Abstract
Background. As per the Centers for Disease Control and Prevention (CDC) guidelines, dentists must avoid the aerosol-generating procedures during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic.
Objectives. This study aimed to compare the rate of bracket bond failure with the aerosol-generating and non-aerosol generating bonding techniques.
Material and methods. A retrospective cohort study was conducted during the SARS-CoV-2 pandemic on a sample of 44 patients (880 teeth), equally divided into 2 groups: the conventional aerosol-generating bonding technique (ABT); and the novel non-aerosol-generating bonding technique (NABT). The rate of bracket survival and total number of bracket breakages in the 2 groups were assessed by means of the survival regression analysis. The influence of pre-treatment factors, such as the sagittal jaw relationship (ANB), the Frankfort–mandibular plane angle (FMA), overjet, overbite, and upper and lower crowding, on the rate of bracket survival was also evaluated.
Results. There was a statistically significant difference between ABT and NABT in terms of bracket survival. The mean bracket survival with ABT was 176.21 ±77.89 days and with NABT it was 162.53 ±83.34 days. The novel technique showed a hazard ratio of bracket survival of 2.99 as compared to the conventional method. There was a statistically significant influence of overjet on the rate of bracket survival (p = 0.010). The posterior segment had a higher rate of bracket failure as compared to the anterior segment in NABT, which was statistically significant (p < 0.001). However, this difference was statistically non-significant in the case of ABT.
Conclusions. There was an increased rate of bracket failure with NABT as compared to ABT. The rate of bracket breakages in the anterior quadrants was comparable for both bonding techniques.
Keywords: bracket bonding, SARS-CoV-2, orthodontic treatment
Introduction
On March 11, 2020, the World Health Organization (WHO) officially declared coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) a pandemic.1 The rapid spread of the SARS-CoV-2 viral web is still unpredictable. It is known that COVID-19 is an airborne infection, transmitted by the infected person through droplets and fomites.2 SARS-CoV-2 directly influences the nasal and oral epithelium, which results in 95% impairment of taste sensations at the onset of the disease.3 SARS-CoV-2 mainly attacks angiotensin-converting enzyme 2 (ACE2) receptors, which are mostly present in the salivary glands.4 The inflammatory response evoked by this infection also leads to severe dryness of the mouth.5 Hence, SARS-CoV-2 is not only transmitted by salivary droplets, but saliva is now used for the detection of the virus.6
Healthcare professionals, especially dentists, are at higher risk of being directly exposed to the virus due to the inhalation of aerosols and droplets, along with indirect transmission via the contaminated surfaces or by asymptomatic infected patients.5 Healthcare facilities are now highly focused on insuring an environment of strict infection control for patients as well as staff members.7 Initially, all elective hospital procedures were suspended to minimize the spread of SARS-CoV2.8 Routine dental treatment as well as the delivery of orthodontic services were rapidly restricted to only emergency procedures to limit the unwanted risk of exposure.9
The WHO promptly presented precise guidelines for emergencies as well as elective dental procedures in order to continue providing patients with healthcare in the infection-controlled environment.10 As per the Centers for Disease Control and Prevention (CDC) recommendations, dental surgeons as well as orthodontists should limit the aerosol-generating procedures by minimizing the use of high-speed air turbines, ultrasonic scalers or triple syringes.11 If deemed necessary, all the aerosol-generating procedures should be performed while wearing the appropriate personal protective equipment (PPE).12
The British Orthodontic Society (BOS), however, classified orthodontic procedures as non-aerosol-generating ones except for the bonding of brackets, the placing of a fixed retainer and the debonding of brackets.13 On the contrary, the American Association of Orthodontists (AAO) claims that orthodontists can use slow-speed handpieces and ultrasonic scalers on a completely dry field and in negative pressure operating rooms with high-volume suction.10, 13 In a study conducted by Golshah et al., high-volume suction reduced the aerosol particles generated during dental procedures by 44%.14 However, this study examined only the dust particles produced during the aerosol-generating procedures, and not airborne droplets.10, 11, 12, 13
It is considered that the laser-assisted procedures, i.e., laser etching, can be regarded as non-aerosol-generating procedures. However, laser etching does not preclude aerosol generating, as it requires water spray as a coolant after etching.14 Therefore, the rationale of the present study is an urgent need for strict recommendations as to limiting orthodontic procedures to the provision of basic care to patients. Hence, the non-aerosol-generating bracket bonding protocol should be promptly developed. This study aimed to evaluate the rate of bracket breakages with the novel non-aerosol-generating bonding procedure. The secondary objective of this study was to compare the conventional aerosol-generating and novel non-aerosol-generating bonding procedures in terms of bracket breakage. The null hypothesis of this study was that there is no difference in the rate of bracket breakages with the use of the aerosol-generating and the non-aerosol-generating bonding techniques.
Material and methods
A retrospective cohort study was conducted at the Aga Khan University Hospital in Karachi, Pakistan, after obtaining an approval from the institutional Ethics Review Committee (ERC No. 2021-6233-17837). The orthodontic records of bracket breakages among the adult patients who had reported for the initiation of treatment at a tertiary-care hospital were obtained. The sample size was calculated with the OpenEpi (3.0) sample size calculator (https://www.openepi.com), based on the findings of Hegarty and Macfarlane, who reported a bond failure percentage of 30% and a risk ratio of 2.6 (1.7, 3.9) for a resin-based composite.15 Keeping the level of significance (α) at 5% and a power of study (1-β) of 80%, at least 22 subjects were required in each group with an inflation of 10%. Hence, we included 44 patients and the analysis was done on a total of 880 teeth. Patients above 18 years of age who reported to the orthodontic clinic and initiated fixed orthodontic treatment were included in the study. Those having any syndromes, asymmetries, cross-bites, cleft lip and palate, centric occlusion–centric relation (CO–CR) discrepancy, or with a previous history of orthodontic treatment were excluded from the study.
All the included patients had their brackets bonded for the duration from March 2020 till 2021. The data was collected in April 2021. All patients were given an option of getting the polymerase chain reaction (PCR) COVID-19 testing so that the bonding of brackets by means of the conventional aerosol-generating bonding technique (ABT) (as per the Buonocore protocol16) could be carried out. This had to be performed under strict infection control conditions to scrutinize symptomatic and asymptomatic patients. We included all those patients who opted for a PCR test as control; however, patients who refused to get tested via a PCR test were bonded by applying the non-aerosol-generating bonding technique (NABT) as described below and were considered the experimental group.
This novel technique comprised the following steps:
– the tooth surface was cleaned by manual scaling and polished by rubbing with raw pumice on a rubber cup manually instead of using a slow-speed handpiece, an ultrasonic scaler or a triple syringe;
– the enamel surface was etched with 37% phosphoric acid for 15 s, as per the Buonocore protocol16;
– the etchant was carefully removed from the tooth surface with a cotton roll, preventing damage to the gingiva. Residual acid was removed by cleaning the tooth surface with a damp gauze swab 3 times (each time with a new gauze swab) instead of using high-volume air water pressure from a triple syringe;
– the frosty white surface of enamel was then achieved by high-volume negative pressure suction and tap drying the tooth surface with a gauze swab;
– the primer was then applied on the dried tooth surface and an orthodontic bracket was bonded on the tooth surface with a light-cured composite.
There were 440 teeth in the experimental and 440 teeth in the control group, equally distributed. All patients in the sample were directly bonded with the Roth bracket prescription, a 0.022-inch slot (3M Unitek™; 3M, St. Paul, USA). Leveling and alignment were achieved using round NiTi archwires initially, which were later progressed to 0.018-inch stainless steel (SS) wires during the space closure and molar correction stage. The patients were instructed to maintain oral hygiene, avoid bracket breakages and maintain punctuality with regard to appointments. The teeth were rebonded as soon as the patients reported to the clinic with breakages.
To eliminate any risk of selection bias, all patients with enamel surface defects, missing teeth, early extractions, prematurely debonded or undergoing single-arch treatment, and those noted to be non-compliant were excluded from our study sample.
Other variables, such as the sagittal jaw relationship (ANB), the vertical divergence pattern (SN–GoGn), the lower incisor to the mandibular plane angle (IMPA), and the upper incisor to sella–nasion plane angle (UI–SN) were cephalometrically analyzed; overjet (OJ), overbite (OB), cross-bites, crowding or spacing, and buccal relationships were measured on plaster models with the Mitutoyo multifunctional Vernier caliper (Mitutoyo, Kawasaki, Tokyo).
Statistical analysis
The data was analyzed using the IBM SPSS Statistics for Windows software, v. 23.0 (IBM Corp., Armonk, USA), and Stata, v. 12.0 (StataCorp, College Station, USA). The Shapiro–Wilk test showed a normal distribution of the data. Descriptive statistics for continuous variables were reported as mean and standard deviation (M ±SD). The probability of bracket survival and the factors influencing bracket bond failure in both bonding techniques were evaluated by applying the survival regression analysis. The comparison of the rate of bracket breakages with the use of ABT and NABT was performed by means of the regression analysis.
Results
Demographics
The analysis of descriptive statistics showed an almost equal gender distribution in the ABT and NABT groups. The mean age of the participants was 26.22 ±9.51 years and it was comparable in both groups (Table 1).
Bonding technique
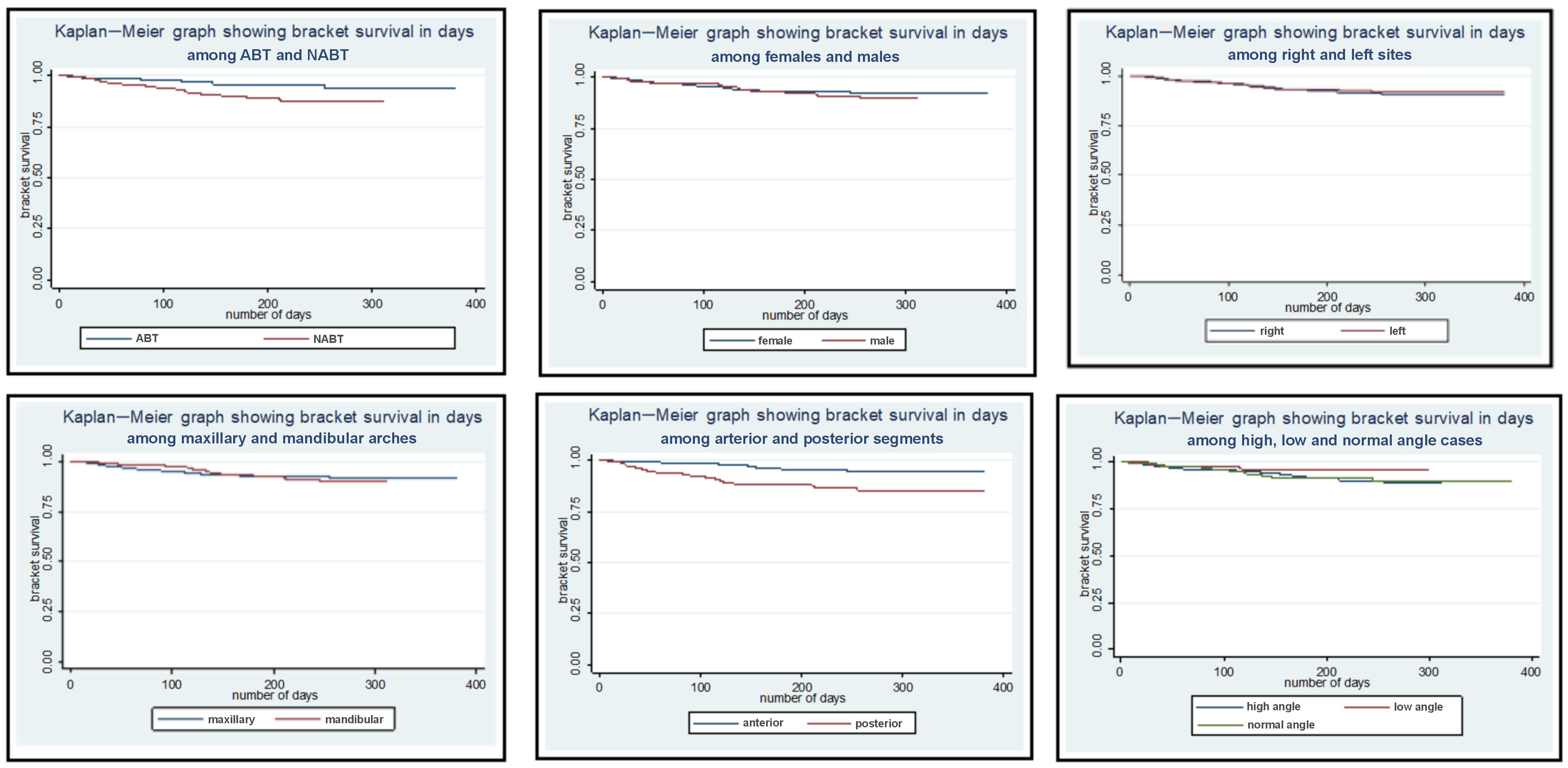
Comparing the 2 bonding techniques, we found that the brackets bonded by means of the conventional technique survived for a mean duration of 176.21 ±77.89 days, with a maximum survival rate of 179.54 days for right upper lateral incisors and first premolars, and for left upper cental and lateral incisors and first premolars. However, the brackets bonded by means of NABT survived for a mean duration of 162.53 ±83.34 days, with a maximum survival of right upper central incisors for 180.27 days (Table 2). These results were also confirmed with the Kaplan–Meier analysis; in the graph, the blue and the red lines indicate ABT and NABT, respectively (Figure 1). Establishing ABT as a reference in the regression analysis, we found that there was a statistically significant difference in the rate of bracket breakages between the 2 bonding techniques (p < 0.001) (Table 3).
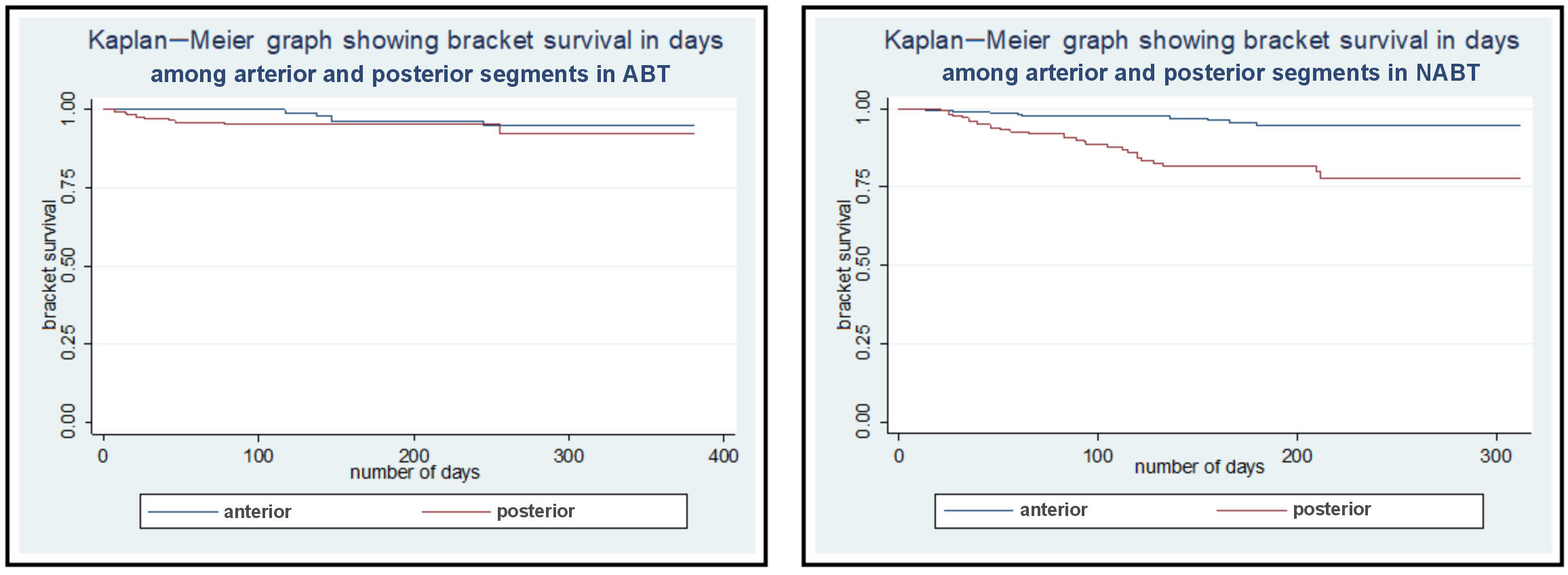
Furthermore, there was a statistically significant difference in the rate of bracket breakages between the anterior and posterior segments (p < 0.001). Hence, we assessed the difference between both the segments separately with ABT and NABT. We found that with ABT, the difference in the rate of bracket breakages between the anterior and posterior segments was statistically non-significant; however, there was a highly statistically significant difference in the rate of bracket breakages between the segments with NABT (p < 0.001) (Table 4).
Cephalometric skeletal variables
The regression analysis revealed that there was a statistically non-significant difference in the rate of bracket breakages with regard to the sagittal jaw relationships in both groups (p = 0.170) (Table 3). We also found that in the case of the normodivergent pattern, bracket survival was greater as compared to the hypodivergent and hyperdivergent patterns, as shown in the Kaplan–Meier graph in Figure 1. However, this difference was statistically non-significant, which indicates that angular values did not influence the duration of bracket survival in any group.
Dentoalveolar variables
Furthermore, we found that with an increase in overjet by 1 mm increased the risk of bracket breakage 1.08 times. Overbite, and upper and lower crowding influenced the rate of bracket breakages insignificantly (Table 3). The rate of bracket breakages was comparable between the right and left sites, with a mean survival of 164.27 ±83.07 days and 161.74 ±83.66 days, respectively, with the NABT technique (Table 2). Establishing the maxillary arch as a reference, we found no statistically significant difference in the rate of bracket breakages between the maxillary and mandibular arches, which is also depicted in the Kaplan–Meier graph in Figure 1; this difference proved to be statistically non-significant in the regression model (Table 5).
Discussion
During the initial months of facing the SARS-CoV-2 pandemic situation, our institution commenced orthodontic bracket bonding by means of NABT. It was required to minimize the risk of spreading the infection through the salivary splatters produced during the conventional bonding of orthodontic brackets. In the present study, the brackets bonded with ABT survived for a mean duration of 176.21 ±77.89 days; however, the brackets bonded with NABT survived for an average of 162.53 ±83.34 days. Apparently, these results lead to the inference that NABT compromised bracket bond strength when compared to the conventional technique. However, we found that there was a statistically non-significant difference in the rate of bracket breakages in the posterior segment with conventional ABT and a highly statistically significant difference with NABT as compared to the anterior segment. This clarifies that in NABT, the posterior segment is the area with a significantly increased rate of bracket breakages. The difference in bracket bond survival in the anterior and posterior segments has also been reported with the use of other techniques related to bracket bonding. While comparing the rate of bracket failure with the use of light-emitting diodes and halogen etching, Krishnaswamy and Sunitha found a difference between the anterior and posterior segments.17 It has been suggested that the compromised bracket bond strength in the posterior segment is due to an increased risk of salivary contamination and the reduced access to this area.17, 18, 19, 20, 21 The difference in bond failure rate between the 2 bonding techniques observed in our study could also be due to the lack of experience of dental auxiliary staff in bonding orthodontic brackets with the use of NABT. To insure the quality of treatment, the abovementioned standardized NABT was applied in all the patients from the experimental group. It is because of the effort in standardization that in the anterior region, the results obtained with NABT were comparable to those achieved with the conventional bonding procedure.
It is a perceived fact that self-etching bonding and laser etching would minimize the production of aerosol during orthodontic bonding.22, 23, 24, 25, 26 As reported by Contreras-Bulnes et al., there was a comparable mean duration of bracket survival with the use of self-etching bonding and NABT.26 For laser etching, they obtained similar results as in the case of the conventional bonding technique.26 Self-etching as well as laser-etching bonding techniques do not provide superior results as compared to NABT, as described in our study, and the use of a self-etching system does not preclude the use of a triple syringe, which can lead to developing saliva splatters. Similarly, laser requires water spray as a coolant, which is yet another way of increasing the production of salivary droplets.
It is quite clear from our results that the effectiveness of NABT and ABT for bonding in the anterior segment is comparable. The difference in the rate of bracket bond failure is observable in the posterior segment; the rate may be greater for NABT than for the conventional procedure, but it is still clinically acceptable (Figure 2) and is of considerable utility when opting for alternative treatment methods during a pandemic situation. According to Skidmore et al., each bracket breakage increases the duration of treatment by 0.6 months.27 Considering this fact, each bracket breakage after every 162 days, would consequently increase the duration of treatment by 0.6 months. This slight delay in treatment can be accepted in contrast to an increased risk of spreading the infection through the production of aerosol, which may lead to an increased rate of mortality in this pandemic situation.
To the best of our knowledge based on a literature search, we were unable to find any study on a bracket bonding protocol entirely with the use of NABT. The non-aerosol-generating bonding technique is an urgent clinical requirement in the present pandemic situation, with the risk of spreading the infection by undiagnosed and asymptomatic patients being increased by 87%.28 The recommendation of this study is that NABT should be strictly followed in all orthodontic setups during the SARS-CoV-2 pandemic instead of suspending all clinical practices.
Limitations
Apart from the reduced survival of the brackets with NABT, the effect on the quality of enamel, and other pros and cons of this treatment modality need further evaluation with research. Long-term follow-up studies must be conducted to validate the clinical utility of NABT. Since this was a single-center study with a short follow-up period, further studies using this alternative bonding technique need to be conducted in other setups. Another limitation of this study is that the sample was collected in a stressful pandemic situation, which may have increased parafunctional habits (bruxism), leading to an increased risk of bracket breakages. The strength of this study is that 880 teeth were considered for analysis and this large number of teeth validates our study findings.
Conclusions
Through our study on the novel non-aerosol-generating bonding technique (NABT), we found that bracket survival with the use of this technique was 162.53 ±83.34 days as compared to the 176.21 ±77.89 days achieved with the conventional bonding technique. The bonding of brackets in the anterior segment was comparable for both bonding techniques; however, there was an increased rate of bracket breakages in the posterior segment with the use of NABT.
Ethics approval and consent to participate
This study was approved by the Ethics Review Committee at the Aga Khan University Hospital in Karachi, Pakistan (ERC No. 2021-6233-17837).
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author and the co-investigators on reasonable request.
Consent for publication
Not applicable.