Abstract
Background. Cleaning overdentures is challenging due to their complex metallic structures, which often create small and irregular areas that are difficult to clean. Thus, it is necessary to find an effective and safe method for their maintenance.
Objectives. The aim of the study was to evaluate the effects of hygiene methods on the dimensional changes and retention force of the O-ring system over a simulated two-year period.
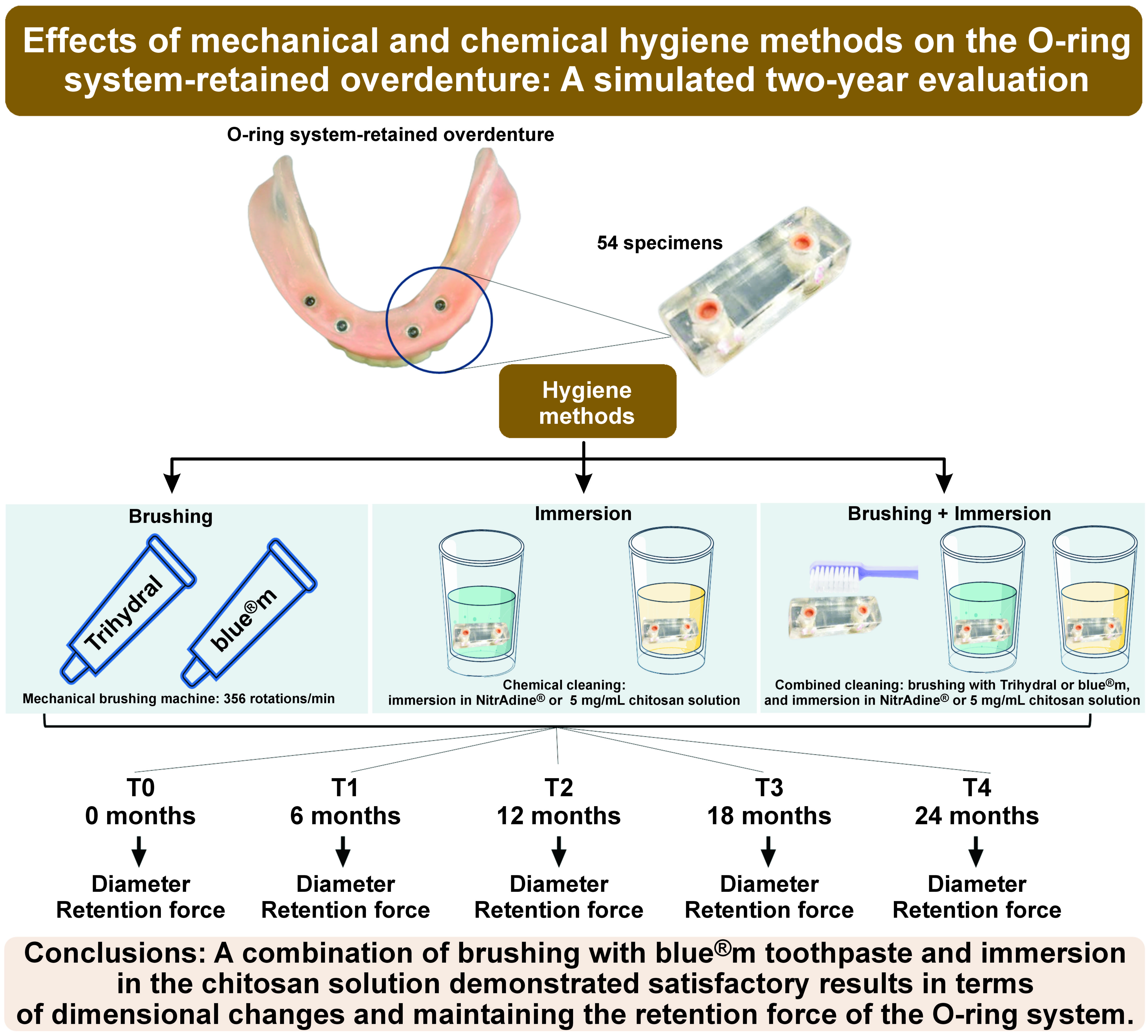
Material and methods. A total of 54 specimens with 2 O-rings each were distributed into 9 groups: control – no cleaning; brushing – blue®m toothpaste (BM); brushing – Trihydral toothpaste (TR); immersion – NitrAdine® (Ni); immersion – 5 mg/mL chitosan solution (Ch); and combined methods: BM+Ni, BM+Ch, TR+Ni, TR+Ch. The deformation and retention force were evaluated every 6 months for 2 years. The statistical analysis was performed using two-way analysis of variance (ANOVA) and Pearson’s correlation test (α = 0.05).
Results. The BM+Ch group exhibited smaller changes in diameter after 6 months (Δ(T1–T0)) than the control and BM+Ni groups, both internally and externally (p < 0.001). In addition, the BM+Ch group demonstrated greater retention forces at 6 months (p = 0.024) and 18 months (p = 0.028) in comparison to the TR+Ch group. The TR+Ch group exhibited a negative correlation with changes in the external diameter (r = −0.334, p = 0.021), while BM+Ch showed a negative correlation with changes in the internal diameter (r = −0.334, p = 0.021). The Ni group demonstrated a negative relationship with changes in both the internal (r = −0.296, p = 0.041) and external diameters (r = −0.405, p = 0.004).
Conclusions. A combination of brushing with blue®m toothpaste and immersion in the chitosan solution demonstrated satisfactory results in maintaining the retention force of the O-ring system.
Keywords: denture cleanser, prosthodontics, toothpastes, dental prosthesis
Introduction
Edentulism remains a prevalent condition affecting a significant portion of the population. Among the available options for oral rehabilitation, the use of overdentures has emerged as an excellent alternative to conventional complete dentures. Overdentures offer various advantages, including the prevention of soft tissue injuries, enhanced retention, stability, masticatory function, phonetics, and esthetics. Success rates for overdentures range between 94% and 100%.1
The O-ring system comprises an attachment connected to the implant and a metallic capsule with an internal silicone ring that is retained in the prosthesis.2 This system effectively distributes masticatory forces among the supporting structures and is favored by patients due to its ease of insertion and removal.2
Proper hygiene of overdentures is crucial for the success and longevity of the treatment.3, 4, 5 Regular recalls and maintenance of gingival health are also essential.6 The literature describes various hygiene protocols, with mechanical hygiene (brushing) being the most commonly used method, and the combined approach involving both mechanical and chemical methods as the most effective in eliminating biofilm and preventing periodontal disease.7, 8, 9, 10, 11, 12, 13, 14, 15, 16 Therefore, the significance of denture cleansers and toothpastes in maintaining oral health cannot be neglected.17, 18
Given the absence of conventional toothpastes designed for the maintenance of overdentures, the present study focuses on products such as Trihydral and blue®m, which are suitable for both prosthesis and oral cavity hygiene without causing metal degradation. Effervescent tablets for dentures, particularly NitrAdine®, have been frequently recommended as a chemical hygiene method. NitrAdine® has demonstrated effectiveness in cleaning removable partial dentures containing metal, as well as overdentures.19, 20, 21 However, since overdentures are composed of various materials, and few studies have examined the effects of cleansers on these prostheses,8, 22, 23, 24, 25, 26 it is necessary to evaluate the efficacy of denture cleansers to recommend an effective and safe method for patients with overdentures. A recent systematic review indicated that hygiene solutions have the most significant impact on retention for the bar–clip attachments in different materials.27
To explore alternative immersion solutions that are natural, easy to use, accessible, and cost-effective, researchers have investigated the potential of chitosan. Chitosan, a natural biopolymer with proven antimicrobial properties, is found in abundance in nature and has been applied in various fields, including pharmaceuticals, foods, cosmetics, and chemicals.28, 29, 30, 31, 32
Despite the significance of overdenture hygiene, a consensus on the most effective hygiene method remains elusive.33 Studies have reported conflicting outcomes with the use of effervescent tablets,5, 21 sodium bicarbonate/sodium perborate,34 mouthwash containing cetylpyridinium chloride and fluoride, and sodium hypochlorite, with consequent changes in the surface of the O-ring capsules.24, 25, 35 However, while the combined mechanical and chemical hygiene method is regarded the most suitable for the hygiene of dentures, there is a paucity of literature addressing its application in overdentures.36, 37, 38
The present study aims to evaluate the effects of isolated and combined hygiene methods on the dimensional changes and retention force of the O-ring system over a simulated two-year period. The null hypothesis posits that the utilization of these methods will not have a significant influence on the O-ring diameters or retention force.
Material and methods
Experimental design
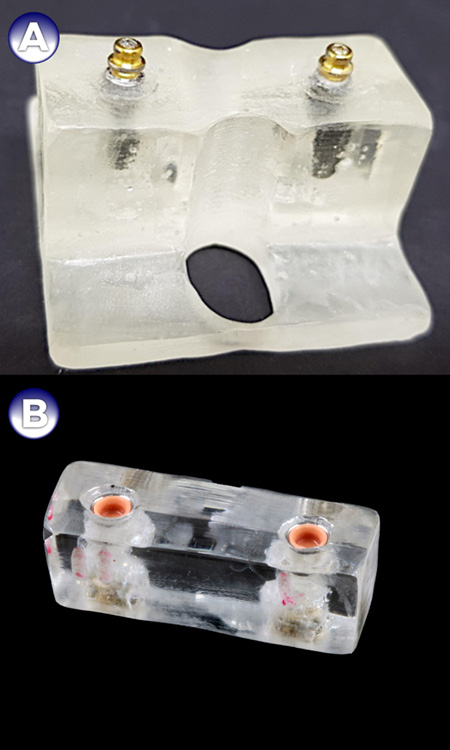
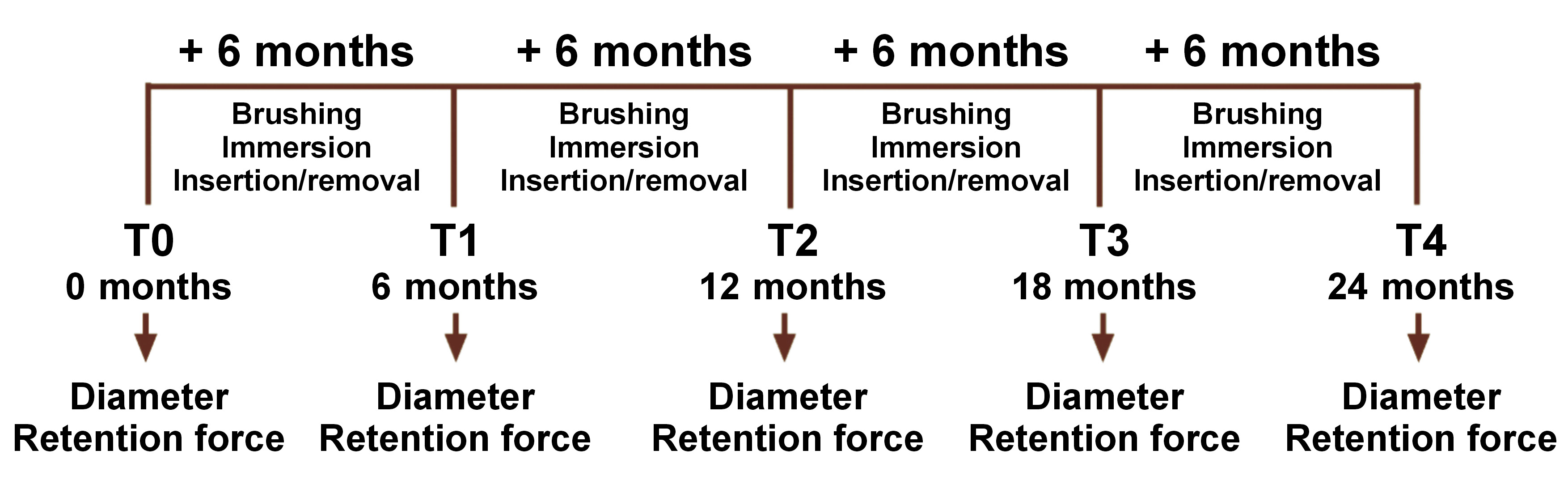
Fifty-four specimens of acrylic resin simulating prosthetic bases, with 2 O-rings each, were obtained39 and articulated. Each base contained 2 implants (grand morse™; Neodent Serviços Odontológicos LTDA, Curitiba, Brazil). In a previous study, the data indicated that the difference in the response of matched pairs is normally distributed with a standard deviation (SD) of 0.88.35 If the true difference in the mean response of matched pairs is 1.38, 5 pairs of subjects would be needed to reject the null hypothesis that this response difference is 0 with a probability (power) of 0.8. The type I error probability associated with this test of the null hypothesis is 0.05. Thus, 6 specimens per group were selected based on the sample size of studies employing the same methodology.35, 36, 37
The specimens were divided into 9 groups (Table 1). Each group, encompassing 6 samples, underwent a hygiene process and had outcomes measured at 4 different times. The selected O-ring contains the pink O-ring rubber (code 102.107), which the manufacturer specifies as having low retention. The resin bases with the implants (Figure 1) were obtained from condensation silicone impressions (Perfil; Vigodent SA Indústria e Comércio, Rio de Janeiro, Brazil) of metallic bases. The O-ring retainers were installed over the implants with a torque of 20 Ncm.35
Initial measurements
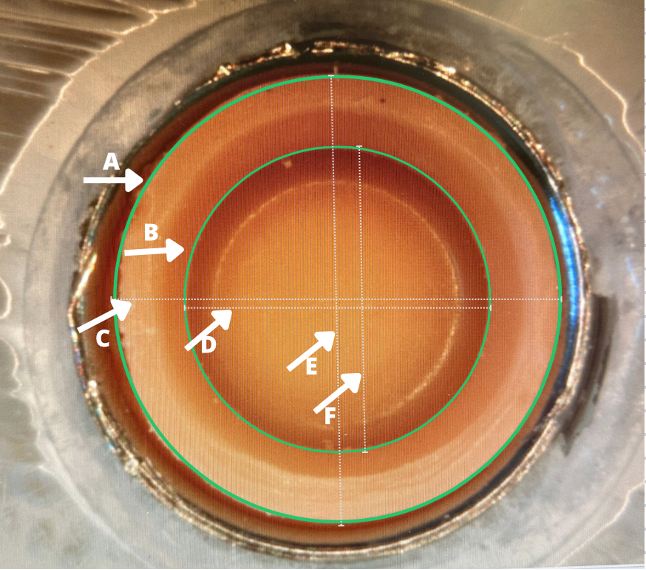
Before simulation, measurements were obtained through stereomicroscopic analysis (SMZ800; Nikon, Melville, USA). The O-rings were subjected to a visual examination, and images were captured using the NIS-Elements for Basic Research software (Nikon) at a magnification of ×20 to evaluate any dimensional changes that occurred due to the cleaning procedures. The horizontal and vertical distances of the internal and external diameters of the O-rings were measured as demonstrated in Figure 2.
The specimens were also subjected to the retention force analysis using a mechanical testing machine equipped with a 196-N load cell. The machine performed 20 insertion/removal cycles per minute,38 resulting in 216 readings (9 groups × 4 times × 6 repetitions). The base that simulated the mandible was fitted and fixed in an acrylic container filled with water at 37°C. Subsequently, the testing machine performed the insertion and removal of the specimen in the base.
The experimental design of the study is presented in Figure 3.
Cleaning
Mechanical hygiene
The mechanical cleaning method involved the use of an artificial brushing machine to standardize the strength and frequency of the brushing (MAVTEC Brush Simulator; Mavtec Comércio de Peças Acessórios Serviços Ltda ME, Ribeirão Preto, Brazil). Additionally, soft-bristle toothbrushes (Colgate Slim Soft; Colgate-Palmolive Company, Rio de Janeiro, Brazil) were utilized. Two types of toothpaste were used: blue®m (Bluem Brazil, Curitiba, Brazil); and Trihydral (Perland Pharmacos Ltda, Cornélio Procópio, Brazil). The toothpastes were suspended in distilled water at a ratio of 1:1 (Table 1).18, 40 To calculate the brushing time at the frequency of 356 rotations per minute, 8,600 cycles were performed, which corresponded to 6 months of brushing exposure. This cycle was repeated until 2 years of use. The toothbrushes and toothpaste solutions were replaced at the conclusion of each 6-month cycle.12, 39
Chemical hygiene
Two methods for the chemical hygiene of overdentures were employed. The first technique involved the immersion of the specimens for 12 h in a solution containing effervescent tablets (NitrAdine®; MST Laboratories AG, Vaduz, Liechtenstein) diluted in 150 mL of water at an average temperature of 37°C.41 This exposure is equivalent to a routine use of the product twice a week for 15 min, according to the manufacturer’s instructions, thereby simulating a period of 6 months. During the immersion, the solution was not changed because studies on the degradation curve of the tablet indicated that the product remains highly effective within the specified time frame.35
The second immersion method entailed the use of an experimental solution of chitosan at a concentration of 5 mg/mL.28 For this purpose, low molecular weight chitosan (Sigma-Aldrich, St. Louis, USA) was utilized. A daily 15-min immersion routine was simulated for a period equivalent to 6 months (42 h) (Table 2).
Combined hygiene methods
In the combined hygiene protocols, mechanical methods were first used, followed by chemical methods, as described in the methodology.38
Outcomes of interest
After each 6-month simulation period, measurements were conducted once more using stereomicroscopy (SMZ800; Nikon) as previously described.
The specimens were also subjected to the retention force analysis using a mechanical testing machine. A total of 720 cycles were performed to simulate 6 months of denture use, based on the assumption of 4 insertions and removals of the prosthesis by the patient per day.40 The force required for each insertion/removal cycle was recorded using the LabVIEW 8.0 software (National Instruments, Austin, USA) connected to the load cell of the testing machine.
Statistical analysis
The data analysis was performed using the IBM SPSS Statistics for Windows software, v. 21.0 (IBM Corp., Armonk, USA). The mean values, which exhibited a normal distribution as indicated by the Shapiro–Wilk test, were compared using two-way analysis of variance (ANOVA) and Tukey’s tests with Bonferroni correction. The Pearson’s correlation (r) test was applied to verify the correlation between the dimensional changes of the diameters and the retention force (α = 0.05 for all tests).
Results
The results of this study demonstrated that the dimensional changes of the internal (ID) and external diameters (ED) of the O-ring system were affected by immersion (p < 0.05), time (p < 0.001) and brushing techniques (p < 0.001). Likewise, the retention force was found to be time-dependent, exhibiting interactions with both immersion and brushing techniques (p = 0.005).
Immersion treatments demonstrated a better preservation of the ID (p = 0.012) in comparison to the absence of immersion, with the use of NitrAdine® yielding a smaller change in ID (26.2 μm (SD = 54.2)) after 6 months (Δ(T1–T0)) compared to the no immersion group, which exhibited a mean change of 40.4 µm (SD = 7.8) (p = 0.009). Similarly, changes in the ED were significantly less pronounced in the presence of NitrAdine®, with a mean change of −19.3 µm (SD = 12.3), in contrast to the no immersion group’s mean change of 12.0 µm (SD = 22.5) at Δ(T1–T0) (p = 0.004).
The brushing method analyses revealed distinct dimensional alterations. The application of Trihydral brushing without immersion led to an increase in the ID (p < 0.001), contrasting with the stabilizing effects of NitrAdine® and chitosan immersion. Brushing with blue®m without immersion resulted in a decrease in diameter measurements at Δ(T1–T0). Moreover, when used in conjunction with chitosan immersion, it exhibited a reduction trend in diameters in the ED (p ≤ 0.001) (Table 3).
The retention force analysis revealed a significant variation over time (p < 0.0001). The initial force (T0) of the O-rings, without immersion or brushing, was 14.41 ±2.69 N. In the subsequent temporal analyses, both NitrAdine® and chitosan immersions demonstrated enhanced retention forces compared to the non-immersion condition (p = 0.006 and p = 0.005, respectively). By the final time point (T4), the retention force in the chitosan immersion group exhibited less variance than that of the NitrAdine® group (p = 0.001). The application of Trihydral brushing demonstrated no significant differences between immersion types across all temporal frames (Table 4).
The correlation analysis between dimensional changes and retention force indicated a weak negative correlation among specimens immersed in NitrAdine®, where less dimensional change was associated with higher retention force (Table 5). These complex interactions were supported by the statistical analysis, according to the data provided in Table 3, Table 4, Table 5.
Discussion
The present study aimed to evaluate the dimensional changes in the internal and external diameters of the O-rings and the retention force before and after the application of different hygiene methods for overdentures. The results indicated that the null hypothesis was not accepted, as the evaluated hygiene methods promoted deformations in the capsules and changed the retention force at the different times analyzed. This highlights the influence of the hygiene method on the properties of O-rings. The present study focused on the evaluation of O-ring systems, which are widely accepted by patients because they are easy to insert and remove, simple to clean, improve quality of life, and allow for effective distribution of forces.3, 4, 5 Previous studies have demonstrated that the retention of systems can be affected by different hygiene solutions.4, 21, 24, 25, 27, 34, 42 Additionally, color changes in the retentive elements have also been reported.25, 42, 43, 44
Regarding the retention force, the combination of blue®m toothpaste and chitosan solution demonstrated optimal outcomes. This combination proved effective in preserving the dimensions and the retention force of the O-ring system. The use of a 5 mg/mL chitosan solution as a complementary chemical method, in addition to brushing, appears to be a promising approach. Chitosan, an abundant and affordable substance of animal origin, has been considered a favorable option for denture hygiene due to its non-toxic nature, biopolymer properties, and proven antimicrobial action.30, 33 The necessity for easily accessible products, coupled with the prevalence of chitosan in nature, has led to the development of blue®m, a product that is free from chemical components such as triclosan and fluoride. This toothpaste contains active oxygen and biological honey derivatives, and is characterized by a neutral pH, as reported by the manufacturer. It is recommended for oral cavity hygiene and for use with overdentures, as it is purported to not cause adverse effects, such as oxidation, on prosthetic components.
The denture retention is directly related to patient satisfaction and chewing difficulties, which can necessitate the replacement of the retaining component of the prosthesis and frequent returns to the dental office for maintenance.
In relation to the dimensional changes, brushing with Trihydral in conjunction with immersion in NitrAdine® as well as brushing with blue®m followed by the immersion in a chitosan solution resulted in the smallest dimensional changes in the O-ring diameter. Trihydral toothpaste does not contain highly abrasive particles that could cause prosthesis wear. Its active ingredient, chloramine-T, has antiseptic and biocidal properties, and has been used as a periodontal surgical adjuvant.43 It exhibits excellent biofilm-penetrating properties and effectively neutralizes bacteria, while also inhibiting gum inflammation and promoting tissue regeneration and repair.43, 44 Martinez et al. conducted a systematic review and meta-analysis to evaluate the effectiveness of effervescent tablets in cleaning and sanitizing removable dentures compared to other chemical and physical methods.45 The authors assessed biofilm reduction, microbial levels and material stability. The study concluded that the combination of brushing with the use of an effervescent tablet yielded significantly better results.45 According to many studies, the NitrAdine® effervescent tablet has antimicrobial properties and is compatible with cobalt–chromium metal alloy.19, 20, 35
A study by de Campos et al. stated that overdentures are subject to loss of retention when undergoing continuous insertion and removal of the prosthesis.46 The authors highlighted several factors that can influence the efficacy of overdentures, including implant angulation, implant type, connector size, retainer depth, and retainer material. However, they did not evaluate the impact of cleaning agents.46 Overdentures are considered to be relatively easy to clean; nevertheless, there is currently no ideal product that could be recommended for their hygiene.47, 48, 49
The results of this study demonstrate that the retention values of the control group were less satisfactory, suggesting that the hygiene method played a crucial role in maintaining adequate retention force. Even with the wear resulting from the insertion and removal of the prosthesis, the efficacy of the cleansers in protecting the retainers likely contributed to the enhanced retention observed in these cases. All groups exhibited higher retention force in comparison to the control group. A comprehensive analysis of the temporal dimension, coupled with the examination of the internal and external diameters of the O-rings, revealed that all groups, including the control group, exhibited dimensional changes over time, characterized by an increase or decrease in diameter. In a study by Ayyıldız et al., the effect of effervescent tablets was evaluated.23 The results indicated that their use resulted in lower changes compared to the control group.23 Effervescent tablets have been proposed for patients with implant-retained overdentures.19, 20 These findings are consistent with the results of other studies that have demonstrated the preservation of retainer system characteristics by cleansers.22 Varghese et al. showed that the use of Polident for 5 min did not significantly alter the properties of the O-ring, while Fittydent and chlorhexidine gluconate resulted in an increase in its retention force when compared to the control group.22
In the present study, a weak negative correlation was observed between the dimensional changes of the internal and external diameters and the retention force after immersion in NitrAdine®. However, the mechanisms of retention loss cannot be solely explained by dimensional and surface changes, as not all groups that experienced retention loss exhibited significant dimensional changes. These results corroborate the findings of Rutkunas et al., who used scanning electron microscopy to evaluate the effects of wear on overdenture retainers and concluded that not all groups exhibiting retention loss demonstrated substantial dimensional changes.47 The changes in the physical and mechanical properties of the O-ring, such as decreased flexibility, may contribute to maintaining the retention force during the use of prosthesis.
Limitations
This study was subject to certain limitations, as it was conducted in vitro and did not evaluate the effect of chewing cycles on the retainers. In clinical settings, chewing forces, as well as patient forces and the insertion axis involved in prosthesis removal and insertion, can undergo changes. Additionally, thermal cycling was not performed, and it is acknowledged that the conditions of the oral cavity can influence the results, as thermal and pH changes can alter the retention force.23 The present study is a pioneering analysis of the combination of mechanical and chemical methods for the hygiene of overdentures, aiming to provide guidelines for improving denture hygiene and informing professionals about the safety of overdenture hygiene. The evaluated methods had satisfactory effects, as they ensured the stability of the O-ring properties within acceptable limits. However, further studies, particularly clinical trials, are necessary to evaluate not only the antimicrobial activity, but also the potential deleterious effects on different surfaces of overdentures.
Conclusions
This study contributes to the understanding of the effects of different cleaning methods on the dimensional changes and retention force of O-rings in implant-supported overdentures. The findings suggest that the combination of brushing with blue®m toothpaste and immersion in a chitosan solution can yield satisfactory results in terms of overdenture hygiene and retention force. Further research is warranted to explore the clinical applicability and long-term effects of these hygiene methods on the overdentures.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.