Abstract
Intimacy, including partnered sex or masturbation, may modestly improve sleep continuity via neuroendocrine and circadian pathways, supporting cautious, ethical and patient-centred integration into behavioral sleep medicine.
Keywords: sleep, sleep disorders, sexual behavior, sexual medicine
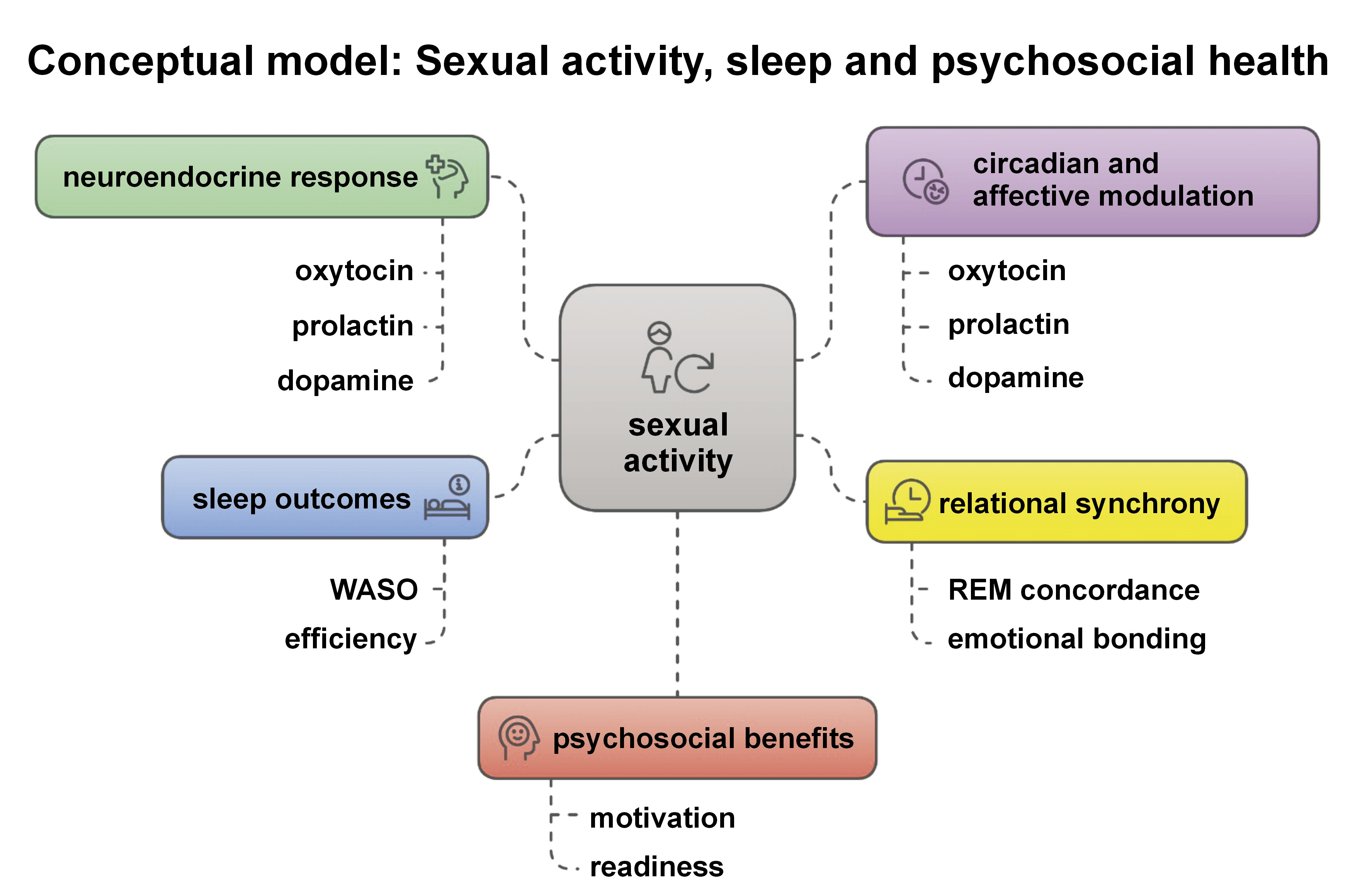
In an era marked by the rising prevalence of sleep disturbances and the escalating dependence on pharmacological treatment, the search for effective, low-risk and accessible behavioral interventions is both urgent and timely. Within this context, the study by Lastella et al., “Sleep on it: A pilot study exploring the impact of sexual activity on sleep outcomes in cohabiting couples,”1 offers a scientifically stimulating, albeit preliminary, contribution. By assessing sexual behavior, including both partnered activity and masturbation, as a pre-sleep activity through ecological polysomnography and subjective outcomes, the authors uncover suggestive evidence that intimacy may offer relevant insights for individual and potentially public health strategies, although further validation is clearly warranted.
The findings, highlighting modest improvement in wake after sleep onset (WASO) and increased sleep efficiency, invite cautious consideration of intimacy as a potential behavioral factor in sleep health. These effects are likely mediated through the neuroendocrine mechanisms involving oxytocin, prolactin and dopamine, and the downregulation of stress hormones, such as cortisol, pathways well-known for influencing both sleep and emotional regulation. However, it is crucial to interpret such benefits within the scope and limitations of the original sample (7 couples), and not to overstate their generalizability.
Drawing from neurochronobiological insights,2 sexual and romantic behaviors, although distinct in function, are both modulated by circadian rhythms, affective neurobiology and sleep architecture. The neurochemical correlates of intimacy and sexual engagement may influence the regulation of rapid eye movement (REM) sleep, emotional processing and the stability of relational bonding. The circadian timing of these behaviors seems to be critical3 and may potentiate their effects, opening the door to chrono-sexual interventions, tailored approaches that align intimacy with individual circadian typologies for optimized outcomes.
Importantly, the possible role of these behavioral pathways extends beyond sleep outcomes. The exploration of sexual activity (whether partnered or solitary) as a coping mechanism for psychosocial stress,4 anxiety, depressive symptoms, and obsessive-compulsive tendencies5 opens a line of investigation that is both clinically relevant and ethically delicate. While pharmacological interventions remain essential for many, they are not without side effects, including REM sleep suppression, cognitive impairment and the risk of dependency. In contrast, sexually intimate behavior, when voluntary and contextually appropriate, may provide a socially reinforcing alternative with fewer adverse consequences. Yet, such behavioral suggestions must be personalized and consensual, with attention to the risk of coercion or the disruption of spontaneity within relationships.
The relational aspect further deserves careful interpretation. The observed synchronization in REM sleep among cosleeping partners suggests that intimacy may enhance sleep through both physiological and interpersonal pathways. Still, such phenomena are contingent upon the quality and dynamics of the relationship. Masturbation, also included in the Lastella et al.’s study, showed similar outcomes,1 which implies that the sleep-promoting effects of sexual behavior are not solely dependent on relational engagement, but may stem from neurobiological mechanisms inherent to sexual arousal and release.
We recognize the controversy surrounding the concept of framing sexual behavior as a ‘therapy.’ While we do not suggest replacing validated clinical interventions, we advocate for further empirical exploration of intimacy-related behaviors as part of a broader behavioral health framework, especially in cases where pharmacological options are contraindicated or poorly tolerated.
To that end, we support a more nuanced approach that integrates sexual activity into the therapeutic dialogue not as a universal recommendation, but as an optional behavioral strategy, applicable in select, consensual and informed contexts. This complements, rather than replaces, current therapeutic modalities and supports a more person-centered model of care.
Recent literature exploring sex differences and sleep-related vulnerabilities also provides a relevant backdrop to these discussions. For instance, emerging evidence indicates that women are more likely to suffer from insomnia and subjective sleep complaints, partly due to hormonal fluctuations, caregiving roles and circadian misalignment. Men, conversely, may be underdiagnosed for disorders like obstructive sleep apnea, which presents differently across sexes and is often correlated with different behavioral triggers.6 Furthermore, the influence of hormones on sleep architecture (e.g., the role of estrogen in REM sleep regulation) suggests the need to tailor behavioral interventions, including those involving intimacy, according to sex and the hormonal status. These insights underscore the importance of stratifying sleep interventions not only by age and relationship context, but also by sex-related physiological and behavioral traits.
Toward strategic integration: Implementing sexual behavior principles in sleep medicine
In light of these insights, a strategic framework is warranted to explore the integration of sexual behavior principles into the broader field of behavioral sleep medicine. This integration must be cautious, respectful of ethical boundaries and rooted in scientific evidence. The approach can unfold across 4 domains: clinical practice; research; education and training; and public health policy.
1. Clinical practice
Clinicians may begin by sensitively incorporating sexual health discussions into sleep consultations, recognizing both partnered intimacy and solitary sexual activity as potentially relevant factors. These conversations must be framed with care to avoid coercion or discomfort. Couple-based behavioral therapies may consider the relational context of sleep disruption and intimacy, and interventions could be personalized based on the chronotype, the attachment style and relational dynamics (Figure 1).
2. Research
Future studies should focus on randomized controlled trials to examine the short- and long-term effects of sexual activity, partnered or solo, on sleep architecture, emotional regulation and circadian physiology.7 Mechanistic studies exploring neuroendocrine responses, sex-specific outcomes and chronobiological alignment are needed to establish evidence-based recommendations.
3. Education and training
Healthcare providers in sleep medicine should receive interdisciplinary training, including sexual health literacy, psychological theory and cultural competence. Programs must prepare clinicians to discuss sensitive topics respectfully and ethically, equipping them to address the diverse needs of patients.
4. Public health policy
Public health messaging can help destigmatize discussions around sexual behavior and sleep health, while policy development can promote holistic models of care that value intimacy, psychosocial wellness and non-pharmacological strategies. Importantly, these efforts must ensure inclusivity and avoid prescriptive norms.
In conclusion, the integration of sexual behavior principles into behavioral sleep medicine offers a promising avenue for non-invasive and patient-centered care. However, this potential must be approached with scientific humility, ethical vigilance and cultural sensitivity.