Abstract
Background. The examination of pro-health behaviors is important in the assessment of factors that influence the health of the population. Despite a constant increase in pro-health awareness observed within Polish society, the epidemiological picture of adult oral health remains unsatisfactory.
Objectives. The aim of the study was to assess the level of knowledge of the study population regarding the prevention of caries, the role of fluoride compounds, and hygiene habits.
Material and methods. A quantitative cross-sectional methodology was employed in the study. A specially designed anonymous survey was used to ensure the confidentiality of participants and to encourage truthful responses. The data was collected over a 5-month period using computer-assisted web interviewing (CAWI) with a Google Forms survey. The link to the survey was shared in public groups and on social media platforms, ensuring the collection of a diverse sample. Submitted surveys were cataloged and de-identified prior to analysis.
Results. The final sample size of the study was 643 participants. In the present study, only 95 respondents (14.77%) demonstrated sufficient knowledge about oral hygiene and declared behaviors that align with recommended practices. Factors such as place of residence, education and income did not have a statistically significant effect on the level of health awareness in relation to the preferred health attitude of the “ideal patient”. The study revealed a lack of knowledge regarding the role of fluoride in caries prevention, with some individuals considering it harmful and refraining from using fluoride toothpaste. Approximately 20% of the surveyed population lacked awareness of the presence of fluoride in their toothpaste. These observations were comparable across both rural and urban areas.
Conclusions. The present study indicates insufficient knowledge regarding oral health among the study population. It is necessary to introduce more comprehensive oral health education programs targeted at the adult population of Poland.
Keywords: surveys and questionnaires, health education, oral hygiene, health behavior, cross-sectional studies
Introduction
Maintaining proper oral hygiene is essential for ensuring optimal oral health, which in turn affects the overall health of the individual. Additionally, oral health has an influence on self-esteem, physical and mental well-being, as well as interpersonal contacts, thereby affecting the quality of life.1, 2 The World Health Organization (WHO) defines oral health as “the state of the mouth, teeth and orofacial structures that enables individuals to perform essential functions such as eating, breathing and speaking, and encompasses psychosocial dimensions such as self-confidence, well-being and the ability to socialize and work without pain, discomfort or embarrassment. Oral health varies over the life course from early life to old age, is integral to general health and supports individuals in participating in society and achieving their potential”.3
The etiology of the majority of oral diseases, including caries and periodontal diseases, is determined by common etiological factors that are shared with many chronic diseases.4, 5 These factors include lifestyle and associated poor nutrition, smoking, alcohol, drugs, and poor hygiene practices.6 The primary means of enhancing oral health are interdisciplinary health promotion and prevention strategies, targeting the needs of the individual and the population.7, 8 An individual’s oral health behavior is influenced by a multitude of factors, including socioeconomic status, sex, level of education and knowledge, and attitudes toward oral health.9, 10 However, consistent adherence to recommended behaviors, such as brushing at least twice a day, cleaning interdental surfaces and using fluoride, has been proven to effectively reduce the frequency and severity of dental caries.11 The international evidence base demonstrates that the use of fluoride reduces the susceptibility of teeth to caries and demineralizes early enamel damage, contributing to a significant and rapid reduction in the incidence of caries.12, 13, 14, 15, 16, 17, 18, 19 Despite the widespread availability of modern toothbrushes, toothpastes, rinses, and a range of other oral hygiene products used in home prophylaxis, the inadequate level of health education remains the limiting factor.20, 21
A notable increase in pro-health awareness has been observed among the Polish population over time. However, epidemiological data indicates that the oral health of adult Poles remains unsatisfactory, as evidenced by the data presented. A notable decline in the prevalence of dental caries and a reduction in the number of tooth extractions due to caries among individuals aged 34–44 years has been observed in the 2019 study compared to the 2010 study.22 However, the value of the decay-missing-filled (DMF) index remained relatively high.22
Studies have indicated that the pro-health behaviors exhibited by the population deviate from the established standard.22 A significant proportion of respondents stated that their most recent dental visit was prompted by toothache and the necessity for immediate treatment, rather than routine check-ups and preventive care.22 This phenomenon is associated with a lack of comprehension regarding the significance of prevention, which consequently results in inferior health outcomes. The allocation of resources toward oral health education has the potential to reduce the financial burden associated with the control and management of dental caries and its associated complications. Numerous studies have attested to the efficacy of fluoride; however, the WHO announcement regarding its potential neurotoxic effect has led to an increasing number of patients discontinuing its use.23, 24, 25 Despite the clear stance of experts on the safety of fluoride compounds in oral care products, some individuals refrain from using them. Furthermore, there has been a notable increase in social media discourse addressing public concerns about healthy living. Consequently, natural and organic oral care products have become more popular.26 This phenomenon may contribute to the dissemination of misinformation about fluoride on online platforms.27 Further research is necessary to evaluate the extent and implications of this trend.
The objective of this study was to assess the level of knowledge about the etiology of dental caries, health-promoting behaviors, and the role of fluoride compounds in preventing dental caries among the adult population residing in the Masovian Voivodeship in Poland. Additionally, the study aimed to identify factors that influence appropriate health-promoting attitudes among the studied population, thereby providing insights into the effectiveness of current oral health education and practices.
Material and methods
The present study was conducted from December 30, 2022, to April 27, 2023. A quantitative cross-sectional methodology was employed using a questionnaire. Eligibility for participation in the study was determined based on specific inclusion and exclusion criteria. Individuals who met the following criteria were included in the study: age >18 years; possessing at least 5 permanent teeth; having no professional affiliation with the field of dentistry; and residing in the Masovian Voivodeship. Conversely, individuals under the age of 18, with fewer than 5 permanent teeth, those professionally involved in dentistry (e.g., dentists, hygienists, dental assistants, or dental students), and those residing outside the Masovian Voivodeship were excluded from the study. All individuals who met the inclusion criteria were considered eligible to participate in the study.
The survey was designed to be anonymous and consisted of 21 questions (supplementary material – available on request from the corresponding author). The first 5 questions were designed to collect sociomedical data using a single-choice format. The subsequent 16 questions included both single- and multiple-choice options and focused on health awareness and attitudes, as well as the sources of information regarding health and hygiene habits of the respondents.
In addition, for the purpose of the survey, we have distinguished the attitude of the “ideal patient” based on current medical knowledge. To qualify as the “ideal patient”, respondents were required to correctly answer 6 out of the 16 questions regarding health awareness, including 4 key questions. The key questions posed to the respondents were as follows:
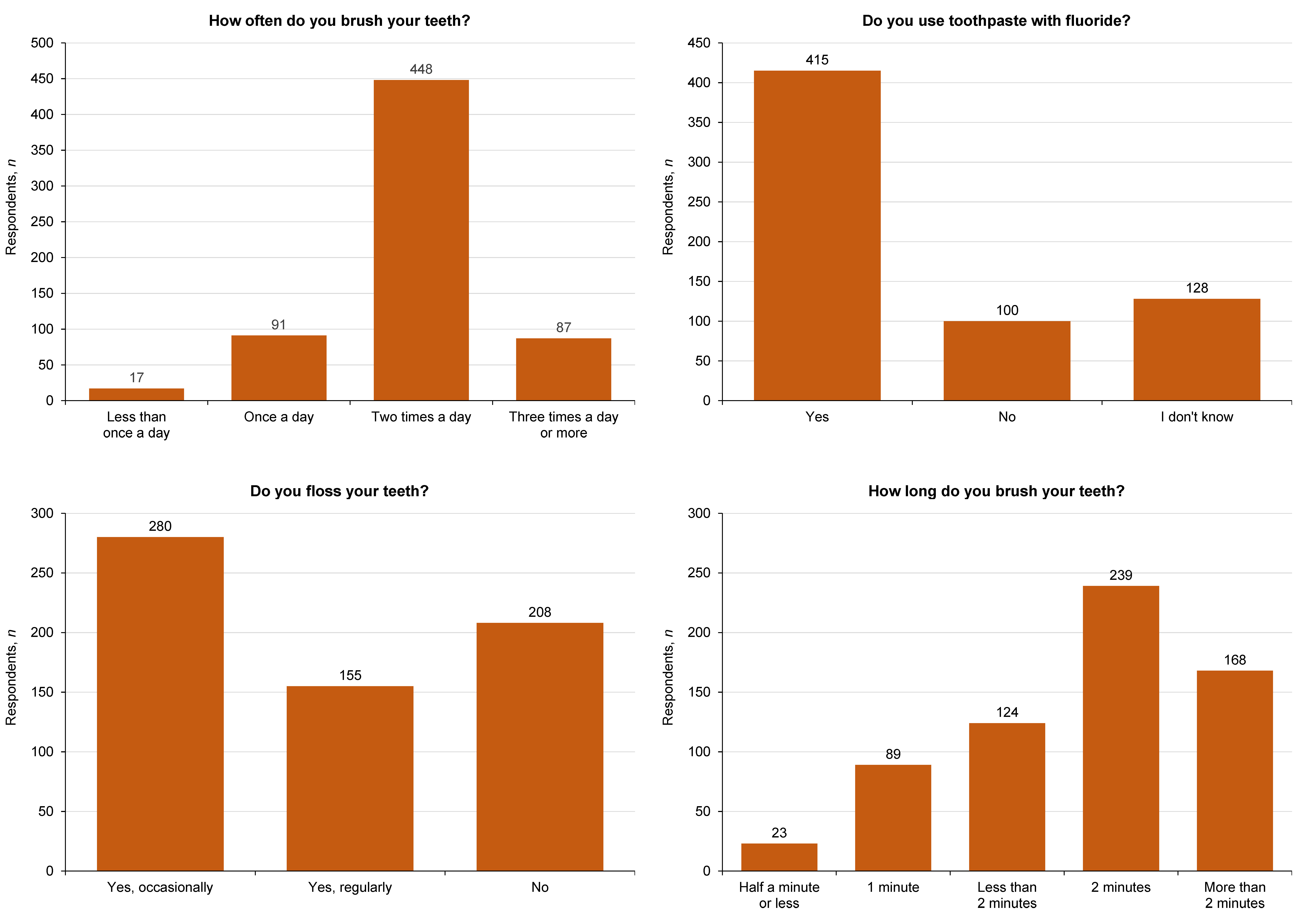
1. How often do you brush your teeth? The correct answers were: “twice a day” or “three times a day or more”;
2. Do you use toothpaste with fluoride? The correct answer was: “yes”;
3. Do you floss your teeth? The correct answer was: “yes, regularly”;
4. How long do you brush your teeth? The correct answers were: “2 minutes” or “more than 2 minutes”.
The data was collected using the computer-assisted web interviewing (CAWI) method with a Google Forms (Google LCC, Moutain View, USA) survey. The survey was meticulously designed to ensure participant anonymity, guarantee data confidentiality, and encourage candid responses. The survey link was disseminated through local Facebook groups specifically targeted to the Mazovian Voivodeship. Additionally, the participants were encouraged to share the survey link with their acquaintances residing in the Mazovian Voivodeship. The invitation to participate in the survey explicitly stated that only residents of the Mazovian Voivodeship were eligible to take part in the study. To maintain the integrity of the data, the Google Forms platform was configured to block multiple submissions from the same user, ensuring that each participant completes the survey only once.
Ethics approval for the study was obtained from the Bioethics Committee of the Medical University of Warsaw (No. AKBE/143/2022). The participants were informed about the purpose of the study and the potential benefits through the survey platform. Completion and submission of the survey were considered consent for participation in the study.
Statistical analysis
Descriptive statistics were employed to summarize the basic characteristics of the study group, thereby providing the number and percentage of responses to each question in the survey. A subsequent comparison was made between the residents from rural and urban areas regarding their behaviors and knowledge levels using the χ2 test. This analysis provided a foundational understanding of the general characteristics of the survey data.
Inferential analysis was conducted using a logistic regression model to explore the relationships between various independent variables (e.g., age, sex and socioeconomic status) and dependent variables related to health-promoting behaviors and knowledge levels. The model parameters were estimated using the maximum likelihood estimation (MLE) method. This analysis was instrumental in identifying the key factors that influence the adoption of health-promoting behaviors among the adult population of Warsaw and its surrounding areas. Odds ratios (ORs) were calculated for each predictor within the logistic regression model, along with their 95% confidence intervals (CIs), thus enabling the quantification of the strength and precision of the observed associations.
A significance level of 0.05 was adopted for all statistical analyses in this study. Statistical significance was assigned to results with a p-value of 0.05 or lower, indicating that the observed effects have less than a 5% probability of being attributable to random variation. All statistical analyses were performed using STATISTICA v. 13.3 (TIBCO Software, Inc., Palo Alto, USA) under a license from the Medical University of Warsaw.
Results
A total of 680 questionnaires were initially collected, with 37 subsequently excluded for failing to meet the established criteria, resulting in a final sample size of 643 participants. The age distribution among the respondents exhibited variability, with the largest group being those aged 18–25, constituting 29.86% of the sample. A significant majority of the participants were female, representing 73.56% of the study group. Regarding educational attainment, 60.19% of the respondents held higher education degrees, while 36.24% had completed secondary education and 3.57% had finished primary education. The majority of the participants resided in towns or cities (58.48%), with the remainder living in rural areas (41.52%). The respondents exhibited a wide range of income levels, with 54.74% reporting average income, 28.77% earning above average, and 16.49% below average. A comprehensive overview of the sociodemographic characteristics of the study group is presented in Table 1.
The vast majority of respondents followed the principles of oral prophylaxis. It is important to note that nearly 80% of respondents indicated that their source of information was a dentist. Statistically significant differences were identified in relation to the place of residence of the respondents. A higher percentage of people living in cities used information from their family than those living in rural areas. The study population included individuals who had never received professional oral hygiene instruction.
The research results indicate that the role of fluoride in caries prevention is unsatisfactory. Some individuals consider it harmful and therefore do not use fluoride toothpaste. In the surveyed population, nearly 20% of respondents lacked awareness regarding the presence of fluoride in their toothpaste. In addition, 40% of respondents did not know which toothpaste they were currently using, relying on the toothpaste available at home. More than a third of respondents acknowledged that their purchase decisions were influenced by factors such as price and advertising. These observations were consistent across both rural and urban areas.
The statistical analysis demonstrated that place of residence is a significant factor in attitudes toward oral health priorities. Individuals residing in urban areas were more likely to report that having white teeth and healthy gums is important to them, compared to those living in rural areas. Similar trends were identified in the frequency of tooth brushing, flossing and mouth washing after brushing. Table 2 presents the detailed responses to the questions included in the questionnaire.
Figure 1 provides a comprehensive overview of oral hygiene practices, focusing on daily routines that contribute to oral health. The analysis reveals varied adherence to recommended practices, which are critical for maintaining a healthy oral cavity. The majority of respondents (83.2%) brush their teeth twice a day or more often, adhering to dental recommendations, while 14.15% of the participants brush their teeth once a day. A mere 2.6% of the respondents brush less than once a day, indicating a strong general compliance with the recommended twice-daily brushing regimen. Furthermore, the analysis indicates a high prevalence of fluoride toothpaste usage, with 64.5% of the participants reporting its incorporation in their oral hygiene routines. Concerning the practice of flossing, the data reveals that less than half of the respondents (43.5%) floss occasionally, while 24.1% engage in regular flossing. Notably, 32.3% of the respondents do not floss at all. With regard to the duration of tooth brushing, a fundamental component of effective oral hygiene, 37.2% of the participants brush for the recommended 2 min. However, 26.1% brush their teeth for more than 2 min. In contrast, 19.3% of the individuals brush for less than 2 min, 13.8% for only 1 min, and a small minority (3.6%) brush for half a minute or less.
In the present study, only 95 respondents (14.8%) demonstrated sufficient knowledge regarding oral hygiene and declared behaviors that align with recommended practices. The analysis revealed that sex and age were significant predictors of being an “ideal patient” who adheres to recommended oral hygiene practices. Specifically, the likelihood of men being classified as “ideal patients” was significantly lower in comparison to women, with OR of 0.47 (95% CI: 0.25–0.85, p = 0.013), indicating that men were about 53% less likely to demonstrate ideal oral hygiene behaviors than women. Furthermore, respondents aged 46–65 showed a significantly higher probability of adhering to recommended oral hygiene practices, with OR of 2.90 (95% CI: 1.49–5.64, p = 0.002), suggesting that they were almost 3 times more likely to adhere to recommended practices compared to the youngest age group (18–25 years). Other age groups did not show significant differences when compared to the reference group. The analysis revealed that other sociodemographic variables such as education, place of residence and income level did not demonstrate a significant correlation with the likelihood of being an “ideal patient” (Table 3).
Discussion
The survey provided valuable information regarding the etiology of the high incidence of caries and periodontal diseases in the Polish population. The obtained results indicated that health awareness and related attitudes remain at a low level. The majority of respondents follow the basic rules of oral prevention, which is limited to brushing their teeth twice a day without regular flossing or using additional measures, e.g., fluoride rinses.
Socioeconomic status is an important determinant of health status, with its impact being manifested through dietary habits, hygiene practices and health awareness. The systemic changes that Poland has undergone have had a significant impact on the health status of the society. The general availability of a wide range of oral hygiene products, the development of the private sector, increased health awareness, but also the collapse of institutional dental care and relatively low expenditure on the medical sector create a situation that is difficult to assess unequivocally. Recent studies have indicated that individuals from families with a higher socioeconomic status exhibit a significantly better health status with respect to dental caries and periodontal diseases.28, 29, 30 Similar trends have been observed in Polish society.22 Despite the improvement in clinical parameters, a certain percentage of adult patients continue to experience the adverse effects of caries, gum and periodontal diseases in their daily lives.31 In the present study, place of residence, reported income or education did not have a significant impact on the pro-health attitudes of respondents in the ideal patient model. However, the statistical analysis of the survey’s questions sheds light on several additional aspects. The difference in attitudes between urban and rural residents was particularly interesting in relation to sources of dental information. Parents and family were statistically more frequently mentioned by urban residents. This finding underscores the important role of the dentist as a reliable source of knowledge and information for patients. Previous epidemiological studies have highlighted the lack of prevention and hygiene education in dental practices.32 Routine dental visits present an opportunity for healthcare professionals to not only assess the risk of caries but also to motivate patients and update their knowledge. A study by Verploegen and Schuller revealed that patients receive insufficient information from the dental team during office visits.33 Additionally, an increasing number of adults acquire health-related knowledge from the Internet.33 While the Internet and social media may enhance health awareness, they do not necessarily motivate or increase self-efficacy in health promotion. This highlights the significance of providing evidence-based information in the dental office to modify patient behavior. The results of the study confirmed that dental professionals remain the most reliable source of information concerning prevention and oral health.34
The study respondents residing in urban areas were more likely to prioritize the importance of white teeth and healthy gums than respondents from rural areas. Similar trends were identified in relation to the frequency of brushing, flossing and mouth washing after brushing.
A total of 473 women and 170 men participated in the study, indicating that women are the more active and health-oriented group. At the same time, women exhibited a higher level of knowledge and pro-health behavior. This phenomenon has been observed consistently over many years, not only in Polish society.35, 36, 37 A notable finding was obtained in relation to the age of the respondents. Individuals over the age of 40 exhibited more favorable attitudes toward oral health maintenance. In contrast, an inverse relationship was described in the study by Jensen et al.21 The authors observed that individuals over 35 years of age exhibited less favorable attitudes toward health promotion. These behaviors were particularly pronounced in the senior patient group.21
As individuals age, the importance of health increases due to the fact that the quality of life tends to deteriorate and there is an increase in limitations in independent functioning. While this relationship is evident in relation to general health, it remains insufficiently understood in relation to oral health. A growing number of patients prioritize the aesthetic appearance of their teeth, often neglecting their functional role.38 The majority of respondents acknowledged the significance of healthy teeth, yet their responses indicated a lack of awareness regarding the progression of caries and the condition of the periodontium, suggesting a potential knowledge gap concerning these health concerns. Notably, individuals who considered the condition of their gums important and utilized chlorhexidine mouthwash, presumably due to underlying periodontal problems, presented more favorable pro-health attitudes. The hygienization phase of the treatment of patients with periodontal disease necessitates their adherence to recommendations. The prolonged nature of the treatment, which includes instruction, motivation and repeated professional dental cleaning procedures, contributes to patients’ greater awareness and attention to maintaining good oral hygiene. The formation of proper health-promoting attitudes is implemented, but in practice, for a considerable number of individuals, this process ends during early childhood and school years. The situation is particularly problematic for adults, especially the senior population, for whom dental prophylaxis is often inadequate.
According to experts in the field, the theories regarding the adverse effects of fluoride are exaggerated and the concentration of this element in oral care products is sufficiently low to be considered safe.39 Furthermore, there are no studies that associate fluoride in toothpaste with negative health effects. At the same time, there has been an increase in the number of patients who are aware of the contemporary world’s demands and the transformations witnessed in recent years. Green dentistry, a concept linked to sustainable development, has emerged as a response to the pressing need for improvement in social, environmental and economic standards.26 However, a paucity of studies has been conducted on the subject of organic toothpastes. Notably, none of the studies included comments on this topic. This may indicate that the promotion of these products is still insufficient. Price and advertising have been identified as the most common determinants of toothpaste purchase.
An effective oral hygiene routine includes brushing teeth twice a day, cleaning the interdental spaces, rinsing the mouth, using sugar-free gum, and maintaining an appropriate diet that limits the intake of products containing carbohydrates, including hidden sources. A study conducted in the late 1990s sought to assess the oral health of the Polish population and revealed a lack of awareness regarding health among patients.34 At the time, the utilization of dental floss and the proper cleaning of interdental surfaces were the indicators of awareness. The authors found that while most respondents were aware of flossing, approx. 1 in 7 men and 1 in 4 young women actually practiced it.34 Residential environment did not significantly differentiate either the awareness of the role of flossing or its use. In our research, improvements were noted in the issue at hand. After approx. 25 years, regular flossing has become a regular part of daily oral hygiene for a quarter of the respondents.
Limitations
The study’s limitations include the selection of the population, which was focused on dwellings in Warsaw and its environs (Masovian Voivodeship). Therefore, the results obtained may be more favorable compared to the rest of the country, especially for those with lower incomes living in less developed areas.
To enhance the data collection process, it was decided to conduct the survey electronically. As a result, the study population consisted only of individuals with Internet access. Moreover, the nature of the survey design may have encouraged responses that were intended to improve the subjects’ image, which could have resulted in the presentation of falsified data.
Conclusions
The outcomes of this research indicate that the population under study lack sufficient knowledge of oral health. The necessity for the implementation of effective domestic oral hygiene care measures is underscored. This study emphasizes the need to introduce comprehensive oral health education programs tailored to the adult Polish population, given the absence of dedicated programs for this demographic.
Ethics approval and consent to participate
Ethics approval for the study was obtained from the Bioethics Committee of the Medical University of Warsaw (No. AKBE/143/2022). Completion and submission of the survey were considered consent for participation in the study.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.