Abstract
Background. Temporomandibular disorders (TMDs) are challenging to manage due to their multifactorial nature. As with other joints, the function of temporomandibular joint (TMJ) is influenced by proprioception, making it an essential factor in TMD management. However, previous studies on the joint position error (JPE) in TMD patients lacked a proper diagnosis and reliability assessment.
Objectives. The aim of the present study was to develop a reliable JPE test in healthy adults as a foundation for future evaluation in TMD patients.
Material and methods. Two examiners conducted the JPE assessment, utilizing a methodology encompassing between-days intra-rater and within-day inter-rater reliability assessments. A total of 22 healthy participants (7 men and 15 women) with a mean unassisted mouth opening of 46 ±5 mm were recruited. The evaluation targeted specific distances (10 mm, 20 mm and 30 mm) within the participants’ mouth opening range, with proprioceptive accuracy evaluated through the measurement of the absolute error (AE) and the constant error (CE).
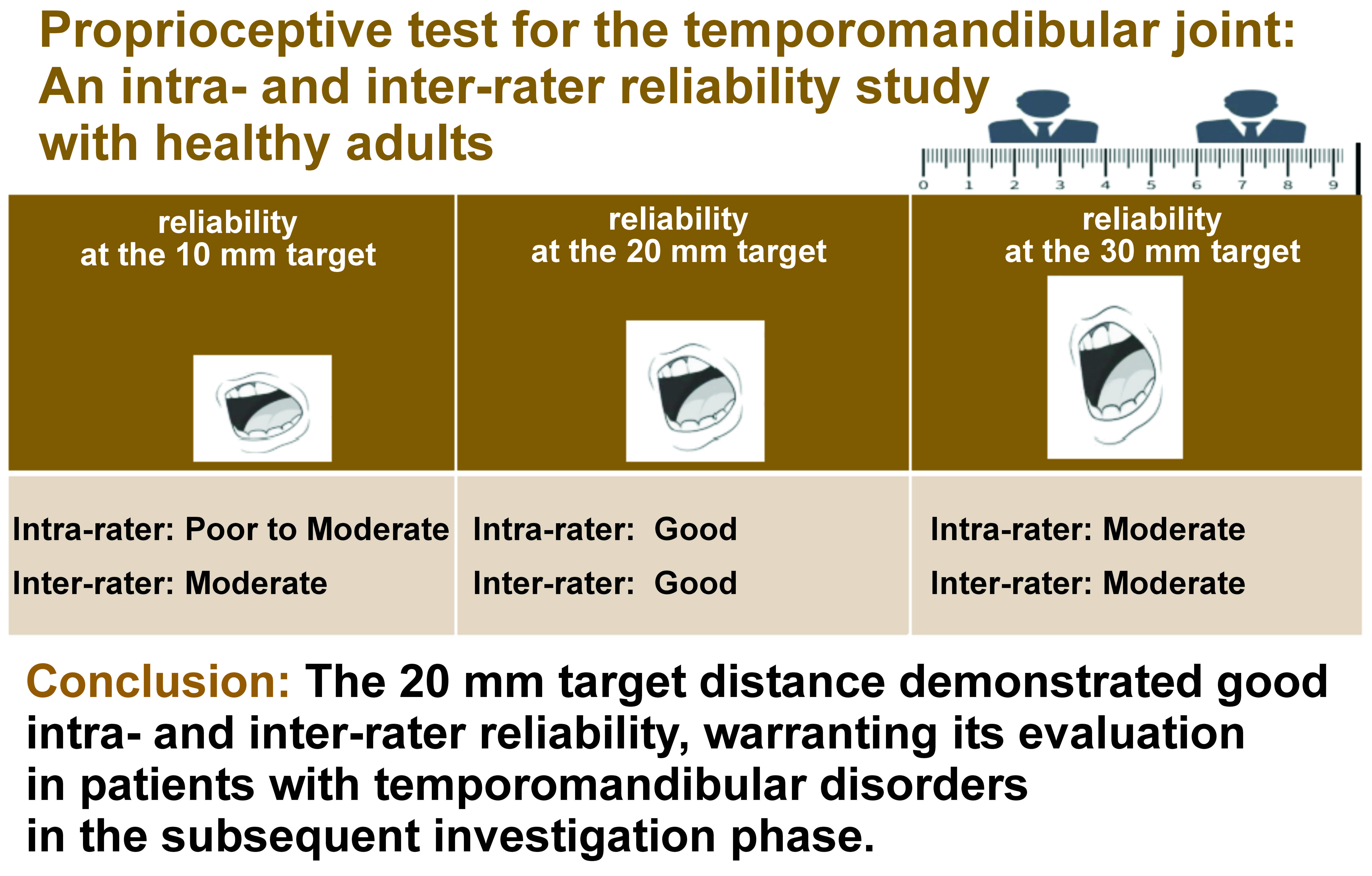
Results. The CE was consistently lower than AE across all the targeted distances, although with higher standard deviations. Intra-rater reliability varied across the distances, with poor reliability observed for AE at 10 mm, moderate reliability for CE at 10 mm, good reliability for both AE and CE at 20 mm, and moderate reliability for both AE and CE at 30 mm. Inter-rater reliability was moderate at 10 mm and good at 20 mm for both AE and CE, with equally moderate reliability levels at 30 mm.
Conclusions. The 20 mm target distance demonstrated good intra- and inter-rater reliability, warranting its evaluation in patients with TMDs in the subsequent investigation phase.
Keywords: temporomandibular joint (TMJ), reliability, proprioception, temporomandibular disorders (TMDs), joint position error (JPE)
Introduction
Temporomandibular disorders (TMDs) are a group of conditions that affect the temporomandibular joint (TMJ), masticatory muscles and other related structures.1 These disorders can cause pain, and facial and jaw dysfunction.2 Temporomandibular disorders are challenging to diagnose and manage due to their multi-etiological nature, including biomechanical, genetic, psychosocial, sleep, and neurobiological factors.2, 3, 4 According to a large multisite prospective cohort study conducted in the USA, called the OPPERA (Orofacial Pain: Prospective Evaluation and Risk Assessment) study, it is estimated that each year, 4% of TMD-free adults aged 18–44 years develop a clinically confirmed first-onset painful TMD.5 The annual incidence of TMDs increases with age, with 2.5% for adults aged 18–25 years, 3.7% for adults aged 25–34 years, and 4.5% for adults aged 35–44 years.5 Despite recent advances in research and clinical management, TMDs still present a challenge, requiring ongoing investigation and collaboration among healthcare professionals to optimize and personalize patient care and outcomes.6, 7, 8
The sensorimotor system comprises 3 primary inputs for motor control – visual, vestibular and somatosensory.9 Proprioception is a critical aspect of the somatosensory component, providing the ability to sense the body parts’ position, movement and orientation in space.10 In the context of joint function, proprioception is vital in providing feedback to the central nervous system (CNS), regarding the relative positions of the articulating surfaces, and the muscle length and tension.10 This feedback helps perform precise movements and coordinate them.10 The joint position error (JPE) measures how accurately an individual perceives and reproduces a specific joint position.11 Several factors, such as aging, injury, hypermobility joint syndrome, and neurological conditions, can impact the proprioceptive function and contribute to alterations in JPE.10, 12 The JPE serves as a critical, valid and reliable outcome measure for several joints in the human body during the rehabilitation process.13, 14, 15
When we move our jaw around TMJ without the visual feedback or the vestibular input, we rely entirely on somatosensory information. This means that the proprioceptive component is crucial for the normal function of the masticatory system. Some studies suggest that patients with TMDs may have a deficit in proprioception.16 Still, previous studies that evaluated JPE in TMD patients failed to subdivide patients properly and demonstrated a high risk of bias.16 A recent study assessed JPE in a specific subgroup of TMD patients (those with intra-articular disorders),17 and while it reported some clinically meaningful deficit in the TMD group, it did not provide any intra- or inter-rater reliability values, which weakens its external validity.
Therefore, the present study aimed to develop a specific and reliable test for JPE in healthy adults, which may be conducted on TMD patients in the future.
Methods
This observational reliability study involved a between-days (two-day gap) intra-rater and within-day inter-rater reliability design. The study followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) reporting standards, as well as the three-phase reliability protocol recommended by the International Academy of Manual/Musculoskeletal Medicine (IAMMM).18 Data was collected from April to June 2023. The study was approved by the ethics committee at Recanati School for Community Health Professions of Ben Gurion University of the Negev, Be’er Sheva, Israel, and all the participants provided written informed consent.
Participants
All the participants were recruited from the student population at the Department of Physical Therapy of Ben-Gurion University of the Negev. To ensure eligibility for the study, volunteers were initially asked to fill out and email a health screening questionnaire.
The study included individuals aged 18–40 years, currently enrolled as physical therapy students at the university. They were generally healthy and could open their mouths without reporting pain (pain-free opening) at a minimum of 45 mm.
The exclusion criteria were as follows: individuals younger than 18 years old; those with a diagnosed systemic or neurological condition; individuals with a history of neck surgery or jaw surgery directly involving the jaw joint (e.g., arthroplasty); individuals with a history of cancer affecting the neck, jaw, face, or mouth; individuals who had experienced trauma affecting the neck or head (e.g., concussion) with ongoing neck or facial pain over the past 6 months; individuals with a history of neck or jaw fractures in the past 3 months; those with major dental procedures or orthodontic treatment in the past 4 weeks; and any individuals with missing or artificial molars, excluding wisdom teeth.
Examiners
Two qualified physical therapists (N.R. and D.B.) conducted the study’s examinations. A senior physical therapist with 20 years of clinical experience in cervical-cranio-mandibular rehabilitation, holding DPT and Ph.D. in Physical Therapy degrees (T.G.), individually trained them for the examination protocol.
Testing procedure
The TMJ position sense was evaluated using the active assisted positioning–active replication method. The measurement was taken using a ruler, and regarded the distance between the top and bottom incisors,19, 20 as illustrated in Figure 1. To determine the reliability rates, the joint position sense was tested at 3 target positions – 10 mm, 20 mm and 30 mm of mouth opening – representing the inner, middle and outer range of motion, respectively. The participant performed 3 repetitions at each target (10/20/30 mm), and the absolute error (AE) for the 3 trials at each target was the outcome measure (Figure 1).
During the examination, the examiner directed the participant to sit on a chair with their back supported and both feet on the ground. The head was intentionally unsupported to stimulate a real functional scenario. Then, the examiner instructed the participant to open their mouth until told to stop. Once the participant reached a 10-millimeter distance according to a ruler, the examiner led them to hold the position for 3 s, and then close their mouth. Subsequently, the participant was asked to reopen their mouth to the same point as before, as accurately as possible, 3 times. The examiner measured the mouth opening each time with a ruler. The same procedure was repeated for mouth openings of 20 mm and 30 mm.
For intra-rater reliability, the same examiner repeated the test 2 days later. For inter-rater reliability, 2 examiners performed the test for each participant on each study day. Data was collected immediately from the participant’s JPE tests, as described above.
Data analysis
The difference between the starting position (zero) and the point of return in the plane of movement was measured in millimeters. The average of the 3 trials was calculated and taken forward for data analysis. Both AE and the constant error (CE) were determined. The AE was defined as the mean of total deviation from the target, ignoring the positive and negative values.21 The CE was defined as the mean of total deviation from the target, considering positive and negative values.21
Statistical analysis
To evaluate the reliability and validity of our study, we used G*Power, v. 3.1.9.4 (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower) to determine the required sample size. The sample size for the reliability analysis was established based on a significance level of 0.05, a true reliability exceeding 0.7, and a power of 0.8. This resulted in a required minimum sample size of 19 participants.22
Data analysis was conducted using IBM SPSS Statistics for Windows, v. 27.0 (IBM Corp., Armonk, USA). The normality of data distribution was assessed with the Shapiro–Wilk test. The interclass correlation coefficient (ICC) and the standard measurement error (SEM) were also calculated. The two-way mixed model ICC (3,k) with absolute agreement and average measures was used for analysis. According to the interpretation criteria, an ICC score <0.50 indicates poor reliability, 0.50–0.74 indicates moderate reliability, 0.75–0.90 indicates good reliability, and >0.91 indicates excellent reliability.23
To evaluate intra-rater reliability, ICC between the 2 assessment days was calculated for each examiner. The total intra-rater ICC was computed as an average of the 2 examiners. To evaluate inter-rater reliability, ICC between the 2 examiners was calculated for each assessment day. The total inter-rater ICC was computed as an average of the 2 assessment days.
Results
Twenty-two participants (7 men and 15 women; a mean age of 26.2 ±1.5 years; a mean body mass index (BMI) of 23.4 ±2.5) with a mean unassisted mouth opening of 46 ±5mm were included (Table 1).
Table 2 displays the average values of AE and CE for the 3 different target distances (10 mm, 20 mm and 30 mm). For all targets, the CE means were consistently lower than the AE means (1.7 vs. 3.1 for 10 mm; 1.5 vs. 3.2 for 20 mm; and 1.6 vs. 3.1 for 30 mm), whereas the CE standard deviations were consistently higher (3.6 vs. 2.6 for 10 mm; 3.7 vs. 2.5 for 20 mm; and 3.3 vs. 2.3 for 30 mm).
Table 3 reports the intra-rater reliability levels, as indicated by ICCs, based on the mean results of 2 examiners across 3 target distances (10 mm, 20 mm and 30 mm). The results demonstrate that at the 10 mm target distance, the reliability was poor for AE (ICC = 0.38) and moderate for CE (ICC = 0.72). At the 20 mm target distance, both AE and CE showed good reliability (ICC = 0.83). At the 30 mm target, the reliability was moderate for AE (ICC = 0.61) and CE (ICC = 0.74).
Table 4 presents the inter-rater reliability levels evaluated at 3 target distances (10 mm, 20 mm and 30 mm). The results indicate moderate reliability at the 10 mm target distance for AE (ICC = 0.72) and CE (ICC = 0.71). At the 20 mm target distance, the reliability levels were equally good for AE and CE (ICC = 0.77). Finally, at the 30 mm target distance, the reliability levels were equally moderate for both AE and CE (ICC = 0.70).
Discussion
This study aimed to develop a proprioceptive test for TMJ. It was decided to check its reliability first on healthy individuals as a baseline for further studies on the TMD patient population. The results showed that CE was lower than AE for all target distances (10 mm, 20 mm and 30 mm), though with higher standard deviations. Intra-rater reliability varied across the distances, with poor reliability observed for AE at 10 mm, moderate reliability for CE at 10 mm, good reliability for both AE and CE at 20 mm, and moderate reliability for both AE and CE at 30 mm. Inter-rater reliability was moderate at 10 mm and good at 20 mm for both AE and CE, with equally moderate reliability levels at 30 mm.
In their recent study, Dinsdale et al. were the pioneers in assessing proprioceptive performance among patients with intra-articular TMDs in comparison with controls.17 They utilized 50% of maximal mouth opening (MMO) as the targeted range of motion and did not gauge the reliability of their proposed novel JPE test.17 In the present reliability study, the targeted range of motion was not linked to the percentage of MMO, but to 3 distinct distances (10 mm, 20 mm and 30 mm), representing a broader functional range of motion rather than a personalized one. Most essential human jaw functions, such as speech and mastication, operate within this range. Hence, proprioception evaluation is necessary with regard to those target distances. For instance, a patient with a MMO of 25 mm would perform the majority of their daily jaw activities within the 20 mm range (and not 12.5 mm, which is 50%), making it a more clinically meaningful target for assessment.
Interestingly, when analyzing the measurements, CE was consistently lower (more accurate measurement) than AE, while the standard deviations from the mean values were consistently higher. The probable explanation is that the participants consistently tended to make the same error while performing their tasks (crossing the targeted range of motion), but were relatively accurate regarding their overall mean.24 However, the larger standard deviations for CE show that there was higher variability or inconsistency in the magnitude of the errors the participants made during the tasks. Regarding reliability, it may suggest less precise or stable measurements, as there was more significant fluctuation in the errors made by the participants.24 After considering both factors (accuracy and standard deviations from means), CE and AE are equally valid parameters for evaluating JPE.
The only targeted range of motion for which good intra- and inter-reliability was found is 20 mm. In general, the inner range of a joint relies more on the somatosensory input from the muscle spindles (10 mm opening of TMJ), while the outer range on the somatosensory input from the joint mechanoreceptors (30 mm opening of TMJ).25 That could explain why the ultimate somatosensory input is reached in the mid-range (20 mm mouth opening) with an ideal combination of muscles and the TMJ somatosensory input, which results in better proprioceptive performance (accurate and reproducible in terms of reliability). Clinically, most TMD patients are likely to have a MMO of at least 20 mm,26 making this test feasible in a clinical setting.
Limitations
The reliability varied across different targets, requiring further investigation for a deeper understanding. Generalizability could be limited due to the relatively young and physically active participants. The lips of the participants could touch each other and provide an additional tactile input.
Conclusions
This study aimed to address the existing gap by developing a specific and reliable test for JPE in healthy adults, laying the groundwork for future investigations in TMD patients. The between-days intra-rater and within-day inter-rater reliability study protocol adhered to international standards, ensuring robust methodology. The results demonstrated variable reliability across different target distances, with the 20 mm target showing the most consistent and reliable outcomes.
Overall, this study advances our understanding of proprioception in TMJ and lays the groundwork for future research in TMD patients. By establishing a reliable assessment tool in healthy adults, this study paves the way for investigating proprioceptive deficits, and their impact on TMD pathophysiology and treatment outcomes. Future studies should include a larger and more diverse population with different TMDs.
Ethics approval and consent to participate
The study was approved by the ethics committee at Recanati School for Community Health Professions of Ben Gurion University of the Negev, Be’er Sheva, Israel, and all the participants provided written informed consent.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.