreme of the scale, no pain is represented by 0, while at the other extreme, unbearable pain is represented by 10. The score was determined by measuring the distance in centimeters using a ruler. The scale was assessed 5 min after the surgery.
Anesthetic requirement
The dose of local anesthetic administered to each patient was recorded during the surgical procedure.
Statistical analysis
The data was analyzed using GraphPad Prism 9 software (GraphPad Software). The normality of the data was assessed by the Shapiro–Wilk test. The Student’s t-test or Mann–Whitney U test was used to determine the mean or mean rank differences between the groups. The level of statistical significance was set at p ≤ 0.05.
Results
The present clinical trial included 30 patients who underwent mandibular third molar surgery. Regarding sex distribution, 53.3% of the participants were female and 46.7% were male. The mean age of the subjects was 26 years (Table 1). No participants withdrew from the study. Also, no cases of adverse effects or allergic reactions have been reported.
The results of the normality test indicated that the data was normally distributed for MDAS, HRb, RRb, and cortisol level. On the other hand, the following variables did not follow a normal distribution: HRa; RRa; diastolic arterial pressure (DAP)b; DAPa; systolic arterial pressure (SAP)a; SAPb; VAS; and anesthetic requirement (AR).
Both groups displayed equal MDAS at baseline. Concerning the clinical sympathetic activity in the heart, HR in both groups showed similar results at baseline. However, after the intervention, HR exhibited lower values in the ATL group. On the other hand, for both groups, DAP and SAP demonstrated similar results at baseline and after the intervention. The respiratory rate in both groups presented similar results at baseline; however, after the intervention, lower RR values were noted in the ATL group. The cortisol level was significantly lower in the ATL group. Nevertheless, AR was significantly lower in the ATL group (Table 2).
Discussion
Dental fear is very common, and the coronavirus disease 2019 (COVID-19) pandemic caused an increase in dental anxiety levels among patients.17, 18, 19 Several CTs have been studied for anxiety control, such as acupuncture, music therapy, massage, and AT.20, 21, 22, 23, 24, 25 However, conflicting results have been reported regarding the effectiveness of acupuncture, as it is an invasive therapy that involves the insertion of needles into muscle tissue. Furthermore, it would be difficult to administer acupuncture before the dental appointment, as it must be performed by a specialist.26, 27 On the other hand, music therapy has been shown to reduce salivary cortisol concentration, SAP, DAP, HR, body temperature, and stimulated salivary flow. However, it has been pointed out that the patient’s musical preferences may influence the results, and that music may function more as a distraction than as a therapy in itself if it is not delivered directly to the patient through headphones. Additional concerns have been made regarding the hygiene of the headphones or the potential financial implications for the patient.28, 29 Massage, like acupuncture, necessitates the expertise of a specialist and a suitable environment for its administration prior to the dental appointment, which makes this option impractical.30
Essential oils extracted from aromatic herbal sources have sedative and stress-relieving properties.31 The evidence for these properties has been obtained through in vivo studies and clinical trials in humans, which demonstrated the physiological effects of odorant inhalation.8 In some clinical studies, ATL was used to alleviate dental anxiety and has been considered effective. However, the majority of studies used questionnaires to evaluate the degree of anxiety and to measure vital signs in both children and adults undergoing dental procedures.32, 33, 34, 35, 36
The mechanisms of AT are predicated on the activation of the sense of smell, which has significant effects on the body. The odorant inhalation acts on the olfactory pathway, extending from the nasal cavity to the olfactory bulb. The pathway sends impulses to the limbic system, which modulates the CNS and induces nerve-calming and mood-enhancing effects. Linalool is a main component of essential oils that are used as anxiolytic agents. They exhibit a dose-dependent impact on the CNS and interact with monoamine oxidase A (MAO-A), the serotonin transporter (SERT), GABA, and N-methyl-D-aspartate (NMDA) receptors.37 Also, linalool reduces the levels of catecholamines within the CNS and suppresses the activity of sympathetic nerves that innervate the adipose tissues and adrenal gland, modulating sympathetic nerve activity and blood pressure.38, 39, 40, 41, 42 In the current study, patients receiving ATL showed lower HR and RR levels compared to the ATS group. However, the AP values did not exhibit statistical differences between the groups. These results can be attributed to the normality in the parameters of AP or the dose-dependent effects of linalool.
Linalool has a wide range of physiological effects, including pain management.43, 44 For instance, it has been reported to diminish orofacial pain by activating inhibitory neurotransmission in the substantia gelatinosa of the trigeminal subnucleus caudalis.45 However, in the present study, patients receiving ATL or ATS did not demonstrate significant differences in pain evaluation. The observed outcomes may be related to the limited duration of follow-up, the measurement methodology, or the dose-dependent effects of linalool.
In addition, it has been reported that the administration of AT with aromatic essential oils containing linalool reduced cortisol levels in the saliva of healthy volunteers under conditions of standardized stress.10, 46
In the present study, patients receiving ATL presented lower cortisol levels compared to the ATS group, which could be related to a low level of anxiety in the ATL group. Likewise, only 1 clinical study with the ATL group measured cortisol levels in children after the administration of local anesthetics. The study noted a lower amount of cortisol in the intervention group compared to the control group.47
The United States Food and Drug Administration (FDA) has classified lavender as a safe substance.48 Products containing lavender are available on the market for the treatment of insomnia and anxiety. However, these products are offered as dietary supplements that do not require extensive pre-marketing approval from the FDA. Nonetheless, the administration of ATL in the waiting room of a dental office can be an easy and safe technique to reduce anxiety in patients.
Limitations
Numerous studies have noted that learning experiences of an aversive or traumatic nature are associated with stress-related problems and specific phobias.49 Also, dental anxiety and fear have been related to the dental traumatic story, cognition and perception.50 Therefore, one limitation of this study is the lack of analysis of cortisol levels, the association of MDAS with traumatic dental experiences, and patients’ educational level. Another limitation may be related to the environmental conditions of the study. The waiting room of a dental teaching clinic was consistently used at the same time of day, and the intervention was conducted over a short period (1 month), during which environmental conditions showed little variation and ambient temperature remained similar. However, in the present study, the volatile fraction of the compounds in lavender essential oil was not determined. Additionally, the target sample size of 90 individuals per group was not achieved. Nonetheless, a sample calculation proposed by Whitehead et al., based on a non-central t-distribution approach, indicated that 15 participants per group were sufficient for obtaining preliminary results.51
Conclusions
Aromatherapy with lavender may reduce HR, RT and cortisol levels in patients undergoing mandibular third molar surgery, presumably by alleviating anxiety. Future trials with adequate sample sizes that examine correlations among variables and compare ATL with other standard anxiety treatments may help generate more robust conclusions.
Trial registration
This parallel, triple-blind randomized clinical trial was registered at ClinicalTrials.gov in February 2020 (ID No. NCT04285385; https://clinicaltrials.gov/study/NCT04285385).
Ethics approval and consent to participate
The study was approved by the Bioethics Committee for Research, Faculty of Dentistry, Benito Juárez Autonomous University of Oaxaca (UABJO) (Oaxaca de Juárez, Mexico) in January 2020 (approval No. 19PEC001FO). All subjects provided written informed consent, and the intervention was conducted in accordance with the Declaration of Helsinki, including the current revisions, Good Clinical Practice guidelines, and the University Manual of Ethics Operations in Research (Benito Juárez Autonomous University of Oaxaca (UABJO)).
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.