Abstract
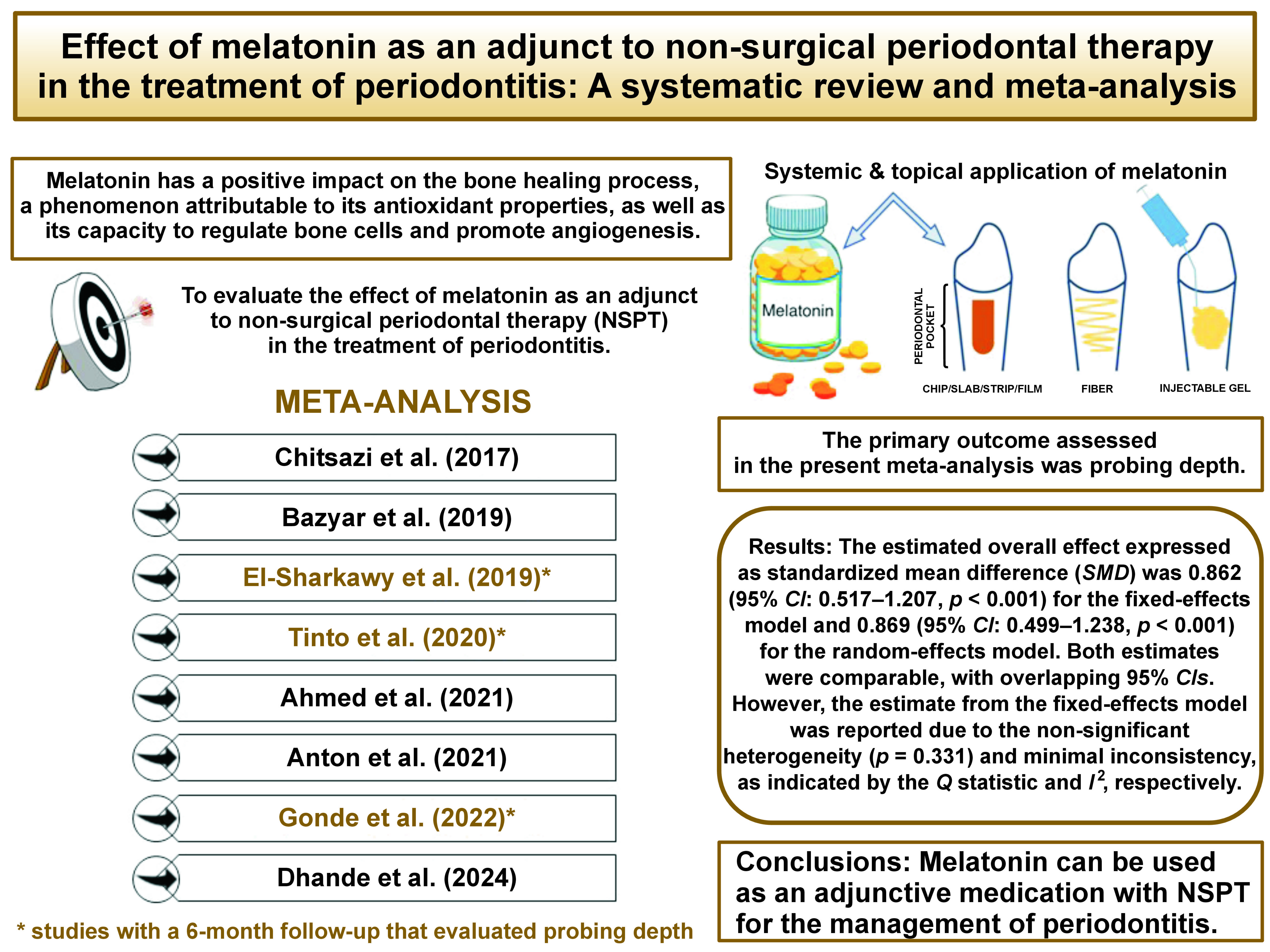
Gingivitis is defined as the inflammation of the gums. The condition may spread to other parts of the periodontium, including the periodontal ligament and alveolar bone, and lead to bony defects. Melatonin has a positive impact on the bone healing process, a phenomenon attributable to its antioxidant properties, as well as its capacity to regulate bone cells and promote angiogenesis. The present meta-analysis aimed to evaluate the effect of melatonin as an adjunct to non-surgical periodontal therapy (NSPT) in the treatment of periodontitis. A thorough electronic search of the PubMed®/MEDLINE and Google Scholar databases was conducted, in addition to a manual search of the reference lists of archived articles published until May 2023. Among the 8 reviewed articles, 3 studies that evaluated probing depth (PD) and had a 6-month follow-up period were considered for the meta-analysis. After extracting the relevant information, the risk of bias was estimated. A summary of the estimates for standardized mean differences (SMDs) from fixed-effects and random-effects models was obtained based on the mean treatment differences reported in the selected studies. The results demonstrated the overall estimated effect from the fixed-effects model (SMD = 0.862, 95% confidence interval (95% CI): 0.517–1.207, p < 0.001) and the random-effects model (SMD = 0.869, 95% CI: 0.499–1.238, p < 0.001), with minimal inconsistency as indicated by the Q statistic and I2, respectively. Thus, it can be concluded that melatonin may be used as an adjunctive medication with NSPT for the management of periodontitis.
Keywords: melatonin, periodontitis, periodontal disease, bone defects, chronic gingivitis
Introduction
Periodontitis, a chronic inflammatory disease that affects the supporting structures of the teeth, poses a significant oral health challenge worldwide. The condition is characterized by the destruction of the periodontal ligament and alveolar bone, leading to tooth loss if left untreated.1 In recent years, researchers have been exploring alternative therapeutic approaches to complement conventional periodontal treatments. One such avenue of investigation involves the role of melatonin, a hormone primarily known for regulating sleep–wake cycles,2 in the management of periodontitis.
Melatonin, a hormone synthesized by the pineal gland in the brain, exhibits diverse physiological functions beyond sleep regulation.3 It possesses powerful antioxidant, anti-inflammatory and immunomodulatory properties, making it an attractive candidate for periodontal therapy.4 Periodontitis is a multifactorial disease, and as it is also driven by an imbalanced host immune response5 and oxidative stress,6, 7 targeting these pathological factors is crucial for effective treatment.
Understanding the role of melatonin in periodontal health and disease progression may pave the way for innovative therapeutic strategies that target the underlying mechanisms of periodontitis. Melatonin can potentially enhance the outcomes of conventional periodontal treatment, that is, non-surgical periodontal therapy (NSPT), and contribute to improved oral health outcomes in individuals affected by this prevalent chronic inflammatory condition.
Melatonin can be administered systemically or locally, depending on the desired therapeutic effect and the specific needs of the patient.8
Systemic administration involves the oral ingestion of the hormone, typically in the form of tablets or capsules. Upon ingestion, melatonin is absorbed into the bloodstream and distributed throughout the body. Systemic administration of melatonin enables its potential systemic effects, including its antioxidant and immunomodulatory properties.5, 6 Moreover, it may influence sleep patterns, which can indirectly impact the overall health and healing processes in individuals with periodontitis.9
On the other hand, local administration of melatonin involves applying the hormone directly to the affected periodontal tissues. This objective can be achieved through the use of melatonin-containing mouthwashes, gels, or local drug delivery systems.10 Local administration allows for targeted delivery of melatonin to the site of inflammation and infection in the periodontal pockets. Consequently, the hormone may exert its anti-inflammatory and tissue regenerative effects directly in the periodontal tissues, potentially enhancing the efficacy of conventional periodontal treatments.
By maximizing the potential of melatonin as an adjunctive therapy, we can improve patient outcomes, reduce the progression of periodontal disease, and promote overall oral health.
The objective of this systematic review and meta-analysis was to evaluate the effectiveness of both systemic and local administration of melatonin in the management of periodontitis. The study aimed to provide a comprehensive overview of the current understanding of the effect of melatonin in periodontitis. A review of studies that have explored the potential benefits of melatonin as an adjunctive treatment in periodontitis has been conducted.
Material and methods
The PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guidelines11 implemented by the Cochrane Collaboration12 were used for reporting the present analysis. The protocol of this study was registered in PROSPERO, the International Prospective Register of Systematic Reviews (ID: CRD42023438265).
Focused question
The research question for this systematic review and meta-analysis was specifically framed based on the PICO criteria, as follows: Population (P) – patients with chronic periodontitis; Intervention (I) – systemic and local administration of melatonin; Control (C) – administration of placebo; Outcome (O) – probing depth (PD).13, 14
Information sources and search strategy
A comprehensive literature search of the PubMed®/MEDLINE and Google Scholar databases was performed to identify relevant studies. In addition, a manual search of the reference lists of archived articles was conducted. The search strategy included a combination of the following keywords: “periodontitis”; “periodontal diseases”; “non-surgical periodontal therapy”; “melatonin”; “randomized controlled trial”; “RCT”; and “clinical trials”. The search was limited to studies published up to May 2023.
Inclusion criteria
The inclusion criteria encompassed randomized controlled trials (RCTs) and controlled clinical trials investigating the use of melatonin as an adjunct to NSPT in patients with periodontitis, which reported clinical parameters such as PD.
Exclusion criteria
Studies written in languages other than English, as well as in vitro and animal studies, case reports, case series, reviews, and conference abstracts were excluded from the analysis.
Selection process
Three reviewers (PAK, SR and PR) independently screened the titles and abstracts of the articles based on the established inclusion and exclusion criteria. Subsequently, the abstracts of all relevant studies and their possible significance were independently reviewed by the investigators. To resolve any discrepancies, an additional reviewer (SU) was consulted. The full-text articles of potentially eligible studies were obtained and assessed for inclusion. At this stage, discrepancies among the reviewers were resolved through discussion and consensus. Studies were selected based on the pre-defined inclusion and exclusion criteria, as stated earlier.
Outcome measures
Probing depth, referred to as pocket depth if periodontal disease is present, is defined as the distance from the gingival margin to the apical portion of the gingival sulcus.15 The present meta-analysis analyzed PD reported in the included articles.
Software for meta-analysis
The present meta-analysis was performed in the MedCalc® statistical software v. 20.118 (MedCalc Software Ltd, Ostend, Belgium).
Data extraction
The data from the included studies was extracted using a standardized data extraction form. The extracted data included characteristics of the study (authors, year of publication, study design), characteristics of the participants (sample size, demographics), intervention details (dosage, duration), and outcome measures (PD). Disagreements in data extraction were resolved through discussion or by consulting the 3rd reviewer (SU).
Assessment of the methodological quality and risk of bias
The quality of the included studies was evaluated independently by 2 reviewers (PAK and SR) using the Cochrane Risk of Bias tool for RCTs. The tool assessed the risk of bias in the domains of random sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other biases. During the judgment process, each “yes” or “no” indicated a low or high risk of bias, respectively, while “unclear” meant an uncertain risk of bias. The study was grouped as “low risk of bias” when all the aspects were deemed to be of a low risk of bias. Conversely, it was classified as “high” or “uncertain risk of bias” when one or more aspects indicated a high or unclear risk of bias. Discrepancies in the quality assessment were resolved through discussion or involvement of the 3rd reviewer (SU).
Data synthesis
The meta-analysis was performed using appropriate statistical methods. In 2 of the 3 included studies, melatonin was administered systemically,16, 17 while in the remaining study, local administration of the hormone was implemented.18 The effect sizes (mean difference, odds ratio) and the respective 95% confidence intervals (95% CIs) were calculated for the outcome measure. The statistical heterogeneity of the included studies was assessed using the I2 statistic. In instances where substantial heterogeneity was detected, a random-effects model was used; otherwise, a fixed-effects model was applied. Subgroup analyses and sensitivity analyses were conducted as appropriate. The presence of publication bias was assessed using funnel plots and statistical tests (Egger’s test and Begg’s test).
Data interpretation and reporting
The findings of the systematic review and meta-analysis were interpreted and discussed. The strengths, limitations and implications of the included studies were considered. The results were reported following the PRISMA guidelines.
Several studies have been conducted to evaluate the effectiveness of different interventions in the treatment of patients with periodontitis, particularly involving the use of melatonin. These studies provide evidence on the effectiveness of various interventions in treating periodontitis patients, with outcomes such as PD, clinical attachment level (CAL), bleeding on probing (BOP), plaque index (PI), gingival index (GI), biochemical parameters, and bone fill being evaluated at different time points ranging from baseline to 8 weeks or 6 months.16, 17, 18, 19, 20, 21, 22, 23 The present meta-analysis was performed on only 3 studies with the same control group, a 6-month follow-up period, and PD as the outcome variable.
Results
Study selection
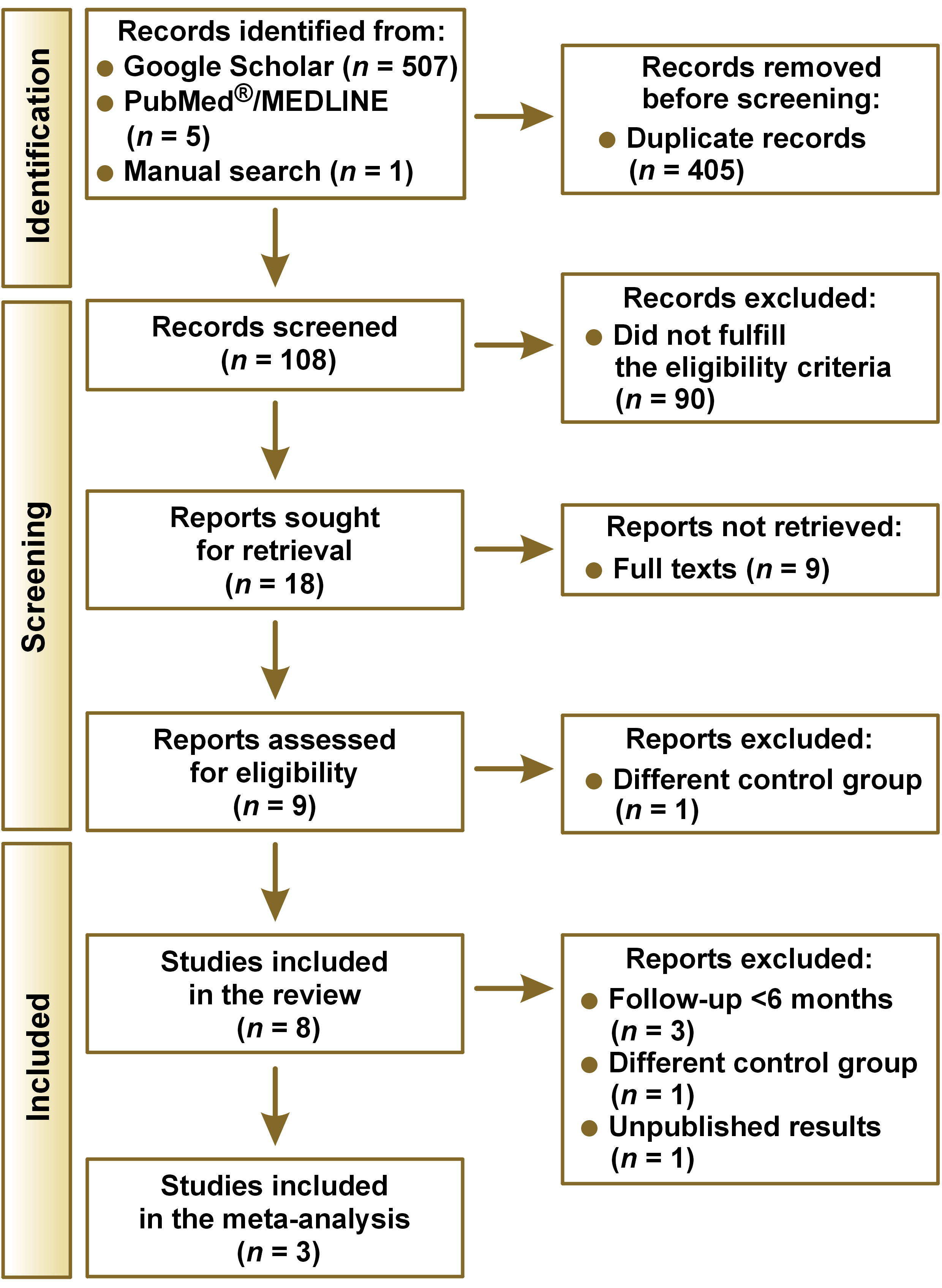
The initial search yielded a total of 513 studies, of which 405 were duplicates and were thus removed (Figure 1). The titles and abstracts of the 108 studies were screened by 2 independent reviewers who removed 100 articles deemed to be irrelevant. The papers excluded from the analysis encompassed animal studies, case series, review articles, and studies published in languages other than English. The systematic review was conducted based on 8 full-text articles. Five of these papers were excluded due to insufficient data available. The number of subjects included in these studies exhibited variability in terms of assessment parameters, the presence of a control group and the duration of the follow-up. Finally, 3 studies analyzing PD were included in the meta-analysis.
Study characteristics
Table 1 presents a comprehensive overview of the 8 studies considered for this systematic review. Three studies were included in the meta-analysis (Table 2). The data from 70 test group participants from 3 RCTs was compared to that of 68 patients in the control groups. The minimum and maximum numbers of participants per group were 10 and 38, respectively. In the test groups, melatonin was administered either locally in the form of a gel or systemically as capsules. In the control groups, a placebo drug was supplied. A 6-month follow-up period was designated in all 3 studies.
Type of interventions
The 3 studies included the same test (scaling and root planing (SRP) + melatonin) and control (SRP + placebo) groups in the experimental design. In one of these articles, melatonin was administered locally, while in the remaining studies, participants were given oral capsules.
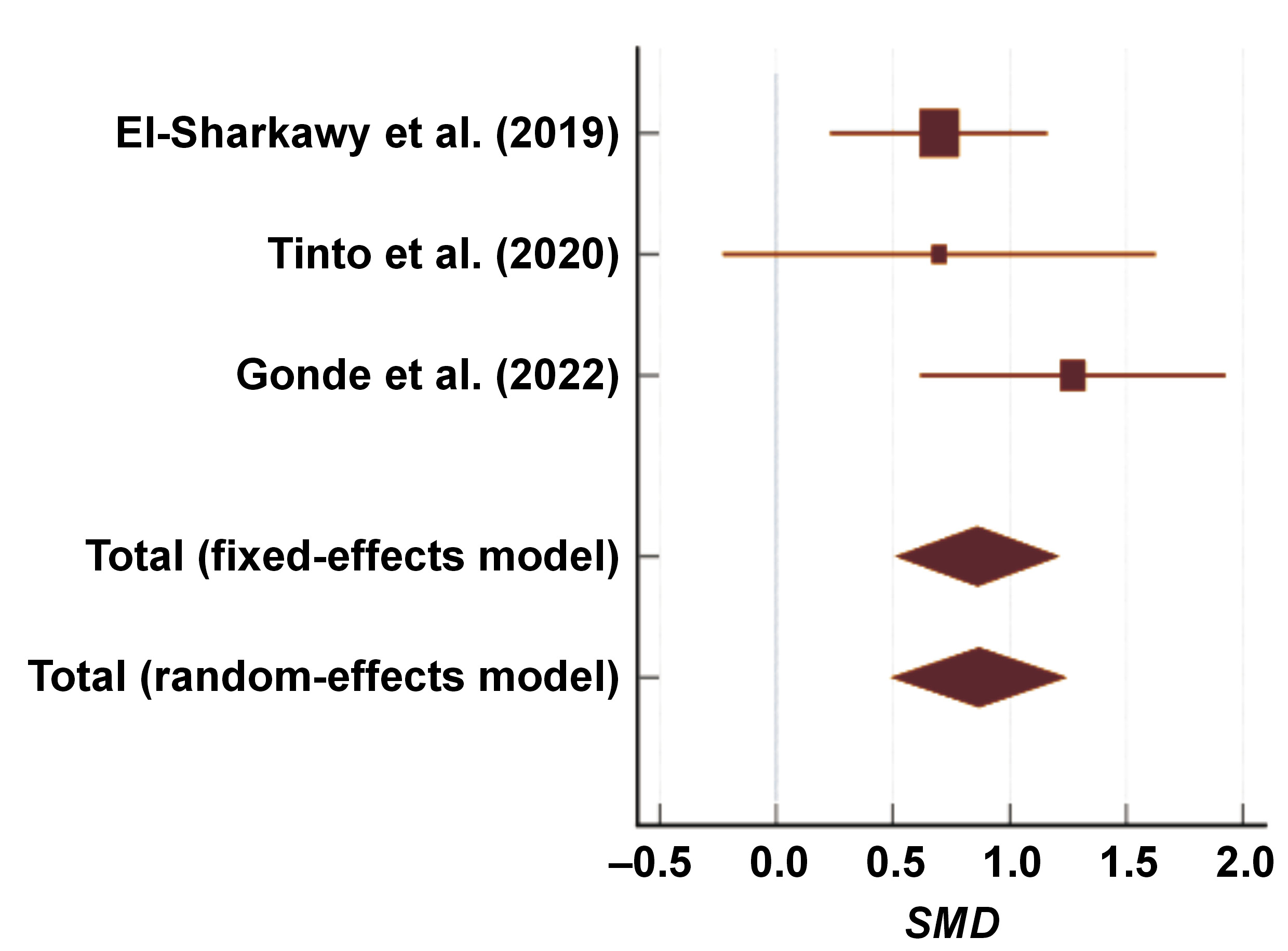
Melatonin and PD
The estimated overall effect (i.e., pre–post reduction in PD) expressed as standardized mean difference (SMD) for the aggregate sample of 70 subjects from 3 studies was 0.862 for the fixed-effects model and 0.869 for the random-effects model (Table 2).
Both estimates were comparable, with overlapping 95% CIs. However, the estimate for the fixed-effects model was reported due to the non-significant heterogeneity (p > 0.331) and minimal inconsistency, as indicated by the Q statistic and I2, respectively (Table 3). The forest plot presents individual and overall estimated SMD values for fixed-effects and random-effects models, along with respective 95% CIs (Figure 2).
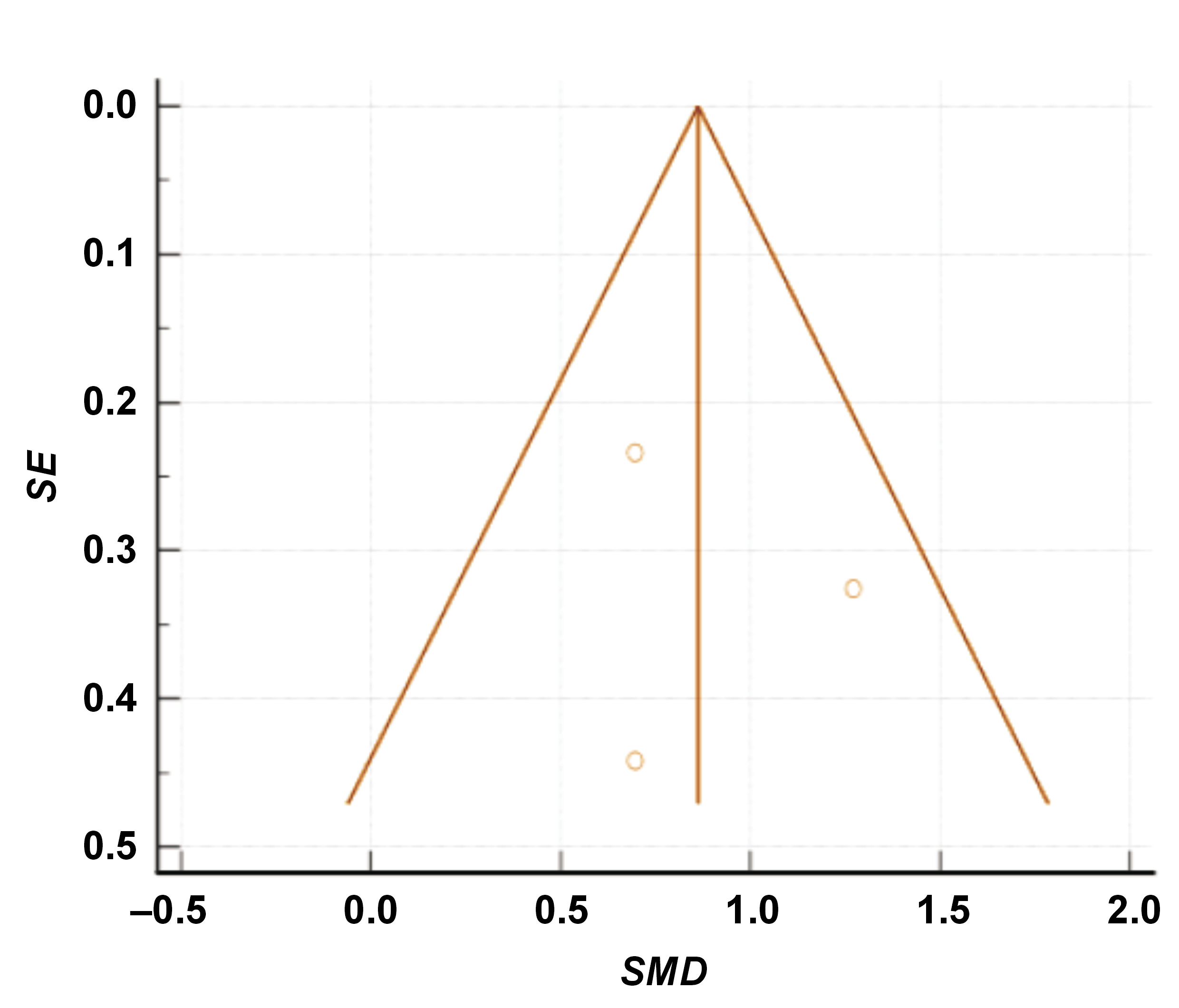
Publication bias
In the present meta-analysis, both Begg’s funnel plot and the Egger’s test were used to evaluate the publication bias. The funnel plot revealed no effect of the publication bias on the summary measure (i.e., SMD in PD from baseline to 6 months) plotted versus respective standard errors from all 3 studies (Figure 3). The results of the Egger’s test (p = 0.823) and Begg’s test (p = 0.602) were non-significant (p > 0.05), indicating an absence of the publication bias (Table 3).
Discussion
Periodontitis is a chronic inflammatory disease that affects the supporting structures of the teeth, including the gingiva, the periodontal ligament and the alveolar bone.1 The primary treatment approach for periodontitis is NSPT, which includes scaling and root planing. However, the use of adjunctive therapies to enhance the outcomes of NSPT has been explored in recent years. Melatonin, a hormone primarily involved in regulating sleep–wake cycles, has been identified as a promising adjunctive therapy due to its anti-inflammatory and antioxidant properties.2
The present systematic review and meta-analysis aimed to evaluate the effect of melatonin as an adjunct to NSPT in the treatment of periodontitis. The meta-analysis included 3 studies that measured periodontal parameters at baseline and after 6 months of treatment, comparing a melatonin-treated group to a control group.
The included papers showed variation in the patient population, as well as in the dosage and route of administration of melatonin. However, all studies assessed the clinical parameters of periodontitis, including PD, as well as biochemical parameters.
The baseline or pre-treatment PD measurements of the included studies ranged from 3.4 mm to 7.45 mm in the test group and from 3.00 mm to 6.95 mm in the control group. After 6 months of treatment, the PD measurements ranged from 2.3 mm to 3.95 mm in the test group and from 2.67 mm to 4.55 mm in the control group. The mean differences in PD between baseline and 6 months varied across the studies, with the test groups demonstrating generally greater reductions in comparison to the control groups.
A meta-analysis of the mean differences in PD between baseline and 6 months revealed that the use of melatonin as an adjunct to NSPT was associated with statistically significant improvements in periodontal parameters. El-Sharkawy et al. reported a mean difference of 2 mm in PD reduction in the test group compared to 1.4 mm in the control group.16 Tinto et al. demonstrated a mean difference of 1.37 mm in the test group compared to 0.73 mm in the control group.17 Gonde et al. noted a mean difference of 3.5 mm in the test group compared to 2.4 mm in the control group.18
These findings suggest that the adjunctive use of melatonin in NSPT may contribute to better clinical outcomes in terms of PD reduction. The anti-inflammatory and antioxidant properties of melatonin are believed to play a role in reducing periodontal inflammation and promoting tissue healing.4 Additionally, the positive effect of melatonin on sleep quality may indirectly contribute to better periodontal health, as poor sleep has been associated with increased susceptibility to periodontal disease.2, 3
It is important to note that the studies included in this meta-analysis had some limitations. The sample sizes were relatively small in some studies. Additionally, the heterogeneity of the study designs and patient populations makes it challenging to draw definitive conclusions. Well-designed RCTs with larger sample sizes are required to validate the findings of this meta-analysis and determine the optimal dosage and route of melatonin administration in periodontal therapy.
Based on the available evidence, the adjunctive use of melatonin in NSPT appears to have a positive effect on periodontal parameters, particularly in terms of PD reduction. However, further research is necessary to establish the optimal protocol for melatonin administration and to further explore its mechanisms of action in periodontal disease.
Limitations
The current evidence is derived from a limited number of RCTs and controlled clinical trials. Additional high-quality studies with larger sample sizes and longer follow-up periods are warranted to further validate these findings and determine the long-term effects of melatonin in periodontal therapy. Future research should focus on elucidating the optimal dosage, duration and timing of melatonin administration, as well as investigating its effects on other relevant clinical and inflammatory parameters.
Conclusions
The findings of this systematic review and meta-analysis provide evidence that the adjunctive use of melatonin in NSPT has a beneficial effect in the treatment of periodontitis. The analysis of the 3 included studies demonstrated that the addition of melatonin to NSPT resulted in significant improvements in PD compared to NSPT alone. The results of the study suggest that the incorporation of melatonin into the treatment regimen has the potential to enhance the outcomes of NSPT and contribute to the management of periodontal disease.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.