Abstract
Background. Dental anxiety presents an ever-present challenge in pediatric dentistry. With the development of dental medicine, new discoveries make undergoing dental therapy easier for patients and reduce their anxiety during dental procedures. Transcutaneous electrical nerve stimulation (TENS) is a therapeutic approach applied to make medical procedures more bearable to patients.
Objectives. This research aimed to examine the possibilities of reducing dental anxiety in children by using TENS.
Material and methods. A total of 125 children aged 9–14 years were included in the study. The respondents were divided into 3 groups. Group A was treated using no anesthesia for the procedure, group B using TENS, and group C with local anesthesia. All respondents underwent a similar dental procedure. The same protocol was used while treating their first permanent molar.
Results. The results show that TENS serves as a distraction to patients, and therefore reduces their anxiety during dental procedures. Anxiety after the procedure was significantly lower in the TENS group as compared to the group that did not receive local anesthesia, and even in comparison with the group that received local anesthesia.
Conclusions. The TENS device proved to be a useful tool for pediatric dentists to distract their younger patients and make them less anxious, and therefore more cooperative during dental treatment.
Keywords: TENS, dental anxiety, pediatric dentistry
Introduction
Examples of anxiety disorders include generalized anxiety disorder, social anxiety disorder (a social phobia), specific phobias, and separation anxiety disorder.1 Traumatic events seem to trigger anxiety disorders in people who are already prone to anxiety.2 Inherited traits can constitute a risk factor.3, 4 For some people, anxiety may be related to a physical health problem.5, 6 At the same time, people may suffer from different anxiety disorders. Common signs and symptoms of anxiety include feeling nervous, restless or tense, a sense of impending danger, panic or doom, a rapid heart rate, rapid breathing (hyperventilation), sweating, shaking, feeling weak or tired, trouble concentrating and an inability to think about anything but current worries, insomnia, gastrointestinal problems, difficulty controlling worry, and the need to avoid things that cause anxiety.7
A fear of dental procedures is a special form of fear, with which the child tries to adapt to the new situation with the medical staff and the medical environment. Given the specificity of the situation, we can expect different reactions from the child than usual. By knowing the stages of child development, and including family, cultural, genetic, interpersonal, and intrapsychic factors, we can understand the change in the child’s behavior. Some fears are completely justified. Pathological forms of fear can be explained as a fear of unknown persons, unknown surroundings, potential pain, or injury. Also, the child may be afraid of being separated from their parents, and react with anxiety in the circumstances unknown so far.8 Sometimes, patients have a negative image of a visit to the dentist, as a punishment for disobedient behavior. In the environment of a dental office, talking about the immediate cause of the child’s bad or good behavior is impossible. However, it is possible to state that pain and negative experiences are potential causes of fear. Dental anxiety is of multifactorial etiology; there is not one or several exclusive factors, but only variables that influence the final picture.8, 9, 10, 11 The final model of behavior is the mutual interaction of the child’s psychological constitution and objective factors in their environment. The child’s ability to cope with stress is influenced by the richness of the affective life and the characteristics of the child’s temperament,12 as well as the potential separation from the mother and the ability to adapt to new situations.13, 14 When successfully establishing contact with the child, intelligence has a great effect. According to some studies, children with a higher IQ quotient feel a lower level of anxiety when visiting the dentist.15 A fear of an unknown situation, the very thought of the dentist, as well as previous experiences during procedures in a dental office, are also responsible for increased anxiety in the child. Conversations with people who have previously had negative experiences also significantly impact the level of anxiety in children. Age, gender and character traits play an important role with regard to the occurrence and manifestation of anxiety. According to some authors, girls are more prone to anxious behavior, and this difference between girls and boys increases proportionally with the child’s age.16, 17 The potentially provoking factors for anxiety are the expected pain, actual pain, the feeling and smell of certain instruments, the sensory sensation when working with a drill, the uncertainty of the overall situation, a feeling of helplessness, the unkindness of the staff, and a feeling of being trapped in the dental unit.18
In dental medicine, treating children and young patients requires a different approach than treating adults. Children still need to be shaped into cooperative patients in the future and are more psychologically liable when undergoing dental treatment. Doctors of dental medicine need to take into account not exposing children to unnecessary trauma, which could lead to developing dental anxiety or a dental phobia in the future. The dental approach when treating children and young adults should be as comfortable and enjoyable as possible to make every visit to the dentist a positive experience to look forward to. Adaptation to the dentist helps in building trust between the child and the members of the dental team. Children with dental anxiety see receiving dental care as a mutual effort between them and the dental team. Developing a sense of control by taking an active role during treatment and communicating their wishes to the dentist helps ease their anxiety. Positive reinforcement is another commonly used behavioral technique in pediatric dentistry. It is believed that small tangible rewards or verbal acknowledgment might provide better cooperation or appropriate behavior from the patient.19 Biofeedback is a technique of providing physiological information in real time. This feedback is referred to as augmented or extrinsic feedback that provides additional information, other than the information from intrinsic sensory receptors. Biofeedback has been proven to have therapeutic effectiveness in reducing dental anxiety and decreasing the negative emotions caused by stress.20 Where dental treatment is urgent, and is combined with a high level of anxiety, sedation is a possibility in the case of younger patients. Sedation is a drug-induced condition in which the patient is rendered free of anxiety. It increases patient cooperation while maintaining the consciousness of the patient.19, 21
This study evaluates the use of transcutaneous electrical nerve stimulation (TENS) in easing dental anxiety in pediatric patients. The TENS device stimulates the nervous system, and serves as an aid to alleviate pain and anxiety in patients undergoing dental treatment. It can also serve as a distraction. It makes children feel in control when treated, as well as more comfortable and cooperative in a dental office.
Transcutaneous electrical nerve stimulation consists in the use of the electrical current produced in a device to stimulate nerves for therapeutic purposes. It covers the full range of currents used to stimulate nerves, although it is often used with a more restrictive intent, i.e., to describe the type of impulses produced by portable stimulators used to treat pain.22, 23 Scientific research shows that high and low frequencies of TENS stimulate the release of endogenous opioids in the central nervous system (CNS) by activating local circuits within the spinal cord or due to the activation of descending pathways of pain inhibition.24, 25
The equipment of the TENS device consists of the main unit, electrodes and lead wires. The TENS unit is a generator of electrical impulses, the lead wires establish an electrical connection by linking the electrodes to the TENS unit, and the electrodes convert the electrical current from the TENS unit into the ionic current in the tissue. The electrodes may be applied for intraoral and extraoral use.
Transcutaneous electrical nerve stimulation is successfully used for analgesia during various dental procedures, such as placing a rubber dam, in restorative dental medicine and endodontics, prosthodontics, oral prophylaxis, and tooth extraction. It is also used to reduce discomfort when administering local anesthesia injections and to relieve periodontal pain associated with orthodontic separation.25
Material and methods
The study included children who had a Class I cavity in the first permanent molar. The minimum age for inclusion was 9 years, and the maximum age was 14 years. The excluding factor was the patient’s cognitive uncooperativeness, i.e., the lack of verbal and non-verbal communication on the child’s part.
The research was approved by the Ethics Committee at the School of Medicine of the University of Zagreb, Croatia, prior to the commencement of the research (No. 05-PA-15-11/2017). All collected data was anonymous, and parents (or guardians) had to sign an informed consent form after being acquainted with the procedure. It was also noted on the forms that all collected data would be strictly confidential. The identities of the research participants were known only to the dentist who conducted the research and the appropriate institution. All children received instructions on how to complete the stress tests immediately before the examination and after the informative interview.
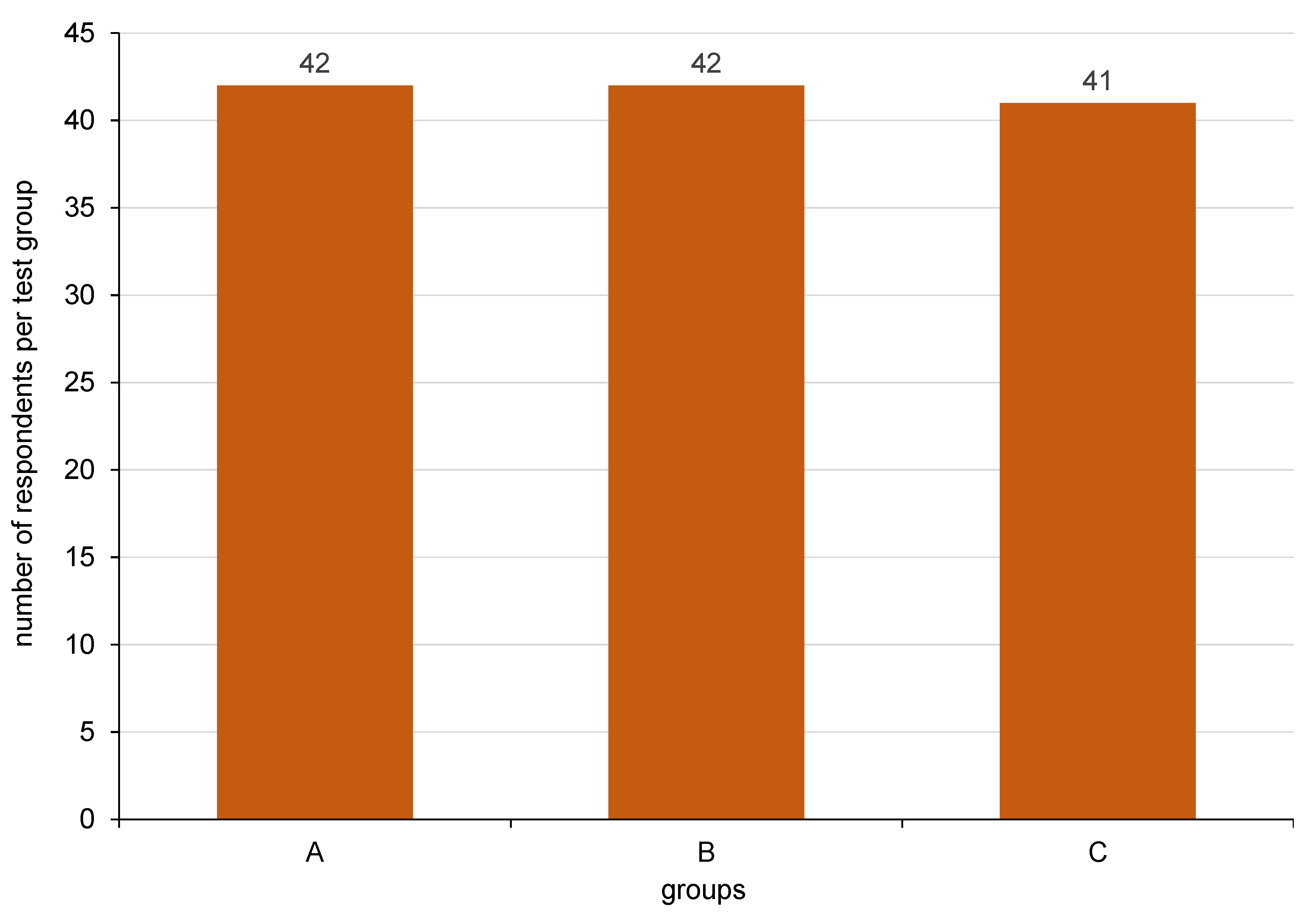
The respondents were divided into 3 groups according to the nature of their procedure and a feeling of pain during dental treatment. Group A included children who were treated using no anesthesia for the procedure. Children from group B had the TENS device applied on their facial skin, and group C included children who received local anesthesia. The distribution of respondents per group is shown in Figure 1.
The prepared cavities were of equal depth in all 3 groups. Dental treatment started with opening the cavity with a round diamond grinder on a pipe with abundant water cooling. The carious contents were removed with a round steel drill with a low number of revolutions of the micromotor. Maximum attention was paid to working intermittently so that the cavity would not get too hot. A feeling of pain in the patients was closely monitored to make sure the children were comfortable during the procedure. The cavity was rinsed with a jet of water, and gently dried with dry air without drops of water or oil. The etching of enamel surfaces with 37% orthophosphoric acid gel was then carried out for 20 s, followed immediately by dentin etching, which lasted for 10 s. All the acidic contents were completely rinsed out of the cavity with a jet of water and the cavity was slightly dried. All surfaces were coated with a dentin adhesive; it was placed on the cavity walls and left for up to 20 s. Then, the excess adhesive was gently removed from the surface with a jet of air so that a shiny surface was obtained. Depending on the manufacturer’s instructions, the dentin adhesive was illuminated and polymerized with a suitable light source. Direct composite materials (Gradia Direct, colors A2 and A3; GC International, Lucern, Switzerland) were used to fill the cavity. The material was placed in layers, and each layer was polymerized for 40 s. The excess material was removed with a suitable diamond bur. Premature contacts were registered with articulation paper. They were removed with a smaller diamond bur. All surfaces of the composite filling were polished with a suitable polishing bur. Interdental floss was used to check the approximate filling surfaces and contact relations. All procedures were performed in the morning, during daylight hours, by one suitably qualified therapist in the pediatric and preventive dental medicine clinic at the Faculty of Dentistry, University of Zagreb. The atmosphere was pleasant. In the waiting room, various cartoons for children were shown on television and the patients were also offered the option to draw.
Local anesthesia was used in the research. The type of anesthesia depended on the jaw in which the tooth was prepared (the maxilla or the mandible). The anesthetic used was Ubistesin™ Forte 4% with adrenaline (40 mg/mL + 0.01 mg/mL) (Pierrel, Capua, Italy). A short needle was used for plexus anesthesia and a long one for mandibular anesthesia. Before the application of anesthesia, the mucous membrane was lightly anesthetized with a topical anesthetic spray. The spray anesthetic used was lidocaine (100 mg/mL). Before applying the anesthetic, the children were asked to close their eyes, so that they would not activate an anxiety reaction by looking at the needle and fearing it.
Before the cavity preparation, the electrodes of the TENS unit were placed extraorally at the place where the mandibular or maxillary nerve is located, depending on which tooth was prepared (in the maxilla or the mandible). The electrodes themselves were attached to the skin using negative-pressure silicone around the electrode. No other adhesive or gel was applied between the skin and the electrode. A conventional TENS mode with a high frequency of 120 Hz was used, producing segmental analgesia with a rapid onset (<30 min) and rapid termination (<30 min). The patients regulated the administration of TENS during treatment by themselves, as shown in Figure 2.
The self-assessment manikin (SAM) scale was used to assess the respondents’ anxiety. The SAM scale measures emotional responses to stimuli in 3 dimensions – pleasure, arousal and dominance (a feeling of control). Each dimension was evaluated on a scale from 1 to 9, determined by 5 corresponding thumbnails and 4 intermediate spaces with described reference points: from “extremely unpleasant” to “extremely pleasant” for pleasure; from “extremely calm” to “extremely agitated” for arousal; and from “extremely submissive” to “extremely dominant” for dominance. The internal consistency for pleasure was 0.63 for the younger group and 0.82 for the older group, 0.98 for arousal –for both groups, and 0.66 for dominance –also for both groups.26
Statistical analysis
The statistical methods used were descriptive. They comprised the calculation of arithmetic means and standard deviations (M ±SD), and the recording of the minimum (min) and maximum (max) values, as well as the calculation of the Pearson coefficient of asymmetry of distribution alpha (α). The two-way analysis of variance (ANOVA) was used to test the significance of differences with regard to the groups of participants and the observation time (before or after treatment).
Statistical analysis was conducted using MS Excel (Microsoft Corporation, Redmond, USA) and IBM SPSS Statistics for Windows, v. 20.0 (IBM Corp., Armonk, USA).
Results
A total of 125 children were included in the research – 40 boys (32%) and 85 girls (68%). The age range of the examined children was from 9 to 14 years, with the average age being 11.53 ±1.78 years.
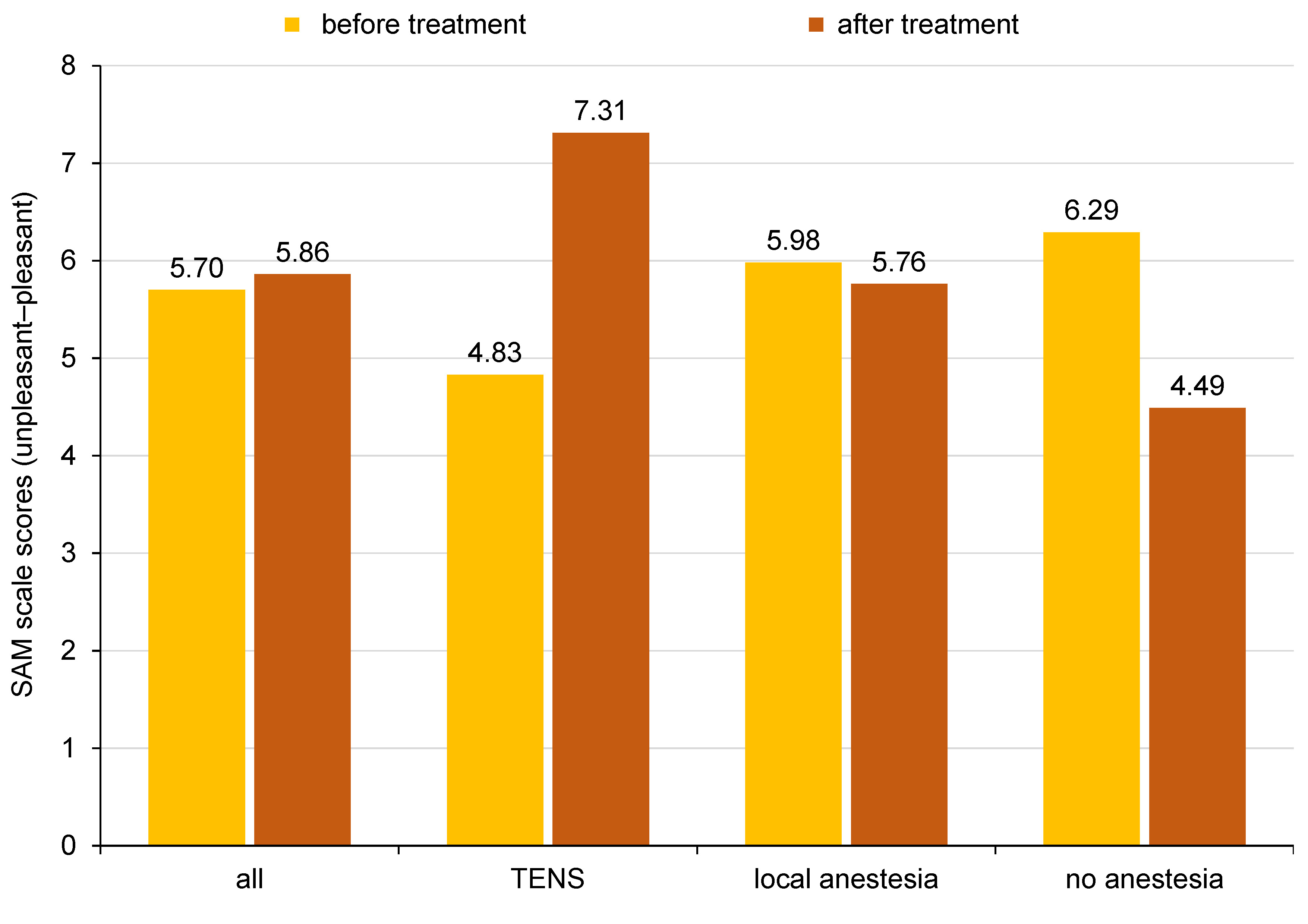
The results in terms of the pictorial SAM scale scores (unpleasant–pleasant) according to the groups of subjects (TENS, with or without local anesthesia) before and after the procedure are shown graphically in Figure 3. The TENS group felt the most pleased after treatment in comparison with the other 2 groups.
The results of the t test for dependent samples, i.e., the significance of the differences in the SAM scale unpleasant–pleasant scores between the 3 groups of subjects before and after the procedure, are shown in Table 1. Statistically significant differences (p < 0.01) with regard to the observation time (before and after treatment) were noted in the TENS group (more pleasant after treatment) and the group with no anesthesia (more unpleasant after the procedure). The young patients described their experiences as more pleasant after dental treatment when using the TENS device.
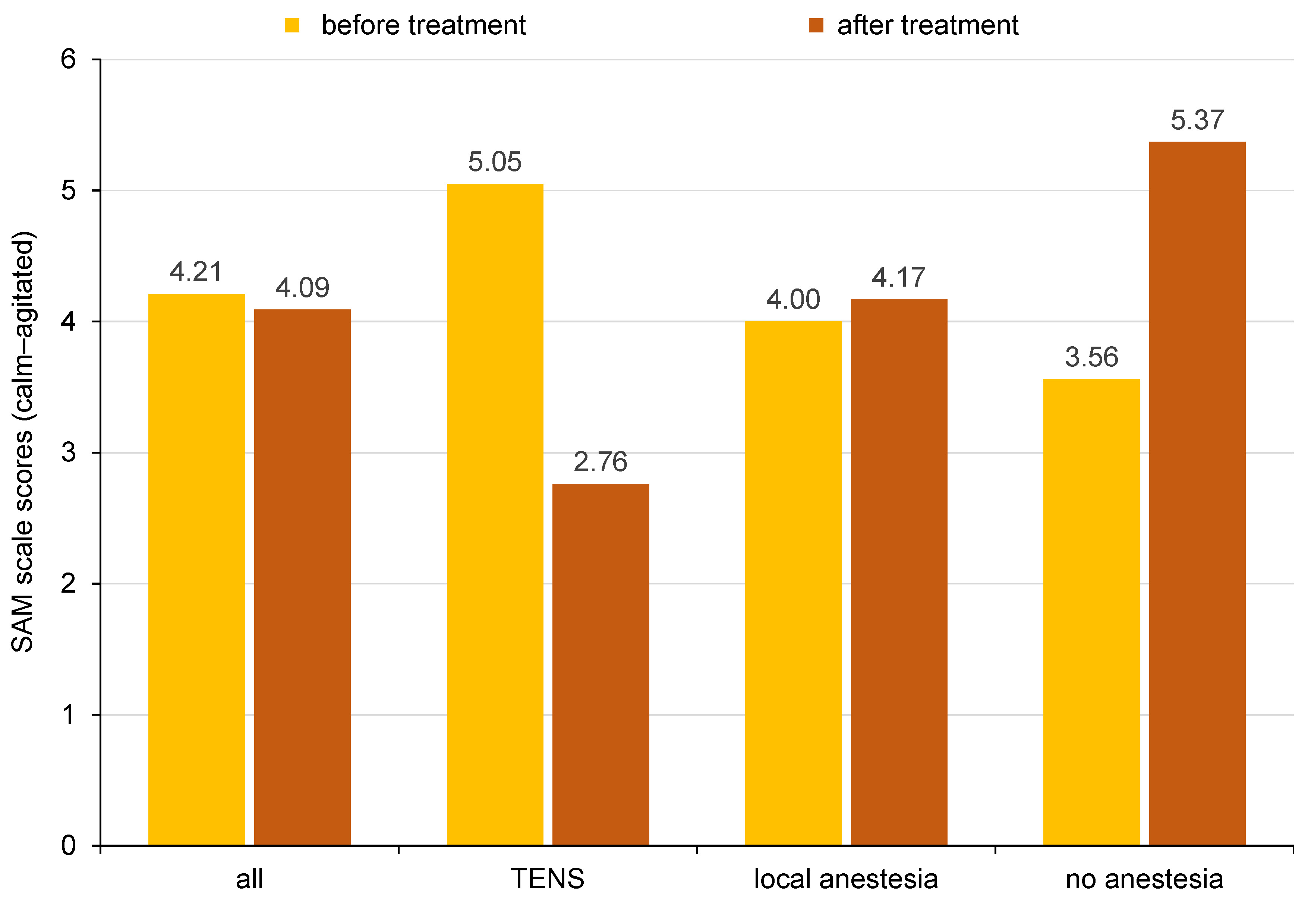
The results in terms of the pictorial SAM scale scores (calm–agitated) according to the groups of subjects (TENS, with or without local anesthesia) before and after the procedure are shown graphically in Figure 4. The respondents felt much calmer after dental treatment when using TENS during the procedure.
The results of the t test for dependent samples, i.e., the significance of the differences in the SAM scale calm–agitated scores between the 3 groups of subjects before and after the procedure, are shown in Table 2. Statistically significant differences (p < 0.01) with regard to the observation time (before and after treatment) were noted in the TENS group (calmer after treatment) and the group with no anesthesia (more agitated after the procedure).
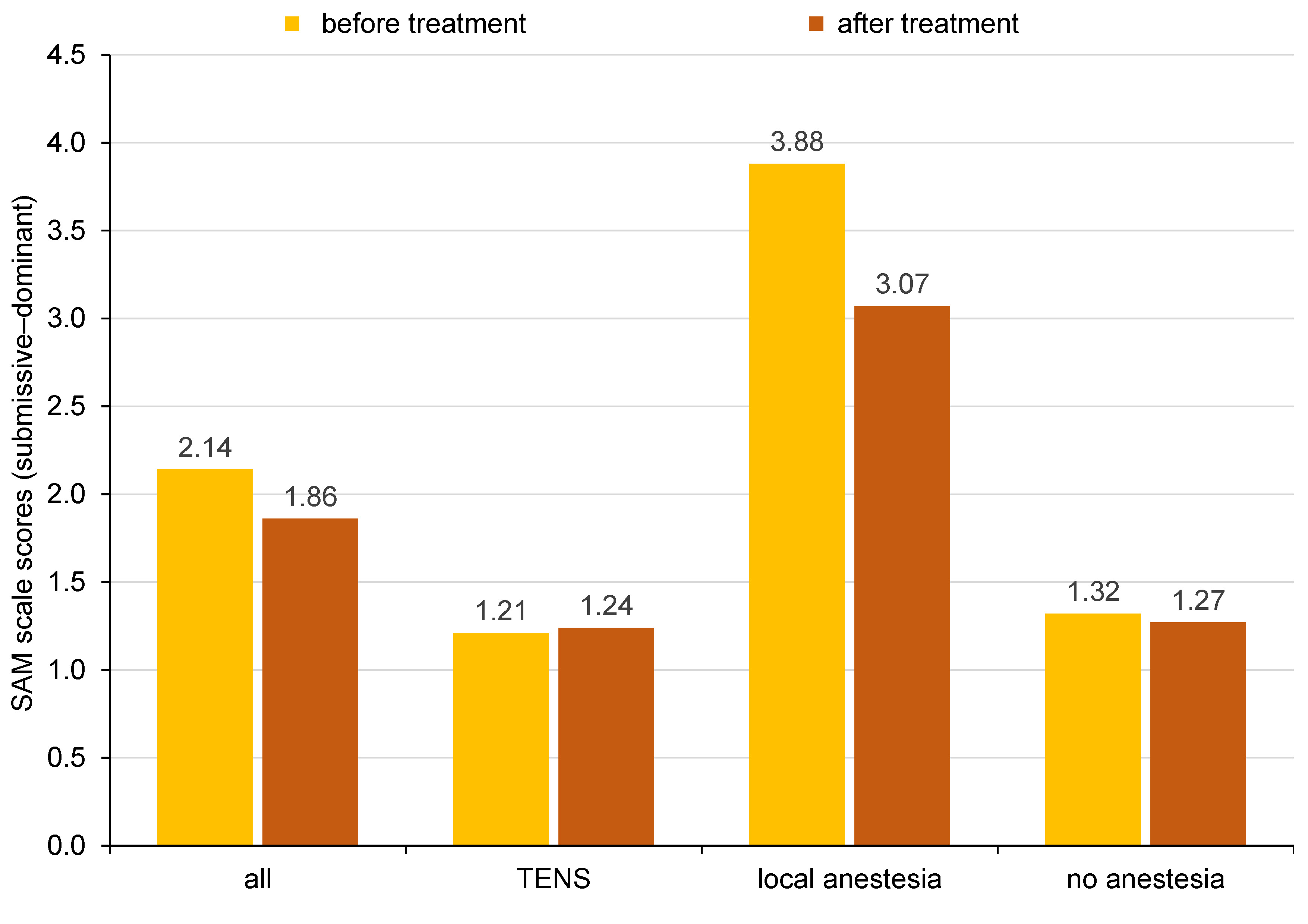
The results as descriptive statistics for the SAM scale scores (submissive–dominant) according to the groups of subjects (TENS, with or without local anesthesia) before and after the procedure are shown graphically in Figure 5. The graph shows the greatest difference in the group which underwent the dental procedure using local anesthesia.
The results of the t test for dependent samples, i.e., the significance of the differences in the SAM scale submissive–dominant scores between the 3 groups of subjects before and after the procedure, are shown in Table 3. A statistically significant difference (p < 0.05) with regard to the observation time (before and after treatment) existed only in the group with local anesthesia. The young patients did not experience a remarkable change in the feeling of dominance after the dental procedure using the TENS device, but felt more dominant after the administration of local anesthesia instead.
Discussion
There are various possible applications for TENS in dentistry, from managing pain during dental procedures to treating chronic pain conditions affecting the maxillofacial region, including trigeminal neuralgia (TGN), post-herpetic neuralgia (PHN) and temporomandibular joint disorders (TMDs), as well as xerostomia, Sjörgen’s syndrome and acute orofacial pain. Saranya et al. compared TENS and microcurrent nerve stimulation (MENS) in the treatment of masticatory muscle pain in 60 patients.27 Patients were randomly divided into 2 groups (A and B) and each group into 2 subgroups (A1, A2, B3, and B4), based on the visual analog scale (VAS) scores. Group A patients were given TENS for 20 min, and group B patients were given MENS for 20 min. Each patient was invited to treatment for 5 days, and the same intensity and frequency were maintained throughout the treatment period. The study showed that both TENS and MENS were equally effective in improving functional mouth opening, although MENS showed a better and more immediate effect in terms of pain relief.27 Side effects, such as tingling and paresthesia, that occur in some patients using TENS are not present when using microcurrent. In 1983, Hansson and Ekblom studied the use of TENS for alleviating acute orofacial pain in 62 patients, using high frequency (100 Hz), low frequency (2 Hz) and placebo TENS.28 The study included patients who suffered from pain for 1–4 days; 38% of patients who received any form of TENS showed a 50% reduction in pain, and 10% of patients who received a placebo showed a pain reduction of more than 50%.28 Steller et al. attempted to determine whether the battery-operated electrical stimulation applied to the hard palate and tongue could initiate salivary flow stimulation in 29 patients with Sjörgen’s syndrome in a double-blinded study.29 They used the device for 4 weeks, 3 times a day, for 3 min. The conclusion was that using TENS was successful only in patients with some residual salivary flow present.29 In PHN, the normal presynaptic inhibition of C fibers does not occur due to the destruction of most of the larger myelinated afferent nerve fibers.30 This causes pain and abnormal skin sensitivity. The use of TENS can increase the activity of the remaining fibers and re-introduce normal inhibition.31 In 1998, Mittal et al. treated 10 patients suffering from PHN.32 They used TENS (70 Hz) for 20 min a day for 10 days. The study showed successful results, reducing 50% of pain in 60% of patients. The authors conclude that patients who respond better to the therapy are those with a shorter duration of PHN.32 The most negative behavior in pediatric patients is a fear of the needles used in local anesthesia.33, 34 Transcutaneous electrical nerve stimulation can help reduce a fear of injections. Studies show that 53–78% of children preferred TENS over local anesthesia.35
The prior experiences of the children in dental offices were not relevant to this study, as the results referred to differences in the anxiety levels before and after the dental procedure. The pain levels were also noted during the procedure, but pain is not mentioned in the results of this research, as it is out of the scope of this paper. All procedures were carried out ethically, taking into consideration the patient’s comfort during dental treatment, as the comfort of the patient is a top priority in a dental office.
The SAM scale showed statistically significant differences in the young patients’ perception of the dental procedure performed with the use of TENS in comparison with administering local anesthesia or using no anesthesia during the dental treatment of the first permanent molar. The results showed that the dental procedure combined with the application of TENS was perceived as more pleasant to the patients, and they felt calmer after the procedure as well. The pleasure aspect and the calmness of the patient during dental procedures may also be beneficial to the dentist carrying out the procedure. Calmer patients, especially younger children, get a lot of positive outcomes from dental procedures, as it is easier to follow protocols such as isolating the treatment site, and focus more on the treatment itself. Young patients who feel pleased and calm during dental procedures will experience less anxiety in the future as well. The feeling of dominance in the young patients who underwent the dental procedure with the administration of local anesthesia is an interesting finding. The children who overcame their fear of needles and local anesthesia will be more cooperative and agree to local anesthesia more easily in the future.
Using the SAM scale in this research proved useful, given that the subjects were young children. The scale is easy to understand, since each dimension is determined by 5 corresponding thumbnails. It was easy for young patients to express their feelings of pleasure, arousal and dominance on the SAM scale used in this research.
The positive experience the study participants gained in a dental office will increase the likelihood of their cooperation during the following dental treatment procedures in the future. The anxiety levels may be lower, thus reducing the risk of developing a dental phobia when the patients grow up. Positive experiences in a dental office are of great importance, since they shape a cooperative attitude in patients, encourage them to take care of their oral health and approach regular checkup appointments at the dentist responsibly. Also, such patients may have a positive influence on people in their close environment, such as siblings or – in the future – their own children.
This study confirmed that TENS was a successful distraction method for dental procedures. The results show that the group in which the TENS device was applied felt less anxiety after the procedure, in contrast to the groups with and without local anesthesia, where the patients felt more anxiety after the procedure. This could be explained by the fact that the group without anesthesia felt little or insignificant fear before the procedure, and felt some unexpected pain during treatment, which caused an increase in the level of anxiety after the procedure. A similar situation occurred in the group that received local anesthesia. Regardless of the painlessness of the procedure, the fear of the needle used during anesthesia caused an increase in anxiety among the subjects. The TENS device, used during the entire dental procedure, distracted the examinee’s attention from the procedure itself and the sensations connected with it. Given that each child has a different pain tolerance threshold, the same amount of electricity could not be given to all subjects equally, and for this very reason, each subject could control the strength of the current individually. The children were focused on the tingling sensation caused by the mild administration of electricity and on dosing the electricity so that the treatment would be pleasant and not painful. The TENS device also served as a “toy” which the child had fun with during the procedure. Transcutaneous electrical nerve stimulation can be used as a mild analgesic during various dental procedures, although it cannot completely replace local anesthesia. It can also exert the placebo effect, as the self-administration of the electrical current can distract attention from the procedure being performed on the tooth. The assumption is that the amount of electricity that children administer to themselves is not high enough to cause discomfort to the child. The pain was closely monitored throughout the procedure to make sure the patient was comfortable. However, the pain-alleviating effect of the TENS device was not within the scope of this research. This can be pointed out as a limitation of the present study. The recommendation for future studies on the TENS device in pediatric dentistry would be to explore its effectiveness in pain management in comparison with the conventional use of local anesthesia for dental procedures.
Conclusions
Positive experiences in a dental office from a young age are crucial for ensuring patient cooperation in the future. Reducing dental anxiety is one of the many challenges dentists face when treating young patients. If not properly addressed, dental anxiety in children can develop into a dental phobia in adulthood, potentially leading to the neglect of oral health due to fear. The TENS device may serve as a useful tool for dentists to help distract younger patients and make them more comfortable, and even excited about visiting a dental office.
Modern dental medicine emphasizes noninvasive and innovative approaches to treatment, focusing on painless, pleasant procedures that help reduce patient anxiety. Preventing oral diseases has never been more important, and minimizing dental anxiety can play a key role in encouraging patients to attend regular checkups. The TENS device may offer a valuable solution for promoting oral health in both young patients and adults.
Ethics approval and consent to participate
The research was approved by the Ethics Committee at the School of Dental Medicine of the University of Zagreb, Croatia, prior to the commencement of the research (No. 05-PA-15-11/2017). All collected data was anonymous, and parents (or guardians) had to sign an informed consent form after being acquainted with the procedure.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
All collected data was strictly confidential. The identities of the research participants were known only to the dentist who conducted the research and the appropriate institution.
Use of AI and AI-assisted technologies
Not applicable.