Abstract
The following description outlines how the current standards for treating mandibular condyle fractures hatched, so that they have grown into mature techniques for guiding patients to recovery.
Keywords: mandible condyle, fracture treatment, open rigid internal fixation
The aim of the present article is to highlight the long way of mandibular condylar process fracture treatment leading to a satisfactory and low-complication-rate outcome.
Treatment modalities for condylar process fractures remain the most controversial issue in maxillofacial traumatology. This is strange, since a fracture of the mandible is the most common fracture of the facial skeleton, and the condylar process is the most common location of mandibular fractures.1 This epidemiology is due to the rather prominent anatomical position of the mandible and some difficulties in protecting it.
The earliest records on the treatment of mandibular fractures date back to the Bronze Age.2 In the “Edwin Smith Papyrus” there is a case report written in 1700 B.C. The author of this military medical guide advises not treating an open fracture of the mandible, since the patient will die anyway.
This state of medical knowledge persisted until the Napoleonic Wars, when Desault pointed out that in the treatment of mandibular condylar process fractures, it was very important to achieve good contact between two bone fragments.3 The impetus for the development of maxillofacial traumatology appeared to be armed conflicts, i.e., World Wars I and II, the Korean War, and the Vietnam War, due to the involvement of large, rich countries and a rapidly increasing number of patients. Lambotte introduced the term ‘osteosynthesis’ (1907), Kazanjian used the splinting of the teeth, tooth ligation and bone sutures (1914–1918), Ivy introduced a ligature with a loop (1922), and Ginestet introduced Kirshner wires and external immobilization (1936). Later, onlay individual silver splints were used for the immobilization of reduced bone fragments. Then, the era of closed treatment in all mandibular fractures, including condylar fractures, set in.4 However, in 1886, the young and relatively unknown surgeon Carl Hansmann presented his experience with the plate osteosynthesis system at the annual meeting of the German Surgical Society.5 He described 2 patients with mandibular fractures he treated with his method. Today, Hansmann is undisputedly considered the inventor of plate osteosynthesis. His subcutaneous plate, fixed with percutaneous screws, bears little resemblance to the plate systems of today. It was open reduction and rigid fixation (ORIF), so called today. Halsted refined this system, introduced it to the USA and used head screws for open internal osteosynthesis in 1893.6, 7 Open reduction and rigid fixation stayed in the shadow of closed treatment for many consecutive decades because of its high complication rates, especially the risk of osteomyelitis. Except for a few isolated reports, plate osteosynthesis was therefore unable to gain widespread acceptance. This was due to the use of inadequate implant materials (corrosion); plates and screws often caused inflammatory lesions, and in the worst cases, osteomyelitis with its catastrophic consequences. This, in turn, led to the general view of “not too much metal for bone.” As a result, the chosen implants were too small, and therefore too weak, which, in addition to corrosion problems, caused instability in the fracture area, which is fatal in osteosynthesis. Non-physiological handling of the bone, i.e., the extensive elevation of the periosteum and too rapid rotations during pre-drilling with insufficient cooling led to premature loosening of the screws. The reduction of susceptibility to corrosion occurred with the invention of chromium-cobalt-molybdenum (Cr-Co-Mo) alloy Vitallium, used by Bigelow in 1943.8 However, external fixation was still used as during WWI.
To overcome this situation and advance toward modern maxillofacial treatment, scientific progress was necessary, i.e., new materials (stainless steel patented in 1915; stainless steel with the addition of Mo to increase resistance to chloride-induced rusting in 1930; the miniaturization of osteosynthetic materials; the development of materials dedicated to maxillofacial surgery, not just the adaptation of orthopedic solutions), the improvement of anesthesiology (first general anesthesia by Hanaoka using tsūsensan in 1804; the creation of specialization in 1912; the introduction of the Macintosh laryngoscope curved blades in 1943; general anesthesia with intubation and relaxation by Pokrzywnicki in Poland in 1947; the replacement of flammable gases with Halothane in 1956, which was then gradually replaced with halogenated ethers, introduced in 1970s), the development of radiological techniques (pantomography: 1970s; computed tomography (CT) scanning: 1980s), as well as the introduction of effective bactericidal medications (penicillin: after World War II; chlorhexidine: 1950s; metronidasol: 1960; lincomycin: 1962; clindamycin: 1966) and specially designed surgical instruments.
The truly modern approach to ORIF is the post-WWII period. First, Robinson should be recalled.9 His L-shape plate is made of stainless steel, which gives it a thinness not met with other plates described in his time, with regard to using the casting method. Robinson used periangular skin access and reported no facial nerve weakness in his patients. He originally recommended ORIF when a patient could not be immobilized with maxillomandibular ligation, but he noticed ORIF was beneficial for most patients with mandibular condylar process fractures. He recommended ORIF for multiple fractures of the mandible, when more stability is needed than is obtained with wire sutures, which were widely used up to 1980s. He mentioned the use of only 2 screws per fracture as an advantage (he used self-tapping screws, 2.7 mm in diameter, with bicortical anchorage).
In those times, the most important question was: “close or open treatment?”10 Surprisingly, most maxillofacial surgeons believed that most fractures of the condylar process of the mandible should be treated non-surgically, and certainly most fractures of the mandibular head. Alternatively, in terms of surgical treatment, it was speculated whether in the case of a mandibular head fracture, the entire lower fragment should be removed, which prevents ankylosis, but irreversibly degrades the stomatognathic system. Korzon summed up his research in 1971: “Assessing the long-term results of closed and conservative treatment of the fractures of the condylar process of the mandible, it was found that only conservative treatment does not always give good results. It fails in fractures with significant displacements, with dislocation, and especially in old fractures of the condylar process of the mandible. Incorrect positioning of bone fragments causes a number of disorders in the masticatory system.”10 Nowadays we know the proper answer, but then it was the hottest issue, or even the voice of the pioneers of the upcoming revolution.
At that time there was a resurgence of interest in the Vitallium alloy. Luhr studied the rigid fixation of the facial skeleton with Vitallium in 1960s and proposed compression osteosynthesis in 1967.6 Luhr and Spiessl reintroduced the idea of using miniature plates in osteosynthesis in 1968 and 1972. Luhr recalled the idea of using self-tapping screws (1968) and used extraoral approaches.11 Spiessl adapted the plates to the dimensions of the mandible and popularized the compression osteosynthesis of the mandible in the USA, beginning in 1971. He also used compression fixations without plates, employing lag screws bicortically (1974) and eliminating intermaxillary postoperative immobilization.12 And finally, the era of intraoral approaches opened (Luhr, 1985).13 Michelet and Moll described mandibular fractures treated with Vitallium miniplates and monocortical immobilization without intermaxillary ligatures in 1971.14 Plate sizes were reduced,6 and based on the abovementioned study, Champy developed monocortical miniplate osteosynthesis in 1976.15 It is still used today as the primary ORIF technique.
Although the possibility of the anatomical reduction of fragments and the restoration of temporomandibular joint (TMJ) function enforced the superiority of open treatment, the breakthrough came 30 years ago, when an Austrian team developed a technique for the osteosynthesis of mandibular head fractures.16 Surprisingly, and invariably since those days, US centers have not been interested in developing the treatment of condylar process fractures. This seems to be due to the fear of complications and unstable treatment results (and related patient claims). And yet, safe and effective protocols for the management of even severely comminuted fractures of the condylar process are known.17
In 1990s, surgical steel was displaced by titanium (Ti) alloys as more biocompatible.18 Another boost came from Strasbourg – extending Kessler’s 1980 study describing ideal osteosynthesis lines in the mandibular body, Meyer et al. described them in the mandible condyle.19 Since then, miniaturized materials and the knowledge of how to apply them effectively have been available.
The still asked question from the 1960s was finally answered by Neff.20 More predictable treatment results can be obtained with ORIF vs. closed treatment. It seems today that by proposing closed treatment to most patients, the clinician assumes responsibility for potentially subjecting many patients to severe dysfunction of TMJ and the entire stomatognathic system. Anyway, it is clear that applying ORIF for the fractures of the mandibular head will be the responsibility of a small number of specialized centers, to which patients from a wider area of the country will be referred, while patients with simpler types of condylar fractures will be managed in any department of maxillofacial surgery.
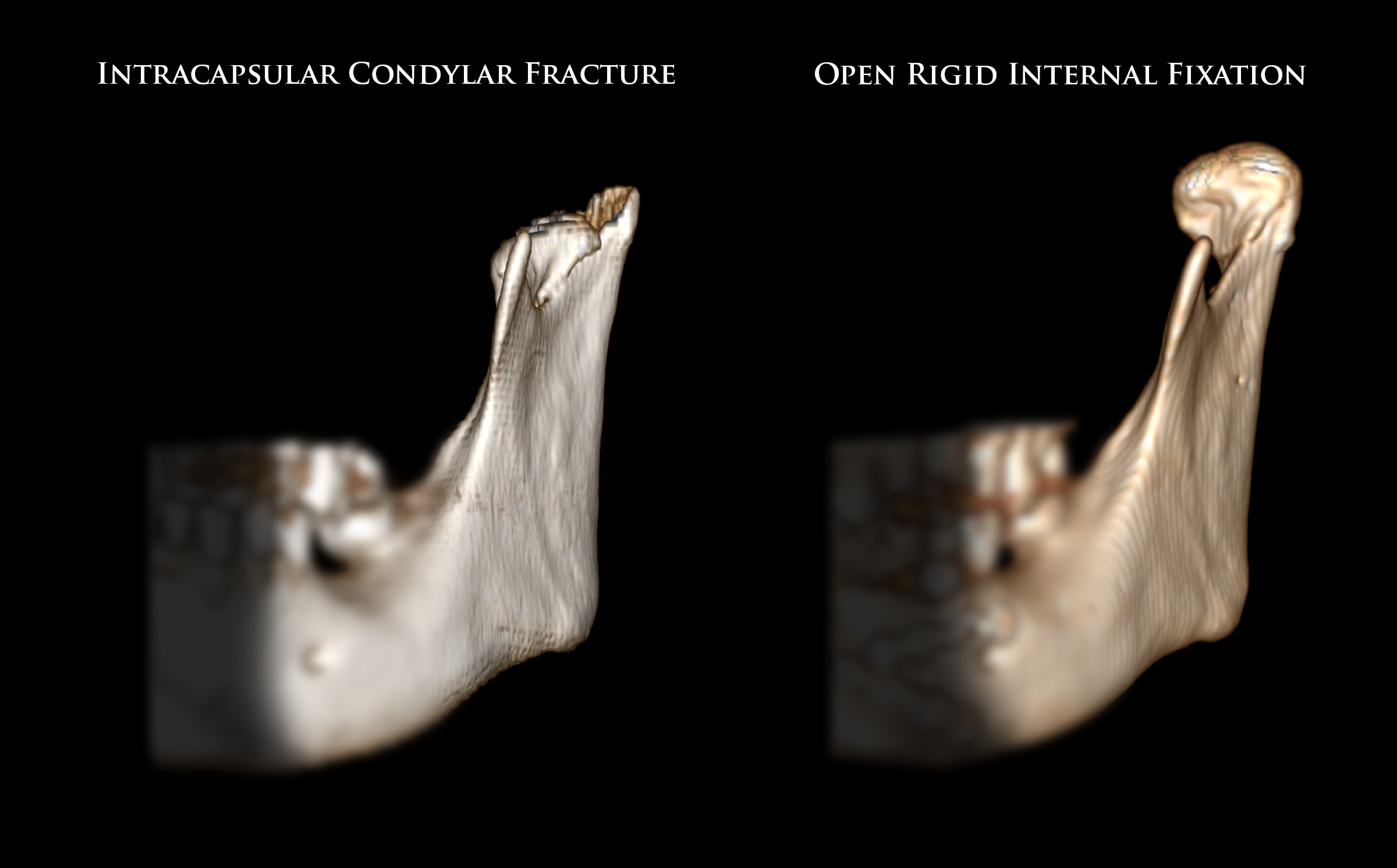
Currently, a range of effective techniques and materials is available for ORIF, enabling the successful treatment of mandibular condyle fractures. The following types of fractures are distinguished: base; neck; and mandibular head. The complexity of surgical treatment increases as these fractures are listed. Many osteosyntheses still use bicortical fixation and there is a multitude of available fixation materials. The current state of the art in managing mandibular condylar process fractures can be summarized as follows: system 2.0; self-tapping screws; Ti alloys; antibiotic prophylaxis; nasal/submental intubation; oral disinfection; intraoral approaches; limited periosteal detachment; monocortical anchorage; the consideration of bone stress areas; water cooling; no intermaxillary immobilization after surgery; and the removal of the fixation material after the period of bone union formation (Figure 1). The ORIF modalities are continually evolving to enhance efficacy, and the field offers substantial scope for further innovation.
Concluding, it must be stated that over the past decades, the approach to fracture treatment has rapidly evolved from closed treatment to ORIF. The current scientific evidence indicates that most patients will benefit from open treatment and osteosynthesis. This reflects the progress in diagnostic techniques, fixation materials and surgical skill.