Abstract
Background. Hyaluronic acid (HA) is a naturally occurring linear polymer with a large molecular size and a simple structure. It is classified as a glycosaminoglycan (GAG), which is a critical element of the extracellular matrix (ECM). Notably hydrophilic, HA has unique qualities such as viscoelasticity, biodegradability and biocompatibility. Its molecular weight (MW) has an influence on its activity, resulting in a wide spectrum of potential effects. Hyaluronic acid and its derivatives are biomaterials with great potential for usage in the medical, dental, pharmaceutical, and cosmetic industries.
Objectives. The aim of the study was to assess the impact of HA on the stomatognathic function of the temporomandibular joint (TMJ).
Material and methods. A meta-analysis was conducted, contrasting HA with alternative TMJ injectable materials, and a review of the literature based on PubMed® publications was carried out.
Results. Hyaluronic acid is considered a safe and effective injectable material for the treatment of TMJ disorders. While HA has shown positive results in clinical applications, it is important to note that other injectable materials may prove equally or more effective, depending on the specific condition and the patient’s needs. These alternative materials are being explored to identify the most suitable treatment option for TMJ disorders.
Conclusions. In individuals with TMJ pain and dysfunction, HA has shown safety and effectiveness in reducing pain and enhancing the maximum mouth opening (MMO). However, when compared to platelet-rich plasma (PRP), HA has demonstrated superior long-term results.
Keywords: temporomandibular joint, filling material, hyaluronic acid
Introduction
Hyaluronic acid (HA) is a natural and unbranched member of the glycosaminoglycan (GAG) group, which is mostly composed of extracellular matrix (ECM) components. Hyaluronic acid is distinguished from other GAGs due to its large molecular size and a simple structure.1
The essential structural elements common to all GAGs are the disaccharide units of an amino sugar and a uronic sugar. However, HA is the only GAG that is not bonded to a core protein and does not undergo postsynthetic modifications. Additionally, it is not produced by Golgi enzymes or sulfated.2 The main structure of HA is composed of a naturally occurring linear polymer with miles of repeating disaccharide units. Each disaccharide is made up of d-glucuronic acid and N-acetyl-D-glucosamine joined by ß-1,4- and ß-1,3-glycosidic linkages in alternating sequences.1, 2, 3
Certain enzymes, known as HA synthetases (HAS), are responsible for the synthesis of HA on the inner surface of cell membranes.3 The human body breaks down HA through various mechanisms. Hyaluronic acid found in blood is broken down systemically in the liver and lymph nodes, while HA present in tissues is broken down extracellularly by reactive oxygen species (ROS) and hyaluronidase enzymes. The molecule regenerates quickly, and its half-life ranges from 12 h to 24 h in the epidermis to a few minutes in the bloodstream. This observation suggests a continuous cycle of synthesis and degradation of this polymer.3, 4
Hyaluronan with a high molecular weight (HMW-HA) is the original long polymer form of HA. It can be broken down into low molecular weight hyaluronan (LMW-HA) components.1 Both HMW-HA and LMW-HA can exhibit opposing biological actions.2
While LMW-HA is a strong pro-inflammatory molecule that promotes angiogenesis and tissue remodeling throughout the healing process, as well as demonstrates antiapoptotic and immunostimulating activities, HMW-HA has been observed to possess immunosuppressive, antiangiogenic and anti-inflammatory properties.1, 5
The hydrophilic groups on the HA molecule interact with water molecules as well as one another to form hydrogen bonds, contributing to the high solubility and hydrophilicity of HA.6 Hyaluronic acid is negatively charged, extremely hydrophilic, and produces a red viscose at HMW due to the carboxyl groups present in the molecule.4 This network is reliant on molecular weight (MW) and HA concentration, since HA networks become stronger and HA solutions exhibit gradually increased viscosity and viscoelasticity with increasing MW and HA concentration. Hyaluronic acid is negatively charged in an aqueous solution and forms highly hydrophilic cells known as hyaluronan or hyaluronate.2 Due to its viscoelastic properties, HA can enter tissues with ease and occupy significant amounts of extracellular space. It is a remarkable biomaterial filler, exhibiting a high degree of malleability. The hallmarks of HA solutions include shear thinning, viscoelastic behavior and non-Newtonian behavior. Moreover, HA solutions are not thixotropic; rather, they return to their original viscosity and structure once the shear rate ends. Hyaluronan’s distinct rheological behavior is uncommon and crucial since it affects numerous physiological processes as well as the drug, food, medicine, and cosmetic uses of the substance.2
Owing to its physicochemical characteristics, HA controls tissue homeostasis, hydration of ECM, and resistance to compression pressures. Numerous proteoglycans interact with HA to produce chemical compounds that stabilize the structure of ECM and maintain the matrix’s gel state.4
Consequently, these polymers can serve as shock absorbers by withstanding compressive pressures on the cartilage and lubricating the synovial fluid in the joints.3 Moreover, HA surrounds the majority of cells in a pericellular layer where it operates as a signaling molecule, regulating cell adhesion, motility and proliferation through interactions with binding proteins. During the processes of tissue repair and regeneration, it is present in high concentrations. Consequently, HA plays a crucial part in numerous physiological and pathological circumstances.
Application of HA and its derivatives
Native HA and its derivatives represent intriguing biomaterials for a range of medical applications due to their distinctive biological and physicochemical properties (e.g., biodegradability, biocompatibility, viscoelasticity), as well as their safety profile. Additionally, they can undergo numerous chemical modifications. While some HA products are being studied for their effectiveness, others are already commercially available and/or in clinical use.2 The hydrodynamic qualities of HA are crucial in tissue hydration and physical characteristics. Hyaluronic acid is essential to the formation and maintenance of tissue architecture and its mechanical characteristics, largely due to its interactions with ECM proteins.3 Treatment with HA has been shown to exert a range of positive effects, including immunosuppressive, antiaging, anti-inflammatory, healing, and antiangiogenic properties.7
In light of the current state of knowledge, the primary goal of the study was to assess whether HA injections into the temporomandibular joint (TMJ) are beneficial in enhancing the stomatognathic function.
Material and methods
Study design
This systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO; registration No. CRD42022321304) and adhered to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA)8 standards. The review was designed using the following PICOS (Population, Intervention, Comparison, Outcome, Study design) model:
– Population – adult patients with TMJ pain or dysfunction;
– Intervention – injection of HA into the TMJ;
– Comparison – other injection materials or no intervention;
– Outcome – analgesic effect, improvement of temporomandibular function and prevention of complications;
– Study design – randomized controlled trials (RCTs).
The following PICO question was formulated: “In adult patients diagnosed with TMJ pain and dysfunction (P), what is the efficacy of infiltrating HA (I) in reducing pain, improving temporomandibular function and preventing complications (O) in comparison to other substances or no intervention (C)?”
Inclusion criteria
The present study incorporated RCTs written in English or Spanish that evaluated patients who were administered HA injections into the TMJ, with a minimum follow-up duration of half a year. In the included studies, in addition to HA, another material or technique was used in the control group to improve pain in the TMJ.
Exclusion criteria
Non-randomized prospective or retrospective studies without a control group, studies that did not include individuals of different age groups or sexes, and studies that did not achieve the established objectives were excluded from the analysis.
Data collection
The primary outcome used to assess the effectiveness of HA in TMJ disorders was the degree of joint pain relief. Secondary outcomes included the increase in the maximum mouth opening (MMO), chewing efficiency and quality of life of the patients.
Search strategy
The search was conducted using 4 online databases: Web of Science; Cochrane Library; MEDLINE; and PubMed®. The same search strategy was implemented for all databases. The search terms included “temporomandibular joint” AND “hyaluronic acid”, with a time span covering the period from May 1, 2014 to May 1, 2023. The languages considered were English and Spanish. The search was conducted without the application of any filters. In addition, a manual search was carried out using the reference lists of papers found during the database search and of publications concerning the TMJ that were indexed in PubMed®.
Screening and selection procedures
The papers identified through database search and manual search were chosen by 2 reviewers (CGO and SBB) who separately screened the abstracts and titles. The same reviewers examined the full texts of articles that met the inclusion criteria, as well as those that lacked adequate information in the abstract and title to support a conclusion. Disagreements among the reviewers were resolved through consultation with the third reviewer (JCBB). The inter-reviewer reliability in full-text selection was determined by calculating the percentage of agreement and the kappa correlation coefficient. The studies with the longest duration of follow-up were chosen when multiple trials involved the same patient group.
Extraction of clinical data
The data was extracted in triplicate by 2 reviewers (CGO and SBB) independently. The authors were contacted when there were gaps or missing data, and they were asked to provide the missing information. Consequently, the data was not included only when it was unavailable.
The following clinical information was extracted: MMO before and after intervention; pain measured using the visual analogue scale (VAS); authors; year and journal of publication; study design; number of patients; follow-up duration; injection site; type of material injected into each joint; and clinical data.
Risk of bias
The risk of bias in each study was evaluated using the Cochrane method that is aimed at RCTs.
The quality of the evidence was assessed using the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) classification system as follows:
1. High quality of evidence: the true effect is expected to be close to the estimate;
2. Moderate quality of evidence: moderate confidence in the estimated effect. The true effect is considered to be close to the estimate, but there is a possibility that it is different;
3. Low quality of evidence: the estimated effect and the true effect may be different;
4. Very low quality of evidence: very little confidence in the estimated effect. The true effect is likely to be substantially different from the estimated effect.
The adequate level of evidence was assigned to the studies with the use of the GRADEpro 3.2 software (Evidence Prime Inc., Hamilton, USA).
Statistical analysis
The meta-analysis was performed using the Review Manager (RevMan) v. 5.3 software (The Cochrane Collaboration, Copenhagen, Denmark).
The odds ratio (OR) was used for the presentation of the dichotomous variables (complications and duration of HA filling). The difference of means (MD) with the standard deviation (SD) was utilized for the continuous variables (effectiveness of other materials), and the 95% confidence intervals (95% CIs) were used for both dichotomous and continuous variables. The differences were deemed significant for p < 0.05. To ascertain whether the outcomes had changed, a series of meta-analyses was carried out, with each analysis excluding a single study.
The heterogeneity was determined by examining the overlapping CIs in the forest plot and estimating I2 and χ2 values.
The χ2 statistic evaluates the homogeneity of the studies. If the p-value is low, the null hypothesis is rejected, and it can be concluded that heterogeneity exists. The I2 value measures the degree to which the studies agree with each other, and serves as an indicator of any inconsistencies present. Values close to 0% signify little or no heterogeneity, while values exceeding 75% indicate high heterogeneity. There are no universal guidelines for interpreting intermediate values. Generally, when I2 falls below 30–40%, the heterogeneity is regarded as low. Values ranging from 30% to 60% are classified as moderate, while those between 50% and 90% are considered significant. The test’s reliability is compromised due to its level of uncertainty. Higher p-values for χ2 and lower I2 values are indicative of greater consistency between studies.
Results
Study selection
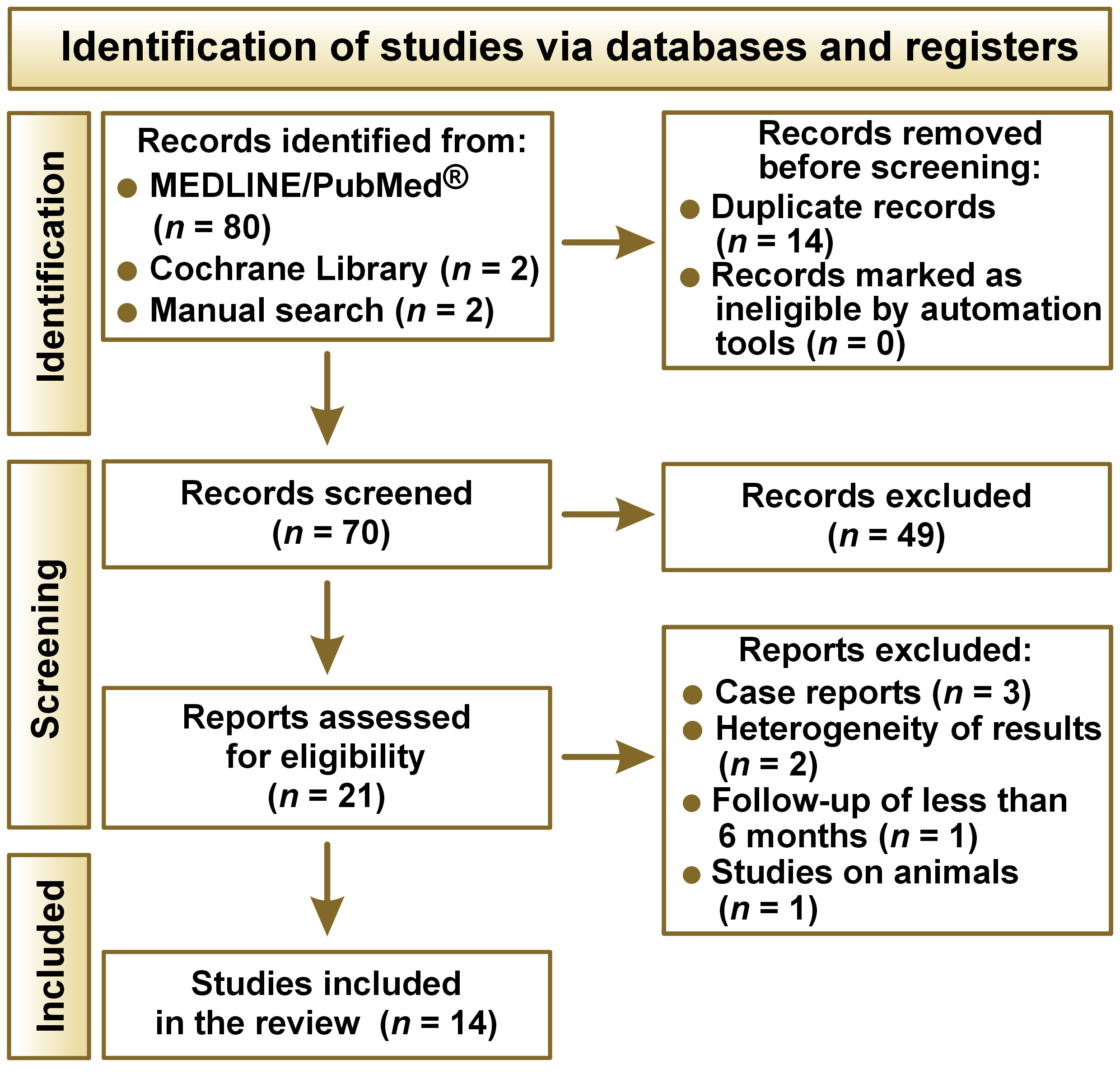
The initial database search yielded 2 titles in the Cochrane Library and 80 articles in the MEDLINE/PubMed® databases. Two additional documents were discovered during the manual search. Fourteen articles were identified as duplicates and eliminated. The full texts of 21 publications were examined following an initial screening to identify articles that did not align with the PICO criteria. This was followed by screening of titles and abstracts. Ultimately, after the extraction and analysis of the data, a total of 14 papers were chosen for the analysis (Table 1). The steps involved in the selection process are depicted in the flow diagram presented in Figure 1.
Synthesis of results
In addition to examining the features of each study and the quantity of events (patients treated with HA and patients treated with other treatment modalities), a comparison was made between the efficacy of HA and other treatments in improving the stomatognathic function of the TMJ.
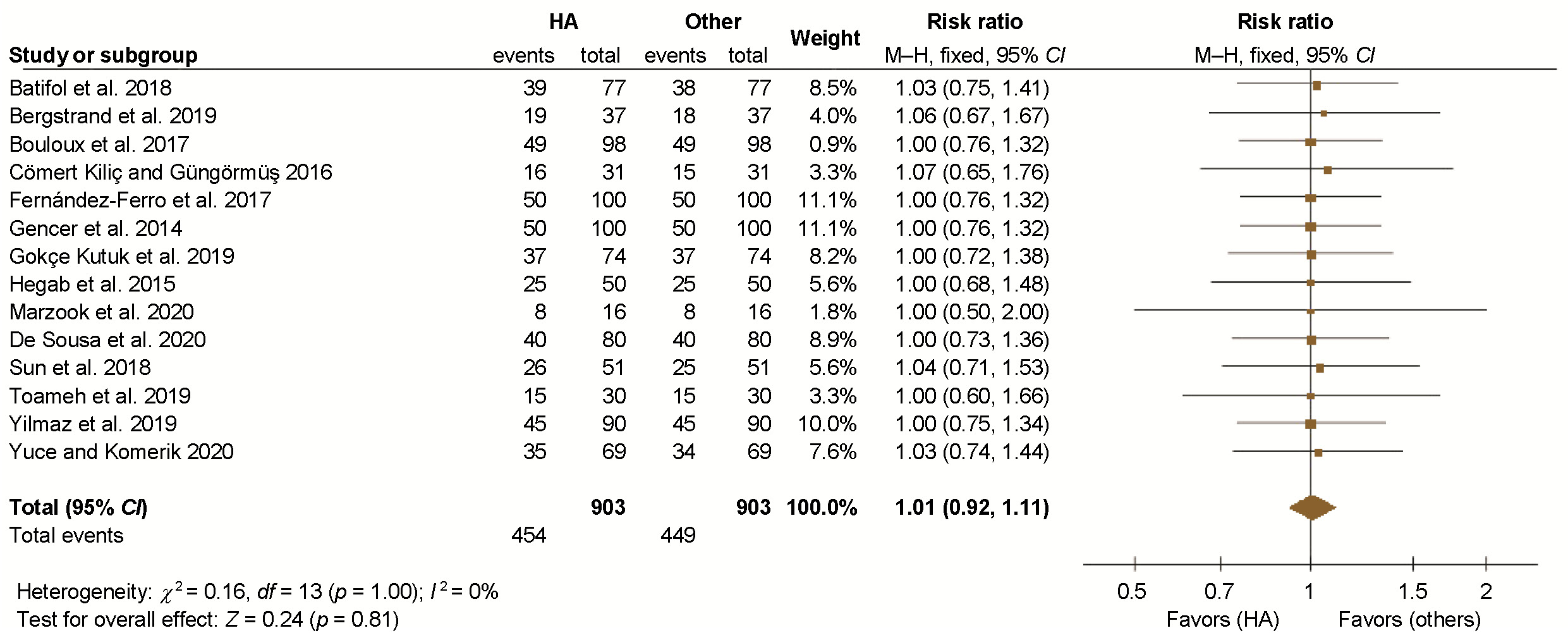
The results of the meta-analysis are displayed in Figure 2. A meta-analysis of fixed effects with relative risk has been conducted. The studies depicted on the left side of the forest plot suggest that HA treatment is more successful, while those on the right indicate that alternative therapies yield better outcomes and provide greater support for the stomatognathic function. The overall effect is expressed as a risk ratio (RR) of 1.01, with 95% CIs of 0.92–1.11 and a p-value of 0.81.
Studies exhibiting a RR of 1, or, in instances where the RR exceeds 1 but the CIs encompass the value of 1, demonstrate that HA and other therapeutic interventions are equally efficacious in enhancing the stomatognathic function of the TMJ. All of the studies demonstrated this outcome.
In general, with a total RR of 1.01 (0.92–1.11), there is no statistical evidence that HA treatment is more effective than another in terms of aesthetics or oral-dentofacial functionality. The sample showed no heterogeneity, with a p-value bigger than 0.05 (p = 1.00) and I2 of 0%. Therefore, the studies included in the meta-analysis are similar.
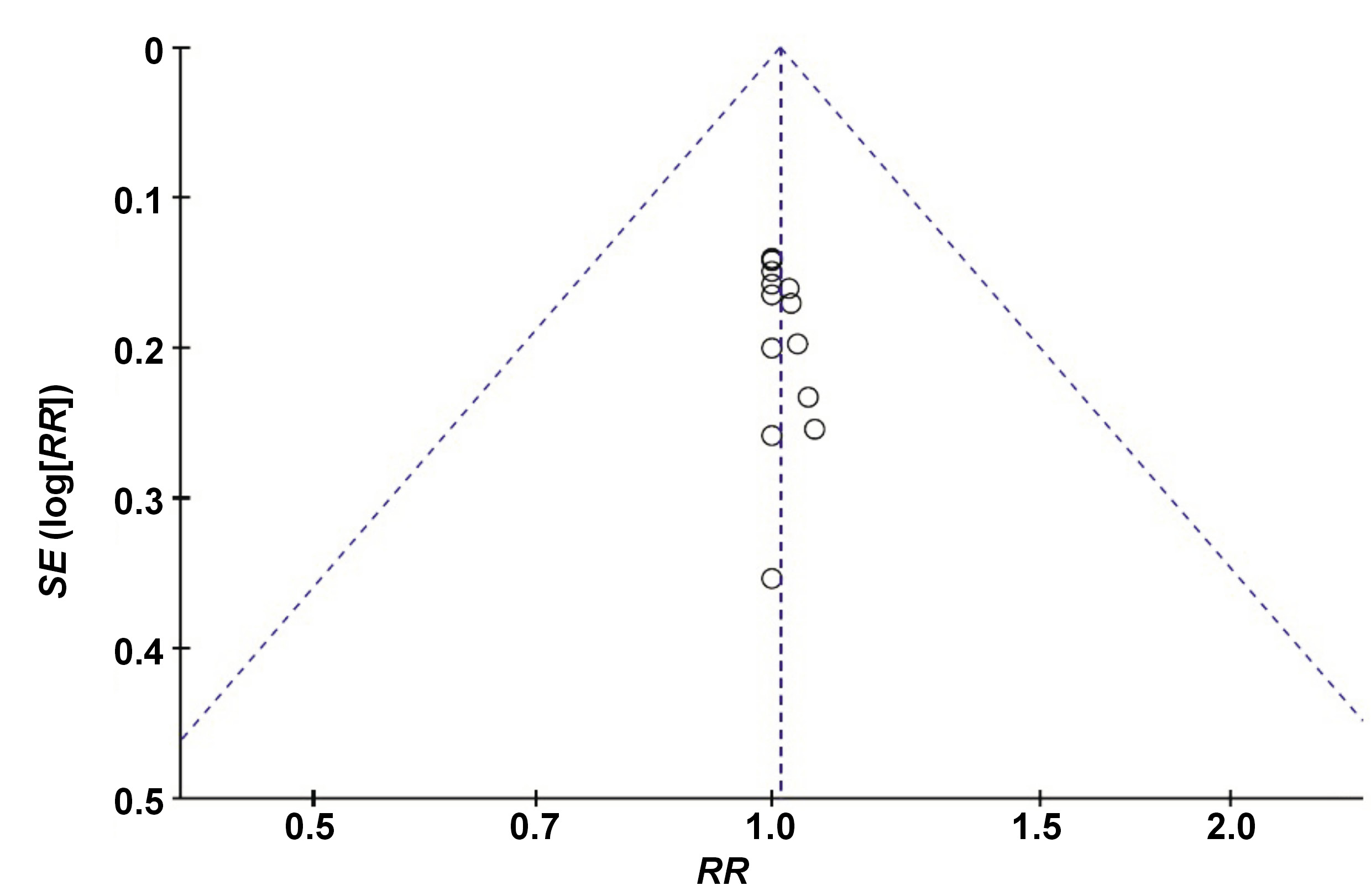
Figure 3 presents the funnel plot of the meta-analysis, where the symmetric distribution of the studies is observed. Consequently, the risk of publication bias is low.
Discussion
The use of HA in patients with TMJ pain and dysfunction has been described in numerous studies.
The comparative efficacy of HA and liquid platelet-rich fibrin (L-PRF) injections intraarticularly after arthrocentesis in patients with TMJ pain and dysfunction was assessed in a study by Yuce and Komerik.10 All techniques have been shown to improve MMO and reduce pain. However, when considering MMO and a consistent improvement in pain reduction, arthrocentesis in conjunction with L-PRF provided superior outcomes.9, 10
Similar outcomes were observed in the study by Toameh et al., which included individuals with TMJ issues and disc displacement without reduction.11 When compared to either platelet-rich plasma (PRP) or HA alone, arthrocentesis using Ringer’s solution produced a statistically significant improvement in MMO and all other parameters of pain intensity and chewing efficacy.11
However, a considerably higher rise in MMO is observed in the PRP and HA groups, and the PRP group demonstrates better results in terms of chewing efficacy and pain intensity. Thus, in the prior study,11 arthrocentesis + PRP exhibited superior outcomes in comparison to arthrocentesis + HA or arthrocentesis alone. Hegab et al. came to the same conclusions, as they determined that PRP outperformed HA in the long term for the treatment of TMJ osteoarthritis with respect to pain reduction and increased MMO.12 However, PRP injections should not be considered a first-line therapy option since, according to the experiment conducted by Cömert Kiliç and Güngörmüs, arthrocentesis + PRP injections are not more efficacious than the combination of arthrocentesis with a single HA injection.13
Arthrocentesis using Ringer’s solution was also implemented in a RCT by Marzook et al., and intra-articular injection was compared to a mixture of 0.5 mL of HA and an equal quantity of corticosteroid (CS).9 The study found improvements in all measured outcomes, with no notable variations observed across the groups.9 Due to its simplicity, intra-articular injection of HA and CS has been the treatment of choice for internal TMJ dysfunction with reduction.9 In addition, Bergstrand et al. examined the effects of arthrocentesis with lavage alone compared to arthrocentesis with lavage + HA in patients with osteoarthritis.14 Arthrocentesis of the TMJ increased the stomatognathic function and reduced pain. Although MMO levels increased in all groups, no significant differences were observed in MMO or reported pain levels. No discernible improvement in joint sounds was observed within the groups. The long-term application of both approaches resulted in a significant enhancement in jaw discomfort and function. Compared to arthrocentesis with lavage alone, arthrocentesis with lavage + HA did not demonstrate a significant advantage.14, 15
In the study by Bouloux et al., the authors noted that arthrocentesis with Ringer’s solution is as effective as arthrocentesis with HA or CS in reducing TMJ pain.16 There were no significant differences between the 3 groups.16
Yilmaz et al. posit that arthrocentesis + HA injection and the administration of a single HA injection without arthrocentesis effectively alleviated signs and symptoms in patients with reduced and non-reduced disc displacement-related joint pain, with the exception of joint sounds.17 However, the combination of arthrocentesis and HA injection yielded better results regarding chewing efficiency and patient quality of life than a single HA injection.17
Gencer et al. compared 3 anti-inflammatory agents.18 Better pain relief scores were obtained in the HA group (intra-articular injection of Hyalgan® 10 mg/mL) compared to the betamethasone or tenoxicam groups. A notable disadvantage of HA is its relatively higher cost in comparison to the other 2 agents. Despite the lower scores of intra-articular tenoxicam or betamethasone, they demonstrated better outcomes than the control group and can be considered more economical alternatives to intra-articular HA injections.18
De Sousa et al. examined the impact of various therapies on patients with TMJ arthralgia.19 Every study participant wore a night bite splint. Some individuals received merely the splint, while others were administered injections of betamethasone (7 mg/mL), PRP or sodium hyaluronate (Hyalart® 10 mg/mL). The administration of each treatment resulted in a decrease in pain and an increase in MMO. By the conclusion of the first week, the patients receiving betamethasone or HA treatments demonstrated the most optimal outcomes. However, a long-term success rate was higher when the splint was used in conjunction with the PRP injection.19 In the RCT conducted by Gokçe Kutuk et al. in patients with TMJ pain and TMJ osteoarthritis, the authors showed that intra-articular PRP injections decrease pain on palpation more effectively than HA and CS.20
Fernández-Ferro et al. noted that the injection of plasma rich in growth factors (PRGF) after arthroscopy is more effective in mitigating pain compared to the injection of 1% HA post-procedure, particularly in patients with advanced internal TMJ disorder.21 Regarding MMO, an increase was observed in both groups, with no significant difference between them.21
Sun et al. evaluated the clinical effects of injecting 20 mg of HA in the upper and lower joint space for the treatment of osteoarthritis.22 The injection alleviated the clinical signs and symptoms of osteoarthritis but did not reverse or prevent the progression of bone destruction during short- and long-term follow-up periods.22
Lastly, Batifol et al. reported a course of treatment for severe and refractory TMJ discomfort that included tongue splints, physical therapy, intramuscular botulinum toxin injections, and HA injections prior to intra-articular Botox® (botulinum toxin type A) injections.23 According to this study, a botulinum toxin injection is a risk-free, non-surgical treatment for severe and refractory temporal bone pain.23, 24, 25, 26, 27, 28, 29, 30
Conclusions
Hyaluronic acid improves the stomatognathic function in patients with TMJ dysfunction and associated pain. Additionally, it has been demonstrated to be both effective and safe in reducing pain and increasing MMO. In comparison to PRP, HA has shown superior long-term results.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.