Abstract
Background. Tooth loss significantly affects health and quality of life of older adults. Removable dentures are the most common solution for restoring oral function and aesthetics. In Poland, a significant portion of elderly population suffers from edentulism or partial tooth loss. However, not all of these individuals receive the prosthetic treatment they need. The measurement of unmet denture needs, defined as the proportion of individuals with tooth loss who lack appropriate dentures, offers critical insight into disparities in the access to oral healthcare.
Objectives. The aim of the study was to compare changes in unmet denture needs among Polish seniors over a decade and to assess patterns in denture use among those who received prosthetic treatment, taking into account sociodemographic factors such as sex, age, education, place of residence, and financial status.
Material and methods. The present study analyzed data from 2 nationally representative cross-sectional surveys, PolSenior (2009) and PolSenior2 (2019), comprising 4,712 and 4,075 participants aged ≥65 years, respectively. The individuals were categorized based on their dental status, denture use and sociodemographic characteristics. Unmet denture need was defined as the absence of complete or partial dentures among individuals with edentulism or partial tooth loss. The χ2 test and age standardization were implemented for the purpose of the statistical analysis. The level of significance was set at p < 0.05.
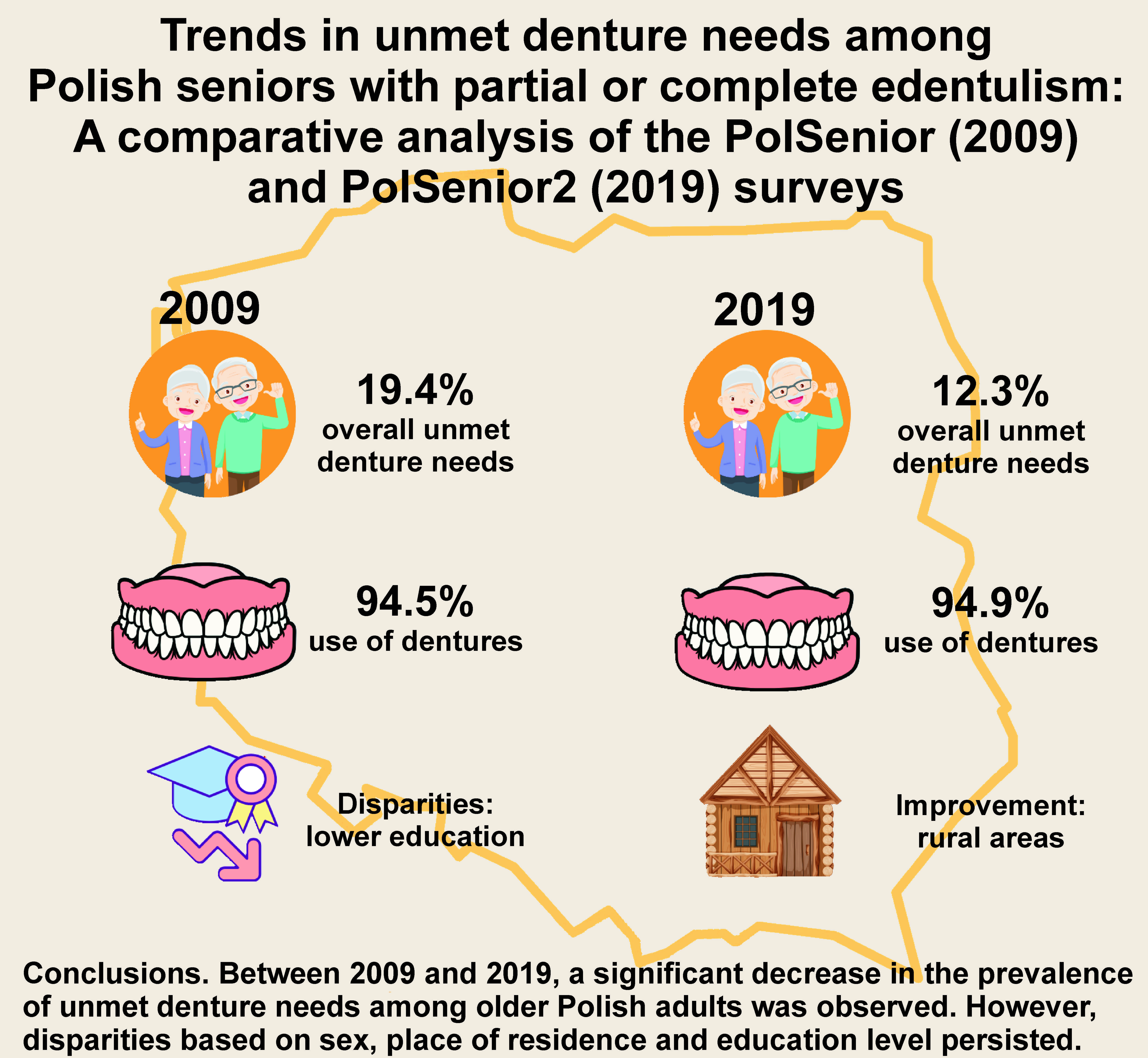
Results. The proportion of edentulous and partially dentate individuals without dentures decreased from 19.4% in 2009 to 12.3% in 2019. The most pronounced improvements were noted among women, urban residents and individuals aged 85 years and older. Despite these gains, disparities by sex, place of residence, education level, and financial status persisted. Among individuals who owned dentures, denture use remained consistently high in both survey waves, exceeding 94%, with no significant differences between the study periods.
Conclusions. The unmet need for dentures among Polish seniors has decreased over time, indicating an improvement in the accessibility to prosthetic care. However, sociodemographic disparities remain, highlighting the necessity for targeted public health strategies aimed at mitigating barriers to dental rehabilitation. The high rates of denture use confirm the enduring functional and psychosocial value of prosthetic treatment in older populations.
Keywords: dental health, dentures, demographic trends, geriatric dentistry, older adult population
Introduction
Tooth loss is a major public health concern among older adults, with far-reaching functional, nutritional, psychological, and social consequences. Globally, approx. 20% of the population over the age of 60 suffers from edentulism, often due to years of health neglect and limited access to dental care.1, 2
The loss of natural dentition significantly impairs masticatory function.3 Studies show that older adults without teeth often consume softer, processed foods, which can lead to digestive and nutrient absorption issues, increasing the risk of malnutrition and conditions such as cardiovascular disease, osteoporosis and metabolic disorders.4, 5
Beyond physical health, edentulism also affects psychosocial well-being. The condition leads to changes in facial structure, contributing to premature aging of facial features and lip collapse, as well as negatively impacting self-esteem and increasing the risk of social isolation.6, 7 These challenges are observed not only in low-resource settings but also in developed countries, where high treatment costs and the lack of comprehensive geriatric dental programs contribute to persistently high rates of edentulism.
In Europe, despite improvements in access to dental services, tooth loss remains prevalent among older populations, particularly in Eastern Europe, where edentulism rates exceed those observed in Western countries.8 In Poland, the 2019 PolSenior2 survey revealed that 36.1% of individuals over the age of 65 are completely edentulous, highlighting the severity of edentulism in Poland despite significant improvements over the past decade.9
Conventional dentures represent the most common and inexpensive solution for restoring lost teeth, allowing individuals to improve oral function, enhance phonetics, engage socially, and maintain an aesthetically acceptable appearance.10 Conventional dentures in this study refer exclusively to removable complete and partial dentures, not implant-supported or fixed prostheses. Dentures improve chewing ability, which is important for digestion and absorption of nutrients.11 Elderly individuals who wear dentures generally exhibit better nutritional status, as evidenced by higher body mass index (BMI) measurements.12 Notably, the Polish national healthcare system provides complete and partial dentures (for cases involving more than 5 missing teeth in a single arch) at no cost every 5 years, which likely contributes to the observed improvements in denture coverage and utilization rates.
The advantages of dentures extend beyond physical functionality, encompassing psychological and social dimensions. Studies have demonstrated that denture wearers participate more actively in social life, experience diminished feelings of loneliness and are at a reduced risk of depression.13, 14, 15, 16
The present cross-sectional study compares data from the PolSenior (2009) and PolSenior2 (2019) surveys to assess changes in the proportion of older adults (≥65 years of age) with unmet denture needs, as well as trends in denture use among those who received prosthetic treatment.
PolSenior was the first large-scale, multidisciplinary project in Poland dedicated to the study of aging, covering medical, psychological, functional, economic, and social aspects of the lives of older adults. A decade later, PolSenior2 continued this work, using a consistent methodology and introducing additional modules, including a focus on oral health. These studies offer a unique opportunity to assess trends in various domains of aging over time. The third edition of the project, PolSenior3, is currently underway and aims to further evaluate the evolving needs of the older population in Poland.
Material and methods
The study draws on data from 2 nationwide cross-sectional surveys: PolSenior (2009); and PolSenior2 (2019). Both projects aimed to assess the health status and socioeconomic conditions of Poland’s aging population. A particular emphasis was placed on oral health, including denture use, enabling a decade-long comparison of trends and disparities. The authors were not involved in the original data collection, but they obtained formal permission to use the datasets for comparative analysis.
Participants were divided into age cohorts, enabling precise comparisons across age groups. A balanced sex ratio was maintained in both studies, facilitating reliable comparisons between male and female subjects.
A three-stage, stratified, proportional random sampling method was implemented in both projects to ensure national representativeness. In the first stage, administrative units (rural, urban and mixed municipalities) were selected; in the second stage, specific streets or villages within the selected municipalities were chosen; and in the third stage, individual participants were randomly selected based on the national PESEL (Personal Identification Number) registry, which is managed by the Ministry of the Interior and Administration of Poland. To enable detailed subgroup analyses, oversampling of the oldest age groups was implemented.17, 18
The participants were classified based on their dental status as edentulous (no teeth), partially dentate (1–19 teeth), or functionally dentate (20 teeth or more). For the purpose of this study, functionally dentate individuals were excluded, as they typically do not require removable prosthetic treatment. The classification of dental status and prosthesis use was based exclusively on structured, self-reported questionnaire responses obtained during face-to-face interviews with trained fieldworkers. No clinical dental examinations were performed to verify the number of remaining natural teeth or the presence of dentures. The analysis focused on assessing both the unmet need for dentures and the actual use of complete and partial dentures among edentulous and partially dentate individuals.
The sociodemographic variables examined in relation to prosthetic needs and denture use included the following:
• age group (65–74; 75–84; ≥85 years);
• sex (female; male);
• education level (primary; vocational; secondary; higher);
• place of residence (rural; town with <50,000 residents; city with 50,000–200,000 residents; city with >200,000 residents);
• self-reported financial status (able to afford everything; can afford with saving; difficulties paying for food and clothing).
The final analytical sample comprised 4,712 participants aged 65+ from the PolSenior survey and 4,075 individuals from PolSenior2. The groups were harmonized to ensure comparability across the 2 time points.
Statistical analysis
The data collected in both studies was subjected to comparative analysis using descriptive statistics. The χ2 tests were applied to assess differences in unmet need for dentures between 2009 and 2019 using categorical variables, and age standardization was performed to account for demographic changes over the analyzed period. Statistical analyses were conducted using R software (v. 3.6.3; https://www.r-project.org) and SAS (v. 9.4; SAS, Cary, USA). The results were presented as percentages with 95% confidence intervals (CI). Sampling weights, which reflect the complex sampling design and post-stratification adjustments, were applied to align the sample distribution by age and sex with the Polish population in 2019. The significance level was set at p < 0.05.
Ethical considerations
Both studies were conducted in accordance with established ethical guidelines, and all participants provided written informed consent. The projects were approved by the Independent Bioethics Committee of the Medical University of Gdańsk, Poland (approval No. NKBBN/257/2017), ensuring compliance with local regulations and institutional requirements.17, 18
Results
Overall comparison of unmet denture needs in older adults (≥65 years)
A comparison of results from the PolSenior (2009) and PolSenior2 (2019) surveys revealed a statistically significant decrease in the prevalence of unmet denture needs among older adults in Poland. The proportion of edentulous and partially dentate individuals who do not use dentures decreased from 19.4% (95% CI: 16.4–22.5%) in 2009 to 12.3% (95% CI: 10.7–13.9%) in 2019, reflecting improved prosthetic service coverage (Table 1).
Unmet denture needs by sex
In both studies, female subjects consistently exhibited a lower level of unmet denture needs compared to male individuals. The proportion of women with unmet need for dentures decreased from 16.3% (95% CI: 12.5–20.0%) in 2009 to 8.1% (95% CI: 6.3–9.8%) in 2019. Among men, the unmet need declined from 24.4% (95% CI: 20.9–27.9%) to 19.2% (95% CI: 16.5–21.9%) over the same period (Table 1). Although improvement was observed in both sexes, the disparity between men and women remained.
Unmet denture needs by age group
A subsequent age-stratified analysis demonstrated a marked reduction in unmet denture needs, especially among older women. In the 65–74 age group of female subjects, the unmet need decreased from 14.3% (95% CI: 9.4–19.1%) to 6.4% (95% CI: 4.1–8.7%). In the 85+ group of women, the unmet need exhibited a decline from 25.3% (95% CI: 17.3–33.4%) to 10.2% (95% CI: 7.3–13.2%). Among men, a decrease was noted in each age group; however, these changes did not reach statistical significance (Table 1).
Unmet denture needs by place of residence
Across both time points, urban residents exhibited a consistently lower prevalence of unmet denture needs compared to their rural counterparts. In rural areas, the proportion of women without dentures decreased from 22.7% (95% CI: 15.0–30.3%) in 2009 to 11.3% (95% CI: 8.1–14.5%) in 2019, while the proportion of male subjects with unmet denture needs declined from 35.9% (95% CI: 30.5–41.2%) to 24.6% (95% CI: 20.2–29.0%). In small urban centers (<50,000 residents), the unmet need among women decreased from 12.4% (95% CI: 8.8–16.0%) to 5.3% (95% CI: 3.2–7.5%) (Table 1).
Unmet denture needs by education level
Lower levels of education were associated with higher unmet denture needs in both survey waves. Among individuals with a primary education, the unmet need remained relatively high, while the lowest levels were observed among those with a higher education. Despite an observed downward trend across all education levels between 2009 and 2019, the differences did not reach statistical significance (Table 1). The association was particularly notable among men, where educational disparities were more pronounced.
Unmet denture needs by financial situation
A significant improvement in denture access was observed among respondents who reported being able to make purchases when saving. In this group, the unmet need for dentures decreased from 17.5% (95% CI: 13.7–21.3%) in 2009 to 11.6% (95% CI: 9.5–13.7%) in 2019. Financial disparities were evident in the PolSenior2 survey. Individuals who reported they can afford everything had an unmet need of 8.8% (95% CI: 6.1–11.5%), while those with difficulties paying for food and clothing had a significantly higher unmet need of 15.2% (95% CI: 12.1–18.2%) (Table 2).
Unmet needs for partial dentures
Among individuals with partial tooth loss (1–19 teeth), the prevalence of unmet need for partial dentures decreased significantly from 25.0% (95% CI: 19.6–30.3%) in 2009 to 16.0% (95% CI: 13.6–18.5%) in 2019 (Table 3).
The most substantial improvement was observed among women, where the unmet needs declined from 20.6% (95% CI: 14.3–26.8%) to 10.5% (95% CI: 7.9–13.1%).
In PolSenior2, financial status was significantly associated with unmet denture needs. Among those who reported they can afford everything, the unmet need for partial dentures was 10.7% (95% CI: 6.8–14.6%), compared to 20.8% (95% CI: 15.9–25.7%) among individuals who experienced difficulties paying for food and clothing.
Unmet needs for complete dentures
In the edentulous group (0 teeth), the proportion of individuals without complete dentures decreased significantly from 11.4% (95% CI: 9.0–13.8%) in 2009 to 7.2% (95% CI: 5.4–9.0%) in 2019 (Table 3).
Among women, the unmet needs declined from 10.4% (95% CI: 7.7–13.2%) to 5.2% (95% CI: 3.0–7.5%), with the most pronounced improvement observed in the 85+ age group, where the rate fell from 18.1% (95% CI: 12.3–23.9%) in 2009 to 7.1% (95% CI: 3.7–10.4%) in 2019.
Denture use among denture wearers
Denture use among Polish older adults, as presented in Table 4, remained consistently high over the analyzed decade, with no statistically significant differences observed between the PolSenior (2009) and PolSenior2 (2019) surveys. The overall utilization rates were 94.5% (95% CI: 93.3–95.7%) in 2009 and 94.9% (95% CI: 93.9–95.8%) in 2019, highlighting the widespread use of dentures across diverse demographic groups and socioeconomic conditions. Both surveys revealed very high usage rates for complete and partial dentures, with complete dentures being used slightly more frequently than partial ones in most subgroups.
Sex differences
Overall denture use was consistently higher among women than men. In 2019, 95.8% (95% CI: 94.9–96.7%) of women reported regular denture use, compared to 93.1% (95% CI: 91.0–95.2%) of men. This discrepancy in outcomes was observed across both complete and partial dentures, and persisted across various demographic groups, including age, education and place of residence (Table 4).
Influence of education
Denture use increased along with education levels. Significant differences were noted between individuals with a primary education and those with a higher education. In 2019, the denture utilization rate among women with a higher education reached 96.4% (95% CI: 93.0–99.8%) compared to 93.5% (95% CI: 91.5–95.5%) for those with a primary education only. Among the male population, the corresponding values were 96.0% (95% CI: 93.3–98.8%) for those with a higher education compared to 91.8% (95% CI: 88.0–95.6%) for those with a primary education (Table 4).
Urban–rural differences
Higher denture use was observed in larger urban areas compared to rural regions. In 2009, denture utilization in rural areas was 92.8% (95% CI: 89.7–95.9%) among women, compared to 98.8% (95% CI: 98.1–99.4%) in cities with populations exceeding 200,000. A similar trend was observed in the male population and in both PolSenior surveys. This pattern was consistent across both complete and partial dentures (Table 4).
Age-related trends
Denture use declined with advancing age. In 2019, the use of dentures among individuals aged 65–74 years reached 97.4% (95% CI: 96.2–98.6%) for women and 93.1% (95% CI: 90.2–96.1%) for men. In the 85+ group, the prevalence of denture use decreased to 91.0% (95% CI: 87.8–94.1%) among women and to 90.9% (95% CI: 86.6–95.2%) among men. The most pronounced decline was observed for partial dentures in the oldest age group (85+). In 2019, the use of partial dentures was 83.4% (95% CI: 75.6–91.2%) among women and 87.5% (95% CI: 80.7–94.4%) among men.
Financial factors
The PolSenior2 survey revealed that there were no significant differences in denture use between individuals with different financial statuses. However, the results of the PolSenior survey noted a statistically significant difference among edentulous individuals. Participants who reported having sufficient financial resources exhibited a denture utilization rate of 98.8% (95% CI: 97.6–100.0%), compared to 93.6% (95% CI: 91.0–96.1%) observed among those encountering difficulties paying for food and clothing (Table 2).
Complete vs. partial denture usage
Complete dentures demonstrated slightly higher utilization rates compared to partial dentures across all demographic categories. For instance, complete denture use in 2019 was 96.1% (95% CI: 95.0–97.2%) compared to 93.9% (95% CI: 92.4–95.3%) for partial dentures (Table 4).
Discussion
The observed decrease in unmet denture needs among Polish seniors — from 19.4% in 2009 to 12.3% in 2019 — indicates notable improvements in access to dental prosthetic care over the past decade. This growth is likely the result of multiple factors, including expanded access to affordable dental care, increased awareness of the importance of oral health among older adults, and health policies that integrate oral care into comprehensive eldercare.
The consistently high rates of denture use observed in both surveys (>94%) among denture wearers confirm that prosthetic treatment is widely used and valued once obtained. This outcome is indicative of the efficacy and acceptability of prosthetic appliances, underscoring the importance of maintaining high standards of fabrication, clinical follow-up and patient education.19
The observed trend in Poland aligns with global improvements in senior dental health, where greater access to dental services and oral health education has led to better outcomes for aging populations. In many countries, the implementation of dental subsidies and public education initiatives have increased the accessibility to dental prosthetics, improving seniors’ quality of life by preserving oral functionality and aesthetics. The Polish data offers further insight into these global trends and underscores the impact of systemic support in promoting oral health equity among the elderly population. Previous comparative analyses using the Survey of Health, Ageing and Retirement in Europe (SHARE) dataset have identified Poland, Germany, Austria, Ireland, Belgium, and the Netherlands as countries with similarly elevated rates of prosthetic rehabilitation among older adults.20, 21
In contrast, Scandinavian and Southern European countries, such as Sweden, Greece, France, and Italy, report lower rates of denture usage. A study from Norway illustrates substantial regional disparities within a national context. In Oslo and adjacent counties, the majority of older adults retained their natural teeth, while in northern regions, 65.7% of seniors relied exclusively on complete dentures.22
Expanding beyond the European context, recent research from Asia and the Middle East reinforces the global variability in denture wearing patterns. Yuan et al. reported that 67.1% of urban edentulous seniors in China wore dentures, compared to only 51.1% in rural areas.23 This urban–rural disparity was primarily driven by differences in education, income, chronic disease burden, and health behavior, especially physical activity.23
In Jordan, Mukatash Nimri and Jebreen found that rural elderly individuals exhibited significantly higher needs for denture replacement compared to their urban counterparts (69.5% vs. 31.6%, respectively). Moreover, nearly half of the rural elderly (47%) reported dissatisfaction with denture fit or function.24 These patterns highlight persistent gaps in prosthetic care access and maintenance, particularly in under-resourced regions.24
Taken together, these international comparisons underscore that denture wearing among older adults is influenced not only by clinical need (e.g., edentulism), but also by systemic and sociocultural factors. Poland’s high denture prevalence is consistent with global patterns observed in countries with similar socioeconomic and healthcare structures, thereby reinforcing the need for integrated prosthetic and preventive care strategies that are context-sensitive and equity-focused.
In the present study, a notable and persistent sex disparity was observed, with women consistently exhibiting lower unmet denture needs than men. This phenomenon may be attributed to sex differences in health-seeking behaviors and perceptions of self-care.25, 26 Additionally, societal expectations regarding appearance and the impact of tooth loss on facial aesthetics may make dentures more appealing for women. Previous studies have highlighted the psychosocial benefits of denture use, particularly in relation to self-image and quality of life.13, 27
In 2009, the unmet denture needs were highest among the oldest age group (85+), likely due to a combination of the following factors: limited historical access to dental care; lower health literacy; and physical barriers such as mobility issues. However, by 2019, these disparities substantially narrowed. The unmet needs among the oldest individuals sharply declined, especially among women. This shift may partly reflect cohort turnover, as individuals who had already received dentures in middle age transitioned into older age groups while continuing to use them.
The age-related improvement in the use of dentures over recent decades suggests an increase in both awareness and service availability. Nevertheless, the utilization of existing dentures exhibited a slight decline with advancing age, which is likely influenced by reduced social activity, general frailty and physical limitations associated with wearing and maintaining dentures.
A persistent urban–rural gap remains evident. Seniors living in rural areas consistently exhibited higher unmet denture needs compared to those from cities. This disparity may be attributed to the limited number of dental clinics in rural areas, which results in reduced accessibility to dental services. For elderly individuals with mobility challenges, the lack of support from close relatives or limited transportation options to urban centers further exacerbates the difficulty of accessing dental care. Consequently, many individuals forgo acquiring dentures due to significant logistical barriers.28, 29 Moreover, the lifestyle in rural areas differs from that in cities. Social pressure related to appearance is often less pronounced in rural settings, potentially diminishing the motivation of individuals with missing teeth to seek prosthetic solutions.
Despite these barriers, rural regions witnessed substantial progress between 2009 and 2019, marked by an approx. 11% reduction in the prevalence of unmet denture needs among both women and men. However, urban populations continue to demonstrate superior outcomes.
Education level was strongly associated with prosthetic coverage. Seniors with higher education had significantly lower unmet denture needs. This trend reflects greater awareness of oral health and a better understanding of the consequences of tooth loss among individuals with higher education. Education level has also been demonstrated to correlate with financial stability and higher retirement benefits, which facilitate better access to dental care.30, 31 These findings underscore the critical role of education in promoting oral health and suggest that public health initiatives should prioritize oral health education, with a particular emphasis on populations with lower levels of educational attainment.
Financial status has a significant influence on the decision to undergo dental prosthesis treatment. This phenomenon was particularly evident in the 2019 study, which revealed that the replacement of missing teeth was considerably more prevalent among the most financially stable seniors compared to those in the most challenging economic situations. The national healthcare system in Poland provides reimbursement for complete dentures for edentulous individuals, which likely explains why no statistically significant differences were observed in denture coverage among edentulous individuals across different financial groups in both the PolSenior and PolSenior2 studies.
However, partial dentures are only reimbursed for individuals with more than 5 missing teeth per jaw. This limitation may be a key factor contributing to the observed differences in denture coverage among partially edentulous individuals with varying financial statuses. The findings highlight the potential need for extending public reimbursement policies to include partially dentate individuals, which could help reduce financial barriers and improve access to dental prosthetics for a broader segment of the aging population.
Additionally, differences in denture use among individuals with varying financial backgrounds may be influenced by factors that extend beyond affordability, such as varying degrees of awareness, social engagement and overall lifestyle. Seniors in better financial situation may have greater access to dental care follow-ups, adjustments and maintenance, which can result in higher rates of denture use. These results emphasize the importance of considering socioeconomic factors when designing policies aimed at enhancing oral health care accessibility and utilization among aging populations.
Limitations
The present study relies on self-reported data, which may be subject to recall bias or reporting inaccuracies. Additionally, while the comparison between PolSenior and PolSenior2 offers valuable insights into trends in unmet denture needs, it does not reflect more recent developments in dental service accessibility or account for policy changes introduced after 2019. Future studies could benefit from the collection of longitudinal data and the inclusion of qualitative insights to better understand the individual motivations and barriers associated with denture coverage.
Conclusions
A comparative analysis of the PolSenior and PolSenior2 surveys demonstrated a significant reduction in unmet denture needs among older Polish adults over a 10-year period. This decline can be attributed to improved access to dental care and increased awareness of the significance of oral health within this population. The study highlights ongoing disparities in prosthetic coverage based on sex, age, place of residence, and education level, indicating areas where public health interventions could be further optimized. Enhancing access to dental care, especially in rural regions and among individuals with limited educational attainment, remains crucial. The high rates of denture utilization documented in both surveys suggest that these devices effectively address the functional and aesthetic needs of older adults. However, the observed decline in utilization among the oldest age groups highlights the need for additional support, such as tailored education on proper denture maintenance and increased access to follow-up dental care. It is imperative that ongoing research be conducted to monitor these trends and identify any additional factors that can further enhance the quality of life and well-being of Poland’s aging population.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.