Abstract
Indirect laminate veneers can deliver excellent esthetic results, but their use must remain secondary to biological and functional principles, requiring an ethical and evidence-based approach during treatment planning.
Keywords: minimally invasive dentistry, esthetic dentistry, adhesive dentistry, evidence-based dentistry, ethical dental practice
Porcelain laminate veneers, first introduced in the early 20th century, have gained popularity due to advancement in ceramic materials, adhesive systems and computer-aided design/computer-aided manufacturing (CAD/CAM) technologies.1 These innovations have enabled more conservative and predictable preparations while meeting the rising demand for esthetic dental treatment – a phenomenon influenced by modern beauty standards and the concept of “emotional dentistry.”
It is well known that the veneers bonded to enamel have greater fracture resistance than those bonded to dentin, making minimally invasive dentistry critical not only for biological reasons, but also for the durability of restorations. When properly planned and executed, porcelain veneers offer an effective solution with a success rate exceeding 90% in long-term studies.2, 3
Key success factors include detailed case planning, enamel preservation, tooth vitality, appropriate material selection, and adherence to the technique. Failure often results from ignoring limitations – especially in young patients with large pulp chambers and minimal wear – or from overtreatment, driven by profit rather than clinical need. Problems such as microleakage, fractures and detachment are more common when the technique is poorly executed.3, 4, 5, 6, 7
Indications for veneers include minor color corrections, abnormal tooth contours, diastemas, recession exposing dentin, malformations, and wear.3, 4, 5, 6, 7, 8 They do not include patients seeking cosmetic enhancement due to societal pressure. In comparison with full crowns, veneer preparations are about 50% more conservative.7, 8, 9 They are typically used to treat resistant tooth discoloration, morphological changes, diastemas, incisal wear, fractures, or non-esthetic conditions.10, 11, 12, 13
A growing concern is that untrained or underqualified practitioners, driven by high demand, may overlook conservative alternatives, leading to overtreatment and irreversible damage. Ethical practice requires full disclosure of all restorative options, prioritizing preservation over esthetics when appropriate.7 When performed correctly, veneer treatment is highly durable, with studies showing survival rates of 92% at 6 years and 86% at 12 years.1 Success is also related to the dentist’s and technician’s expertise.
Ultimately, 3 pillars underpin successful outcomes: understanding the treatment concept; technical accuracy; and long-term maintenance. These steps focus on minimizing complications and extending the longevity of the restoration. As the number of prosthetic procedures increase, this raises critical questions about how they align with the principles of preventive dentistry and the importance of dental tissue preservation in modern practice.3
Furthermore, patient age must be considered, especially for the young. Younger individuals have larger pulp chambers; thus, even minimal tooth reduction (0.5 mm) risks postoperative sensitivity and potential pulp damage. Additionally, the longevity of veneers – while high (85–95% over 5–20 years) – still necessitates replacement eventually, leading to further tooth reduction.8, 9, 10
Enamel wear from aging also affects veneer viability. Enamel thickness decreases with age, especially after 50, increasing the risk of exposing dentin during preparation. Adhesion to enamel is more predictable than in the case of dentin, where moisture control is difficult and structural properties are inferior, raising the risk of fractures. Adhesive cementation can mitigate some issues, but not all.11
A critical question arises: Are we overtreating? Despite being termed “conservative,” veneer preparation may remove up to 30% of healthy enamel.8 The goal of restorative dentistry should be to preserve natural tooth structures while addressing disease and function. When esthetic concerns are the only issue, less invasive options like whitening or orthodontics should be prioritized. Veneers should not substitute appropriate orthodontic treatment, especially in younger patients or those with crowded teeth, as this may require excessive tooth reduction and increase complications.10
Informed consent is essential. Patients must understand biological costs, the need for enamel preservation and the long-term implications of dentin exposure. Gurel et al. found failure rates of 89.3% when veneer margins extended into dentin vs. significantly higher survival when the margins remained in enamel.2
Another option would be treatment with direct composite veneers, which can offer good esthetics and preserve healthy tooth structures. Though more prone to degradation and staining than ceramics, their reversibility and repairability make them ideal for borderline cases. Studies show survival rates of ~80–100% over 3–6 years for composite restorations.3
The veneer philosophy has evolved. Initially, no-prep veneers were preferred to avoid invasiveness. However, they often lead to overcontoured restorations and soft tissue irritation. A standard reduction of 0.3–1 mm is now recommended to allow proper material thickness and esthetics. Standardized diamond burs and mock-ups help guide tooth reduction while preserving enamel.12 Yet, aggressive preparation is still common, particularly in esthetic-driven practices. Preparation should be individualized, especially in additive cases, such as diastemas or worn teeth, to avoid unnecessary enamel removal. No-prep veneers are only suitable when natural tooth contours allow a 0.3-millimeter material thickness without overbuilding.13, 14
Veneer materials have also advanced.15 Feldspathic ceramics, though esthetically superior, are brittle and difficult to fabricate in thin layers.16 Newer materials for indirect restorations like lithium disilicate offer greater fracture resistance and are suitable for ultra-thin veneers (as thin as 0.3 mm).14, 15, 16, 17
From a laboratory perspective, a chamfer finish line remains important for predictable fabrication. Diagnostic tools like mock-ups, temporary composite veneers and wax-ups enable clinicians to visualize final outcomes and determine necessary reduction more accurately.12
Digital dentistry has emerged as a key ally. Approaches like the anatomical shell technique aim to replicate natural tooth morphology, improving predictability and reducing reliance on manual skills.12, 13, 14, 15, 16, 17 Digital systems facilitate obtaining high-quality esthetic results and enable the reproduction of various kinds of tooth morphology.18 However, limitations remain, especially in replicating the optical dynamics of single anterior teeth, something 3D-printing technologies may overcome when associated with intraoral scanning.19
In the context of material selection, lithium disilicate ceramics – particularly those fabricated through milling – can show superior wear resistance as compared to feldspathic ceramics, which demonstrate lower wear performance, but behave similarly to heat-pressed lithium disilicate ceramics.20
In summary, veneers should not be a default esthetic solution. Treatment decisions must be grounded in ethical practice, clinical need and respect for biological preservation. Dentists must guide patients responsibly, proposing conservative options first, and ensuring long-term function and esthetics are achieved with minimal harm.
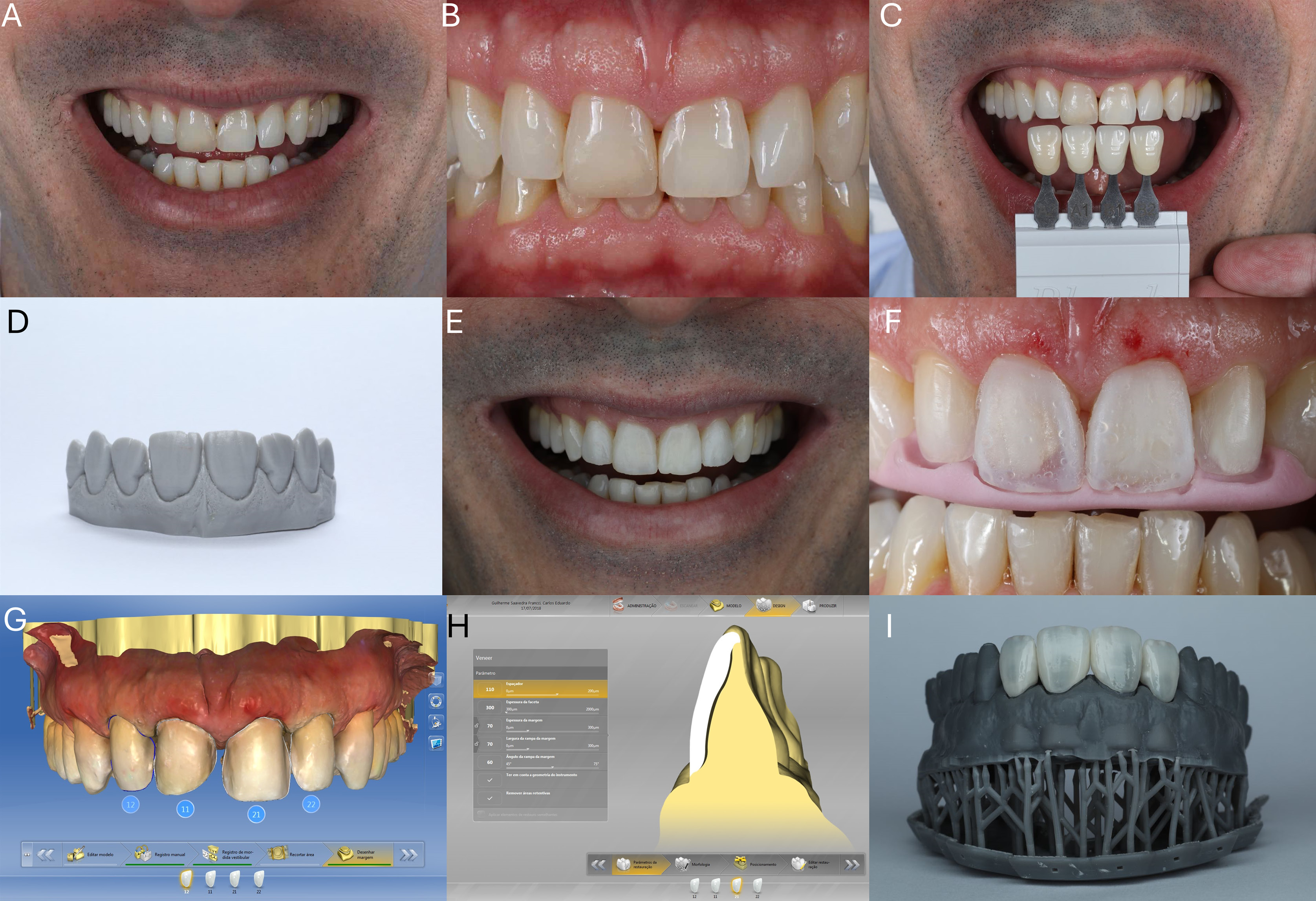
After shared decision making on an indirect veneer, one possible clinical protocol can be summarized as follows (Figure 1 and Figure 2):
1. Initial Assessment. Comprehensive photographic documentation of the patient’s smile should be performed, including images with lips at rest, during maximum smile, intraoral views, profile views, and detailed photographs of the maxillary anterior region. This step should be conducted in accordance with ethical treatment planning and shared decision making, ensuring that both esthetic and functional needs are met.
2. Shade and Proportion Analysis. Select the appropriate tooth shade under standardized lighting conditions. Evaluate the height-to-width ratio of central incisors to assist in determining the ideal tooth shape. Measure the gingival sulcus depth to assess the potential need for soft tissue modification.
3. Tooth Morphology Selection and Mock-up. Choose a morphological tooth model that harmonizes with the patient’s facial and dental proportions. Fabricate provisional resin veneers, using a matrix derived from the selected model. Place the mock-up intraorally to evaluate esthetics and function. Scan the intraoral mock-up to generate a digital model with corrected proportions.
4. Gingival Correction. If indicated, perform a gingivectomy guided by the mock-up and the previously obtained sulcus measurements to refine the gingival zeniths and improve symmetry.
5. Tooth Preparation. After soft tissue healing, prepare the teeth for veneers, using the mock-up or a silicone index as a guide. This approach ensures minimally invasive preparation, prioritizing enamel preservation.
6. Digital Workflow and Design. Capture intraoral scans of the prepared teeth. Utilize CAD software to design restorations based on the scanned mock-up, adjusting design parameters and finalizing the morphology as needed.
7. Model Printing and Verification. Digitally edit and print physical models to verify the fit and adaptation of the restorations. Perform adjustments, finishing and extrinsic staining on the ceramic veneers before final placement.
8. Cementation. Bond the milled ceramic laminate veneers, using adhesive cementation techniques under proper isolation.
9. Final Evaluation. Acquire postoperative photographs from multiple angles, including frontal views with lips at rest and smiling, as well as intraoral, occlusal and profile views. These images can be later used to assess esthetic outcomes and verify incisal edge-to-lip harmony.
Conclusions
Indirect veneers are a reliable solution for esthetic dental issues, offering long-term success with significantly less tooth reduction than full crowns. However, ethical and effective treatment requires individualized diagnosis, patient-centered planning and the consideration of all available alternatives. Clinicians must be properly trained and inform patients of the benefits, limitations and potential risks, especially regarding dentin exposure. To preserve healthy tooth structures, veneer preparations should be carefully planned, using tools like diagnostic wax-ups, mock-ups and/or silicone guides.