Abstract
Background. Odontomas are odontogenic tumors located in the jawbone, referred to by the World Health Organization (WHO) as hamartomatous (Greek hamartion – a bodily defect) developmental malformations. The term was first used by Brock in 1866 to refer to every odontogenic tumor. Today an odontoma is believed to be a congenital malformation of dental hard tissues. Odontomas can contribute to the development of dental abnormalities and bite disorders.
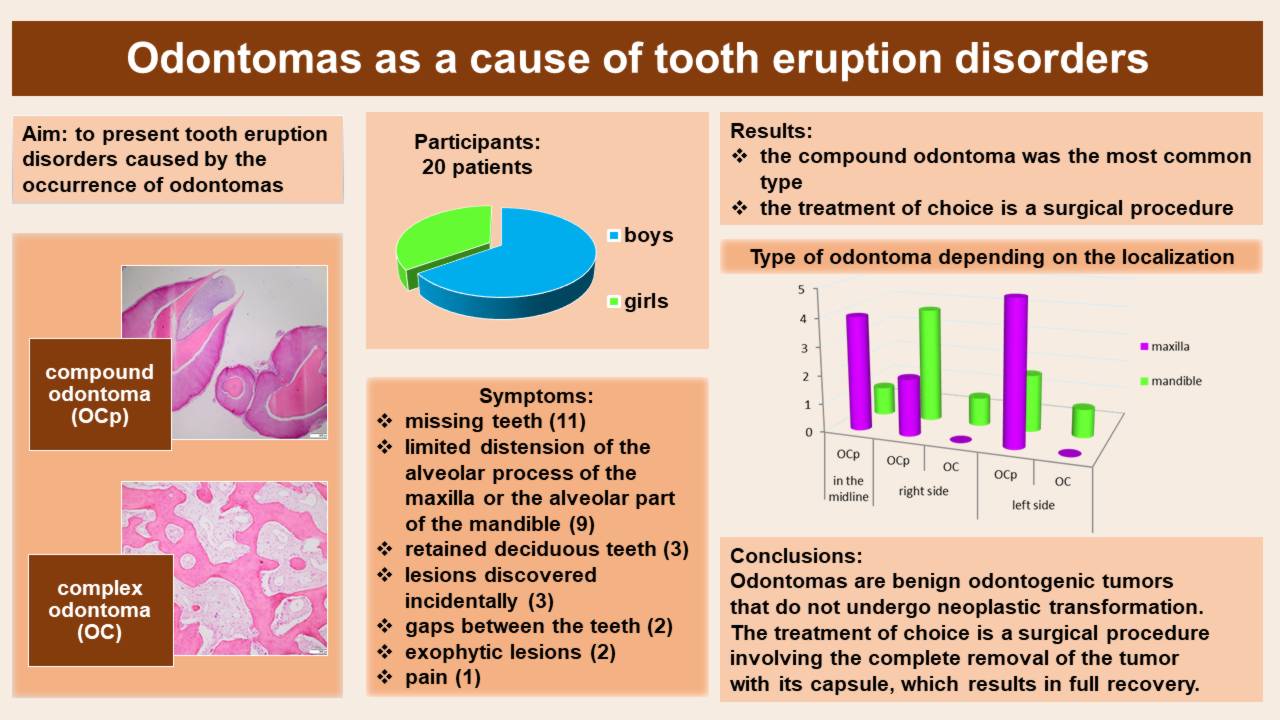
Objectives. The study aimed to present tooth eruption disorders caused by the occurrence of odontomas in 20 patients treated at the Dental Surgery Clinic for Children.
Material and methods. The study group comprised 20 patients (13 in good general health, 6 with systemic diseases and 1 with a congenital malformation), aged 2–17 years (mean age: 8.96 years), with jawbone odontomas diagnosed through clinical and radiological examination. These odontomas were the cause of disorders in the eruption of deciduous and permanent teeth. The treatment method applied in all patients involved the enucleation of the tumor with its capsule and sending the material for histopathological examination.
Results. Odontomas were discovered accidentally or were accompanied by such clinical symptoms as retained deciduous teeth, impacted deciduous and permanent teeth, missing teeth in the oral cavity, gaps, displaced teeth, and the distension of the alveolar process of the maxilla/alveolar part of the mandible. The odontomas occurred in both the maxilla and the mandible, more often in boys. The compound odontoma (OCp) was the most common type.
Conclusions. Odontomas are benign odontogenic tumors that do not undergo neoplastic transformation. The treatment of choice is a surgical procedure involving the complete removal of the tumor with its capsule, which results in full recovery.
Keywords: children, oral surgery, orthodontics, dental anomalies, tumors
Introduction
Odontomas are among the most common odontogenic neoplasm-like tumors of the jawbone.1, 2 They are not typical neoplasms, as they are only hamartomatous developmental malformations.3 According to the literature, they most frequently occur in the 2nd and 3rd decades of life, though they are also not infrequent in the 1st decade.4 Their etiopathogenesis has not been fully explained and there are a number of theories concerning the origin of odontomas, such as traumas, infections, genetic disorders, or anomalies in the development of the tooth bud.3, 4, 5 Odontomas are often discovered incidentally, as they rarely cause pain. The most common reasons for their discovery are retained deciduous teeth, impacted deciduous and permanent teeth, missing teeth in the oral cavity, gaps, displaced teeth, and the distension of the alveolar process of the maxilla/alveolar part of the mandible. Odontomas usually have a diameter not exceeding 3 cm.1 Since they are odontogenic tumors, they contain an epithelial and mesenchymal component. The World Health Organization (WHO) divides them into 2 groups: complex odontomas (OC); and compound odontomas (OCp).6, 7, 8 The complex odontoma is a hamartomatous developmental lesion in which structures such as enamel, dentin, and sometimes cementum are arranged chaotically.4 The compound odontoma is an encapsulated developmental hamartomatous malformation containing numerous denticles – odontoids. In the case of OCp, structures such as enamel, dentin, cementum, and pulp are arranged in an organized fashion, so they resemble a properly formed tooth.4, 9 Some authors distinguish another variant – erupted odontoma – in the past referred to as peripheral odontoma. It is a variant of OCp that erupts in the oral cavity.4, 5
In histological examination, individual tooth tissues like enamel, dentin, cementum, and pulp can be distinguished.9 Diagnostic methods include radiological imaging – tooth X-rays, panoramic radiography, cone-beam computed tomography (CBCT) and/or computed tomography (CT). The treatment of choice is a surgical procedure involving the enucleation of the tumor with the capsule around it.2, 4, 9
The study aimed to present a type of tooth eruption disorders caused by the occurrence of odontomas, as well as treatment methods for odontomas in children and adolescents.
Material and methods
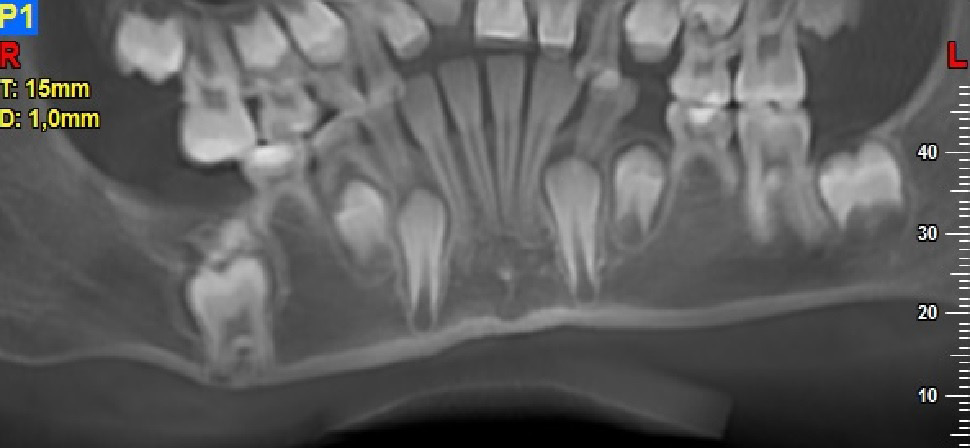
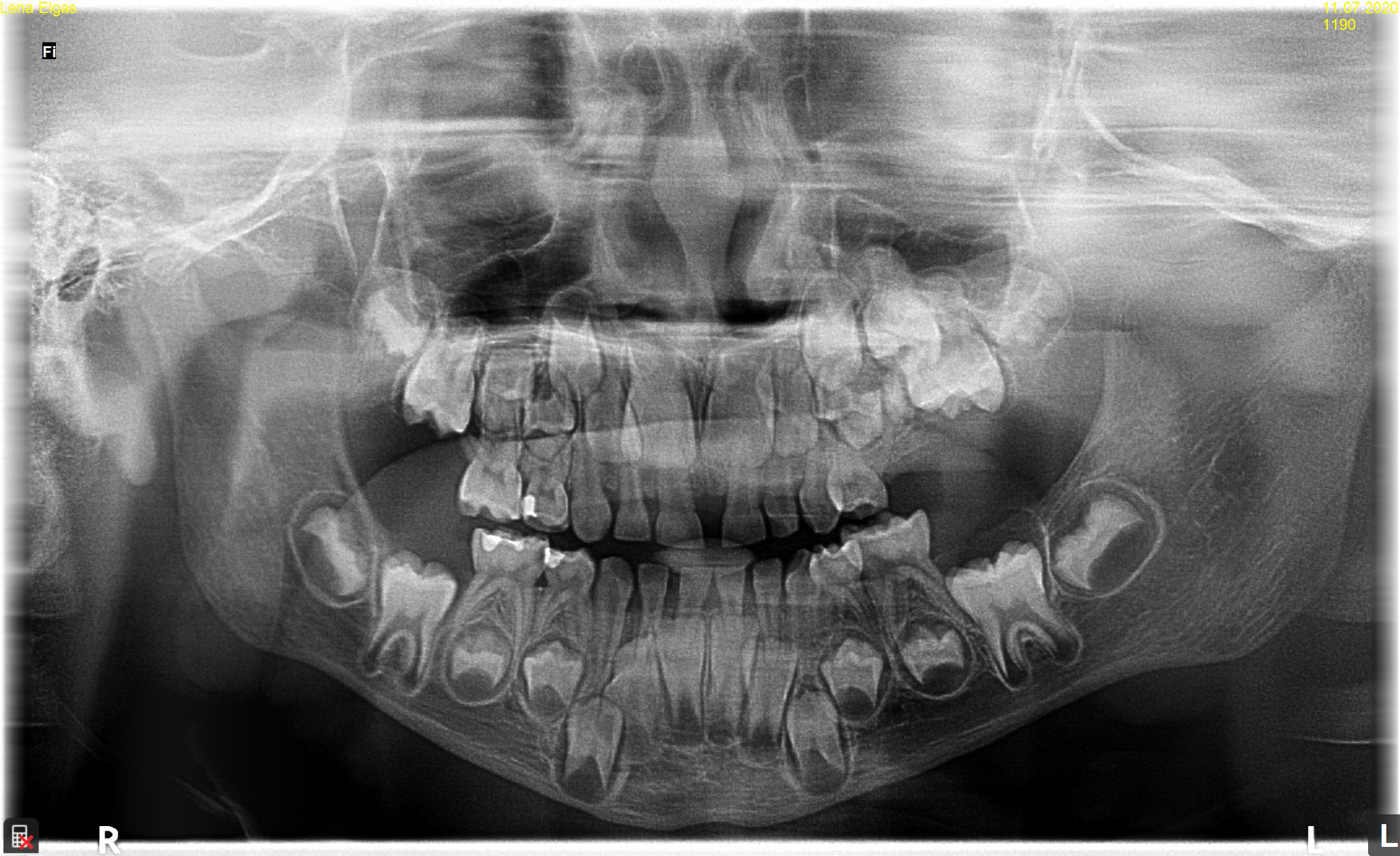
A total of 20 patients (13 (65%) boys and 7 (35%) girls), aged between 2.8 and 17.6 years (mean age: 8.96 ±4.20 years), were included in the study. The study involved general and local history-taking concerning chronic comorbidities and the medications received, dental history (the reason for the visit, presenting complaints), and extraoral (facial symmetry and lymph nodes) and intraoral (the number and type of erupted teeth, the assessment of the shape and consistency of the alveolar process) clinical examination. All patients underwent radiological and histopathological examination. Depending on the indications, tooth X-rays, panoramic radiography, CBCT and/or CT were performed. Radiological imaging was used to assess the location and type of odontoma, the presence of impacted or retained teeth, gaps, and tooth displacement. While OCp were found in X-ray images as high-density radiopacities arranged as numerous small deformed denticles (odontoids) surrounded by a band of radiolucency with an osteosclerotic border, OC were characterized by irregular radiopacities with a radiolucent edge and an osteosclerotic rim. The treatment of choice for all patients was the enucleation of the tumor with the capsule surrounding it.
Results
Six participants (30%) had a diagnosis of a systemic disease: nephritic syndrome; bicuspid aortic valve (BAV) dysfunction; epilepsy; atrial septal defect (ASD) II; autoimmune polyglandular syndrome (APS); and a history of chemotherapy for anaplastic ependymoma. One patient (5%) had a congenital malformation – cleft lip and cleft palate. The remaining patients were in good general health. Eight children (40%) had deciduous teeth, and 12 (60%) had permanent or mixed dentition (Table 1).
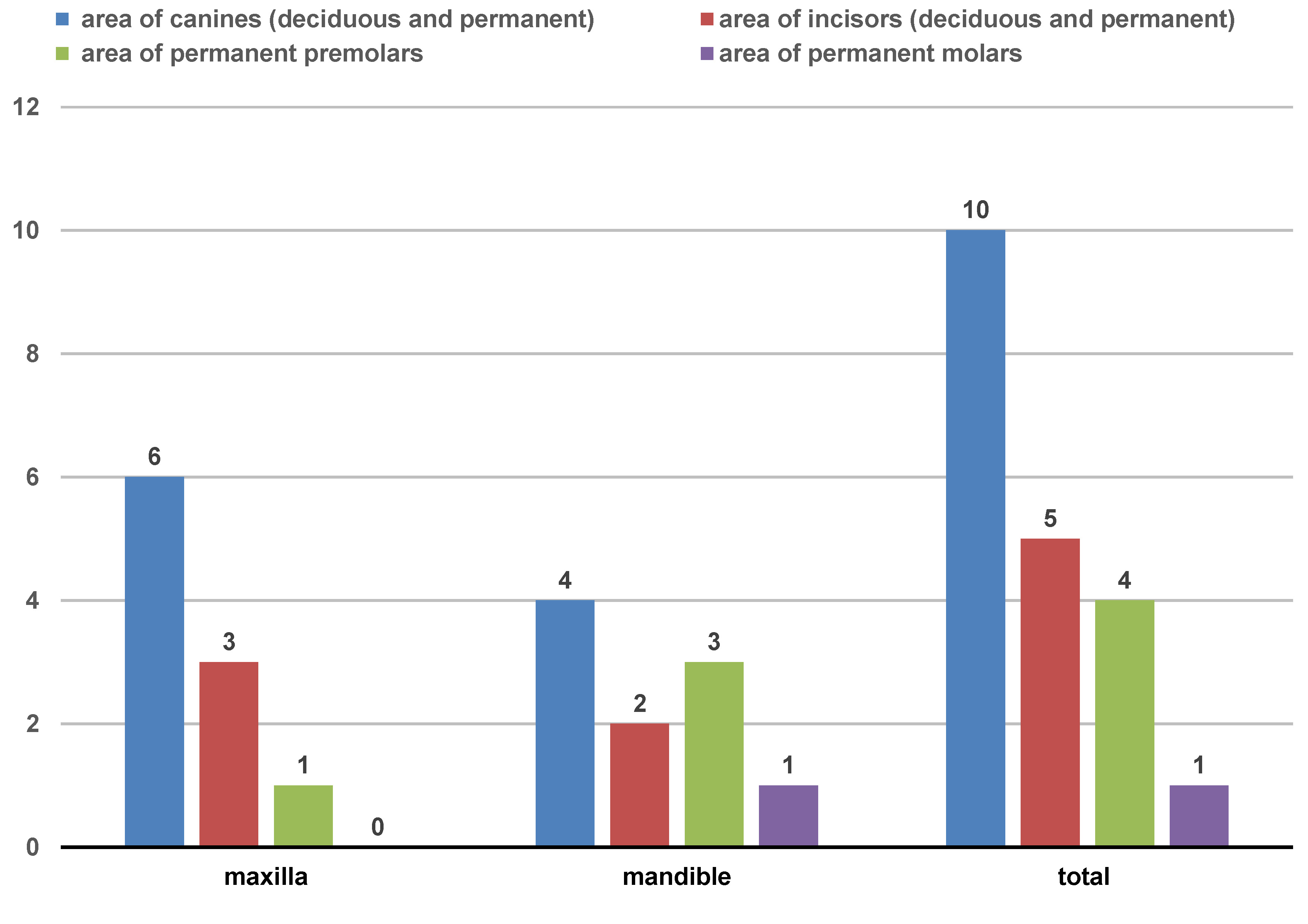
All patients were referred for diagnostic examination by dentists: 11 (55%) of them due to missing teeth; 3 (15%) due to retained deciduous teeth; 9 (45%) had limited distension of the alveolar process of the maxilla or the alveolar part of the mandible; 2 (10%) had gaps between their teeth; 1 (5%) experienced pain; 2 (10%) had exophytic lesions; in 3 patients (15%), the lesion was discovered incidentally in plain radiography. Some patients had 2 or more symptoms simultaneously, for example, gaps between the teeth and the distension of the alveolar process of the maxilla or the alveolar part of the mandible (1 (5%)) or an impacted tooth and the distension of the alveolar process of the maxilla or the alveolar part of the mandible (2 (10%)). Most patients reported no pain. Only one boy at the age of 3.6 years reported moderate pain of a distending and continuous nature. In 2 boys (aged 2.8 and 3.6 years), changes in facial features in the form of cheek protrusion were observed. The buccal skin in the area of the lesions was unaffected, without signs of inflammation. None of the participants had palpable or painful submandibular lymph nodes. The most common intraoral symptoms included the absence of a deciduous or permanent tooth typical for the patient’s age despite the presence of a corresponding tooth on the other side, and alveolar process enlargement (protrusion, a gap between the teeth). Five of the 9 patients with alveolar enlargement also lacked a tooth typical for their age, of which 1 child was from the group with deciduous teeth (1/5) and 4 children were from the group with mixed/permanent dentition (4/5). Nine patients were lacking a single tooth, the remaining 2 (each of them) were lacking 2 teeth (teeth 71 and 81, 43 and 44). The most commonly missing teeth were deciduous or permanent canines. Radiological examination showed that all the missing teeth were impacted. In 3 patients from the group with mixed/permanent dentition, the absence of a tooth was accompanied by the presence of retained deciduous tooth/teeth (teeth 61, 73, 84, and 85). Lesions were more frequently observed in the maxilla (55%), predominantly in the area of canines (50%) and incisors (25%), and they were least frequent in the lateral segment (25%) (Table 1, Figure 1).
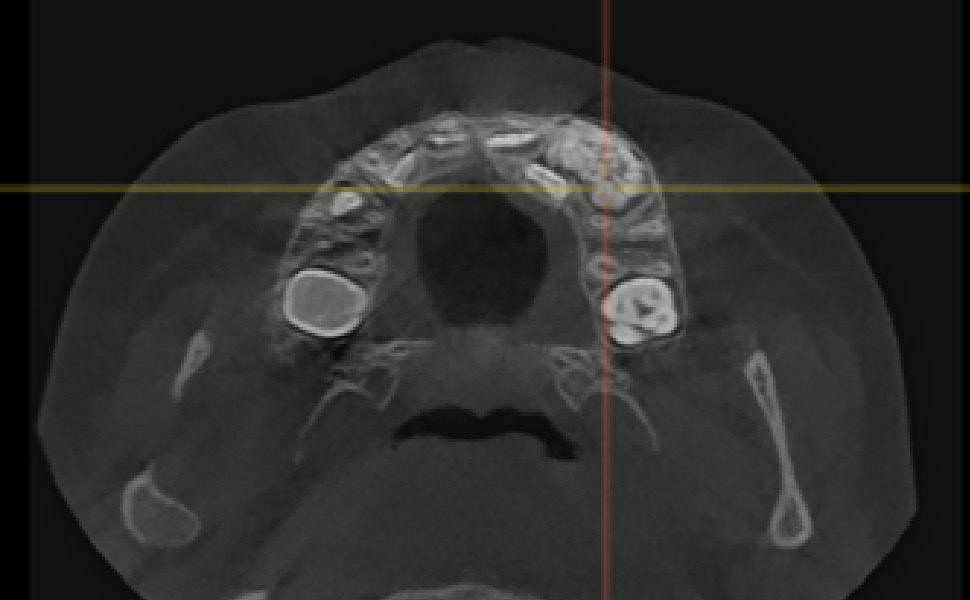
The patients had the following examination performed: tooth X-ray (11 (55%)); panoramic radiography (11 (55%)); CBCT (12 (60%)); or CT (1 (5%)). X-ray images revealed 18 OCp (of which 2 were described as erupted) and 2 OC.
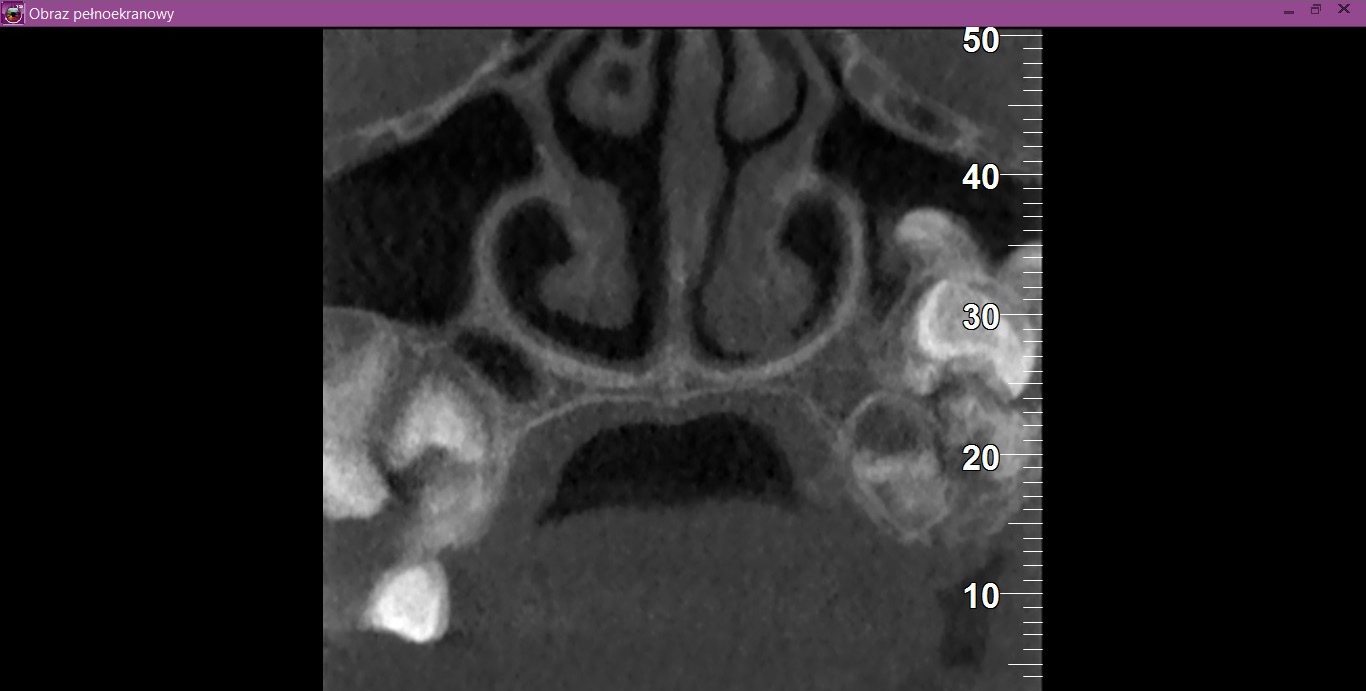
In 11 patients (55%), odontomas occurred in the maxilla – 4 (20%) in the midline, 5 (25%) on the left side (Figure 2) and 2 (10%) on the right side, and they were all OCp, of which 1 (5%) on the right side was an erupted odontoma. Nine patients (45%) were diagnosed with lesions in the mandible, with 5 (25%) of them having lesions on the right side (including 4 (20%) OCp and 1 (5%) OC) (Figure 3), 3 (15%) of them with lesions on the left side (1 (5%) OCp, 1 (5%) OC and 1 (5%) erupted odontoma) and 1 patient (5%) with OCp in the area of incisors.
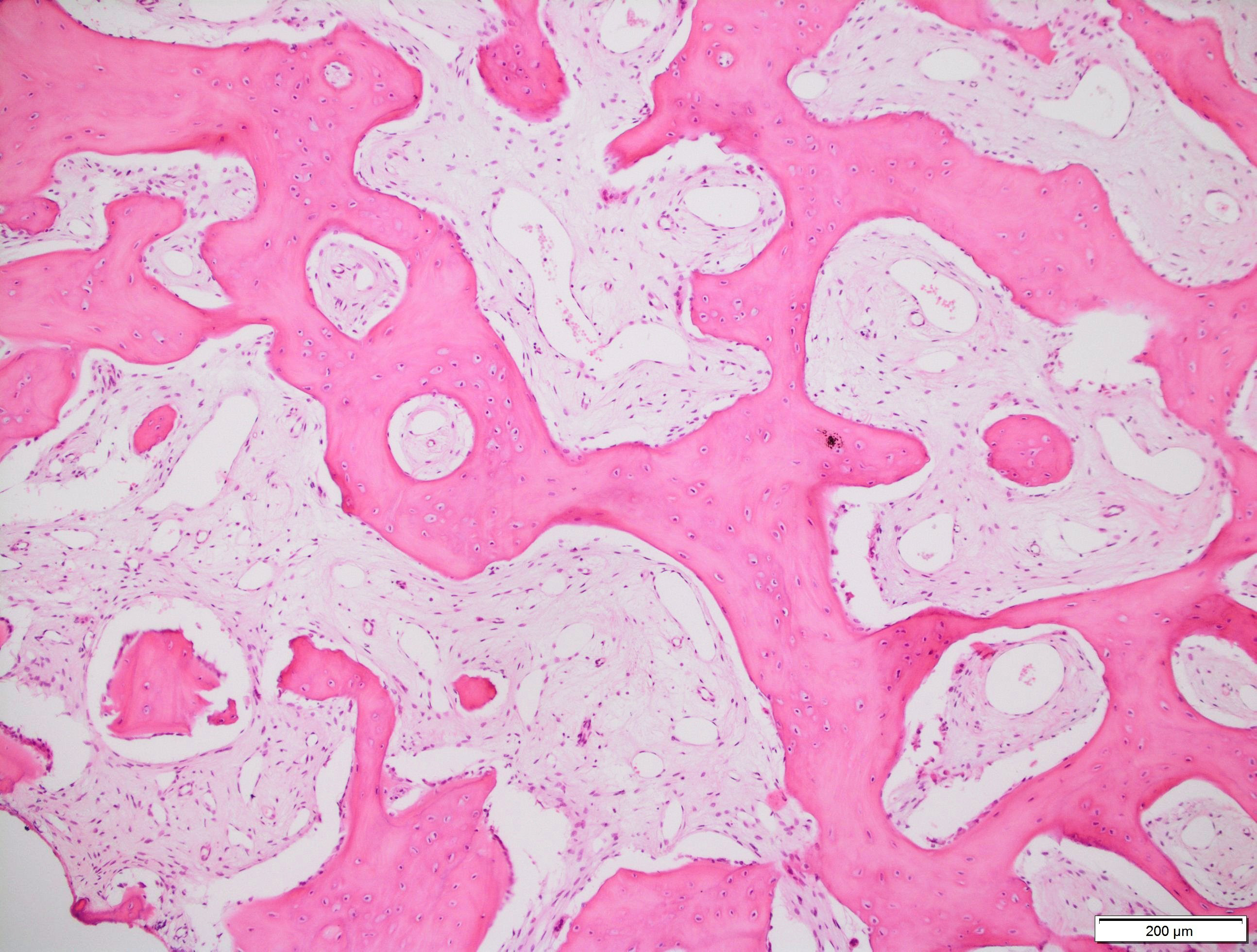
In the case of all patients, it was decided that their tumors and the capsules surrounding the tumors would be enucleated surgically in local or general anesthesia (depending on the patient’s age and cooperation). After the procedure, the patients received antibiotics – amoxicillin, or alternatively clindamycin in the case of an allergy to penicillins – at doses adjusted to the body weight (b.w.) and age of the child in mg/kg b.w./day, or at doses as for adults (more than 40 kg). The material was sent for histopathological examination. On microscopic examination, in 16 cases (80%), the lesions were described as OCp, 2 (10%) as OC, and 2 (10%) as erupted odontomas (visible in the oral cavity). Compound odontomas were described as fragments of the dental pulp, dentin, enamel matrix, epithelium with fragments of connective tissue, or fragments of a tooth with preserved histological structure, with fibrovascular tissue without epithelial covering and with foci of chronic inflammatory granulation tissue (Figure 4). Complex odontomas, on the other hand, were described as fragments of dentin and connective bone tissue (Figure 5).
Follow-up appointments were arranged for patients 1 day after the procedure, 1 week after the procedure, 1 month after the procedure, and then at 3 and 6 months after the first follow-up. On follow-up examinations, the wounds were observed to heal properly. After approx. 6 months, in 3 patients (15%), the impacted teeth were erupting or were situated higher as compared to their position during previous X-ray examinations. A 12-year-old girl who had 2 impacted teeth (the lower right first premolar 44 and the lower right canine 43), after 2 years from the procedure, had tooth 44 erupted and tooth 43 situated higher, but impacted by the crown of tooth 44. In another case of a 14-year-old boy who had the odontoma removed when impacted tooth 33 had completed root development, after about half a year, the impacted tooth did not change its position. Both patients were referred to an orthodontist and in both cases, the impacted teeth were orthodontically inserted into the dental arch. In no case was a recurrence observed after the removal of an odontoma.
Discussion
Odontomas account for approx. 22% of odontogenic tumors.1, 10 They are found mainly in deciduous and mixed dentition.3 Many authors claim that OCp are more common than OC.4, 9, 10, 11 On the other hand, according to Uma, OC are more common in older people, while OCp in the younger population.3 In our radiological and histopathological examinations, in the age group between 2 and 17 years, the OCp was the most common lesion – it was found in 16 patients (80%). Two patients (10%) were diagnosed with OC, and in 2 boys (10%), the lesions were visible in the oral cavity, and thus classified as erupted odontomas.
Khanum et al. mention one more variant of mixed odontoma (compound-complex odontoma), which they described in a 13-year-old boy.8 They reported it as an extremely rare type of odontoma, and their diagnosis was based on the histopathological examination showing that in some places, dental tissues were haphazardly arranged, and in other places, they presented regular, small tooth-like structures – odontoids.8
According to some researchers, the incidence of odontomas can be gender-specific.12, 13, 14, 15, 16, 17, 18 Uma in her article notes a predilection toward females in the case of OC, and OCp being more common in males,3 whereas Gedik and Müftüoğlu claim that odontomas of the maxilla are more often found in girls.11 In our study, OC were found in 1 boy (5%) and 1 girl (5%), and OCp in 10 boys (50%) and 6 girls (30%), which is inconsistent with the findings of Uma and Gredik and Müftüoğlu.3, 11
With regard to the typical locations of odontomas described in the literature, for OC, it is mainly the lateral section of the mandible and the anterior section of the maxilla, and for OCp, it is predominantly the anterior section of the maxilla.3, 4, 10, 19 In our study, similarly, OC were found in the posterior region of mandible (10%), while OCp was diagnosed in the mandible in 6 patients (30%), and in the maxilla – in 10 patients (50%), which points to its predominance in the maxilla.
According to Kale et al., odontomas occur more frequently on the right than on the left side (62% of OCp and 68% of OC), regardless of whether they are located in the maxilla or the mandible.10 In our patients, odontomas occurred on the left side – 8 (40%), on the right side – 7 (35%), and 5 (25%) of them in the midline, which does not confirm the findings of Kale et al.10
Amailuk and Grubor claim that traumas are among the causes of odontomas.5 The authors described a case of a 15-year-old boy from Sudan with OCp that was erupted, together with malformed crown and root of the upper left central incisor 21. It was decided that the odontoma and tooth 21 would be removed, and the crown of the upper right central incisor 11 reconstructed (tooth 11 had erupted with a malformed crown). The authors report that the odontoma and abnormalities in teeth 11 and 21 were caused by a childhood trauma. In some African countries, in accordance with local beliefs, children aged from 3 months to 3 years have the buds of their deciduous teeth removed by their healer for protection against viruses and vomiting. The authors mention 2 more cases of children who had their deciduous tooth buds removed in a ritual in their childhood, and then were diagnosed with an odontoma in their adolescence.5 In one of our patients (17 years old, with nephritic syndrome), the odontoma was visible in the oral cavity in the region of lower left canine 33 and lower left first premolar 34. During the first appointment, the visible nodule was diagnosed as an erupting supernumerary tooth, and it was not until an X-ray was performed that the correct diagnosis of OCp was reached, which, due to its occurrence in the oral cavity, was described as an erupted odontoma (Figure 6). In this case, similarly to our other patients, the patient’s parents could not remember past traumas or inflammations in the region of the odontoma.
Custódio et al. report that odontomas can occur not only in the bone of the jaws, but also peripherally.20 In their article, they describe a case of an 11-year-old girl who had on her palatal mucosa a 1.5-centimeter non-painful nodular lesion with a smooth surface, covered with an unaffected mucous membrane, which had been growing slowly for more than 2 years. Clinically, the picture was consistent with a peripheral ossifying fibroma or a peripheral giant-cell granuloma. Radiological and intra-operative examinations revealed no erosion of (damage to) the bone tissue. In was not until histopathological examination that a complex odontoma was revealed. In their study, the authors refer to 17 publications from the years 1989–2014 discussing peripheral odontomas (gingival odontomas/soft tissue odontomas), 15 of which were found in children.20
Clinically, in 18 (90%) of our patients, the lesions occurred in bones, and in 2 patients (10%), there were exophytic lesions in the oral cavity (in a 3-year-old patient on the lingual side, near teeth 83 and 84, and in a 14-year-old patient after cleft lip and cleft palate on the palatal side near tooth 13). An erupted odontoma was discovered accidentally in a 3-year-old patient during a dental appointment; his parents did not know how long it had been present in the oral cavity. The lesion was not painful, covered with an unchanged mucous membrane. Due to the patient’s lack of cooperation, X-ray images were inaccurate and did not indicate any pathologies. In general anesthesia, CT was performed, revealing a small radiopacity located lingually at the level of the neck of tooth no. 83, characteristic of OCp. A 14-year-old patient was admitted to the Dental Surgery Clinic for the removal of a palatal lesion. On clinical examination, tooth 12 was missing, tooth 13 was displaced, the alveolar process of the maxilla was slightly distended, and an odontoma was erupting from the palatal side – it was removed in local anesthesia.
Clinical signs of odontomas described in the literature include retained deciduous teeth, impacted permanent teeth, the distension of the alveolar process of the maxilla or the alveolar part of the mandible, gaps, mild pain (in only one case), a changed shape of teeth (one patient after a childhood trauma), a nodular non-painful lesion covered with an unaffected mucous membrane (diagnosed as a gingival complex odontoma), discovered accidentally in an X-ray image.2, 3, 4, 5, 6, 7, 8, 9, 10, 19, 20 In most of our cases, the symptoms were similar: tooth eruption disorders; the protrusion of the alveolar process of the maxilla or the alveolar part of the mandible; retained deciduous teeth; impacted permanent teeth without abnormalities; gaps; no pain. Only one boy was referred to a dentist due to pain and the swelling of the cheek, as his tumor was large and caused a significant distension of the alveolar process of the maxilla. Normal tooth eruption was observed at follow-up visits, with no indications for orthodontic treatment.
Radiographically, OC is a highly dense radiopacity of irregular shape, surrounded by a band of radiolucency with a sclerotic rim,6, 19 and OCp is a dense radiopacity arranged as numerous small deformed denticles (odontoids) surrounded by a band of radiolucency and a sclerotic rim.6 Similar radiological pictures were obtained for our patients. Histopathological examination should be conducted to confirm the clinical and radiological diagnosis. On microscopic examination, OCp is described as fragments of the dental pulp, dentin, enamel matrix, epithelium, and connective tissue, or as fragments of a tooth with preserved histological structure, with fragments of fibrovascular tissue. On the other hand, OC is described in histopathological findings as fragments of dentin and connective bone tissue. The histopathological picture of OC is very similar to that of an ameloblastic fibro-odontoma (AFO).20, 21 And this was the microscopic picture obtained for the lesions removed in our patients.
Recently, there has been improvement in X-ray diagnostic imaging methods, especially with regard to CBCT, which certainly facilitates arriving at diagnosis as early as at the stage of radiological examination. Jayam et al. describe a case of an 11-year-old girl with a radiological picture (panoramic radiography, a tooth X-ray and a maxillary occlusal radiograph) description of impacted tooth 11 with an additional cusp and an extensive dentigerous cyst.2 In the course of marsupialization, the dentigerous cyst was found to have no contact with tooth 11, while it contacted the adjacent additional cusp. On histopathological examination, OCp was diagnosed with a cyst. According to some authors, X-ray images – panoramic radiographs and targeted dental X-rays – may not accurately reveal the pattern of the lesion, which is why cross-sectional CBCT is recommended in the case of doubts or for more accurately determining the location.2 In the case of 2 of our patients, it was not until a CBCT was performed that the adequate diagnosis was reached, and it was later confirmed during the procedure and histopathological examination. The first patient was a 9-year-old girl referred to an orthodontist in our clinic due to impacted tooth 21 for the exposure of the tooth and the application of a bracket to the crown of tooth 21. The patient had with her a current panoramic radiograph with visible impacted tooth 21, showing a small non-distinctive radiopacity in the tooth crown, which could be consistent with an additional cusp. An X-ray of tooth 21 was performed at our clinic, revealing a non-distinctive area of radiopacity next to the crown of tooth 21 (Figure 7). The patient was referred for cross-sectional CBCT. After verification, OCp was diagnosed and removed with its capsule, and an orthodontic bracket was attached to tooth 21 in local anesthesia (Figure 8). Histopathological examination confirmed the preliminary diagnosis of OCp. The other patient was a 5-year-old girl who was admitted to our clinic with a missing deciduous tooth 65. The patient had a current panoramic radiograph with her, revealing an impacted tooth (most probably tooth 65) with a non-distinctive area of radiopacity (Figure 9). Cross-sectional CBCT was recommended. In the X-ray image, the preliminary diagnosis suggested OCp with the impacted deciduous tooth 65 above it and the tooth bud of permanent tooth 25 on the palatal side (Figure 10). The procedure involved the resection of the impacted deciduous tooth 65 and the enucleation of the odontoma with its capsule; the tooth bud of tooth 25 was left. Due to the child’s age and her poor cooperation, the procedure was carried out in general anesthesia. Histopathological findings revealed OCp.
Preoteasa and Preoteasa mention the possibility of asymmetric resorption of the roots of deciduous teeth, caused not by a permanent tooth, but by a tumor, which may lead to tooth eruption disorders, i.e., to the occurrence of an impacted deciduous tooth and an impacted permanent tooth.9 The authors describe a case of a 9-year-old patient who was admitted with impacted upper left central incisor 21, ectopically located upper lateral incisor, and retained deciduous incisors – left central 61 and left lateral 62. The X-ray image revealed OCp located between teeth 61 and 21, which caused asymmetric resorption of the root of deciduous tooth 61, which could have caused its delayed exfoliation.9 Other authors, Amailuk and Grubor, report the possibility of changes in the shape of the roots of permanent teeth adjacent to a tumor.5 In the group of our patients, there were 2 cases (10%) with a retained deciduous tooth above which an odontoma was found with a permanent tooth over it, but no changes were observed in the shape of the root of permanent teeth.
A 14-year-old patient, after the treatment of complete cleft lip and palate, came to us for the treatment of an odontoma. Paradowska-Stolarz and Kawala compared the incidence of dental anomalies in 154 patients with complete cleft lip and palate and in 151 healthy patients.22 According to the authors, dental anomalies were much more common in patients with cleft and on the cleft side.22 In our case, the odontoma was on the right side and the cleft was on the left side.
The treatment of choice for odontomas is a surgery involving the complete enucleation of the tumor with its capsule. According to de Oliveira et al.4 and Qazi et al.,23 if an odontoma causes the impaction of the tooth bud of a permanent tooth, the tumor should be removed as soon as possible, before the root of the permanent tooth is fully developed (e.g., before it reaches half of its length) to prevent its permanent impaction. According to Uma, in turn, if after the removal of an odontoma, the impacted tooth does not erupt within 3 months of the procedure, the patient should be referred to an orthodontist.3 In conclusion, odontomas should be removed as soon as possible to prevent the occurrence of complications in the form of dental abnormalities. In our clinic, the tumors were removed as soon as possible (within a month from the first appointment). In one case, the procedure was postponed in a 4-year-old boy (with antiphospholipid syndrome) who was receiving chemotherapy. On clinical examination, the protrusion of the alveolar process of the maxilla and a small gap between deciduous teeth 62 and 63 were observed, and there were no impacted teeth. The procedure was performed 4 months after the first appointment, during which OCp was diagnosed.
Many authors recommend the use of platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) after surgical procedures, presenting their benefits.24, 25, 26 Healing after procedures in children very often proceeds without complications. In our cases, we did not observe dry sockets or bone inflammation. We did not perform odontoma removal procedures in patients taking bisphosphonates. In our research, we did not use PRP and PRF, but based on many positive studies and opinions, we are considering the use of PRP and PRF after odontoma removal procedures.
The literature does not report recurrences after the complete enucleation of the tumor with its capsule.8, 9 So far, we have not observed recurrences in any of our patients, either.
Conclusions
Odontomas are benign tumors that do not undergo neoplastic transformation. Such clinical signs as dental abnormalities, missing teeth, a protrusion on the alveolar process of the maxilla or the alveolar part of the mandible should prompt a dentist to perform diagnostic imaging. It is very often that, due to the absence of clinical signs, odontomas are discovered by accident during an X-ray performed before orthodontic treatment. The compound odontoma is the most common type of odontoma. Its radiological picture is characteristic – highly dense tooth-like radiopacities (odontoids) surrounded by a band of radiolucency with a sclerotic rim. The treatment of choice is a surgical procedure involving the complete enucleation of the tumor with its capsule, which results in full recovery.
Ethics approval and consent to participate
This retrospective study was approved by the institutional review board at The Children’s Memorial Health Institute, Warsaw, Poland (No. of approval: 28/KBE/2021).
Data availability
The datasets supporting the findings of the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.