Abstract
Background. Temporomandibular disorders (TMD) constitute a serious health problem that can have a negative effect on patients’ lives, impair work performance, and result in work absences and restrictions in daily activities. Therefore, it is of great importance not only to employ appropriate diagnostic and therapeutic procedures in the case of patients suffering from TMD and/or sleep bruxism (SB), but also to analyze the impact of different medical and non-medical factors on the occurrence of such conditions, as the proper modification of these factors may mitigate the severity of patients’ symptoms.
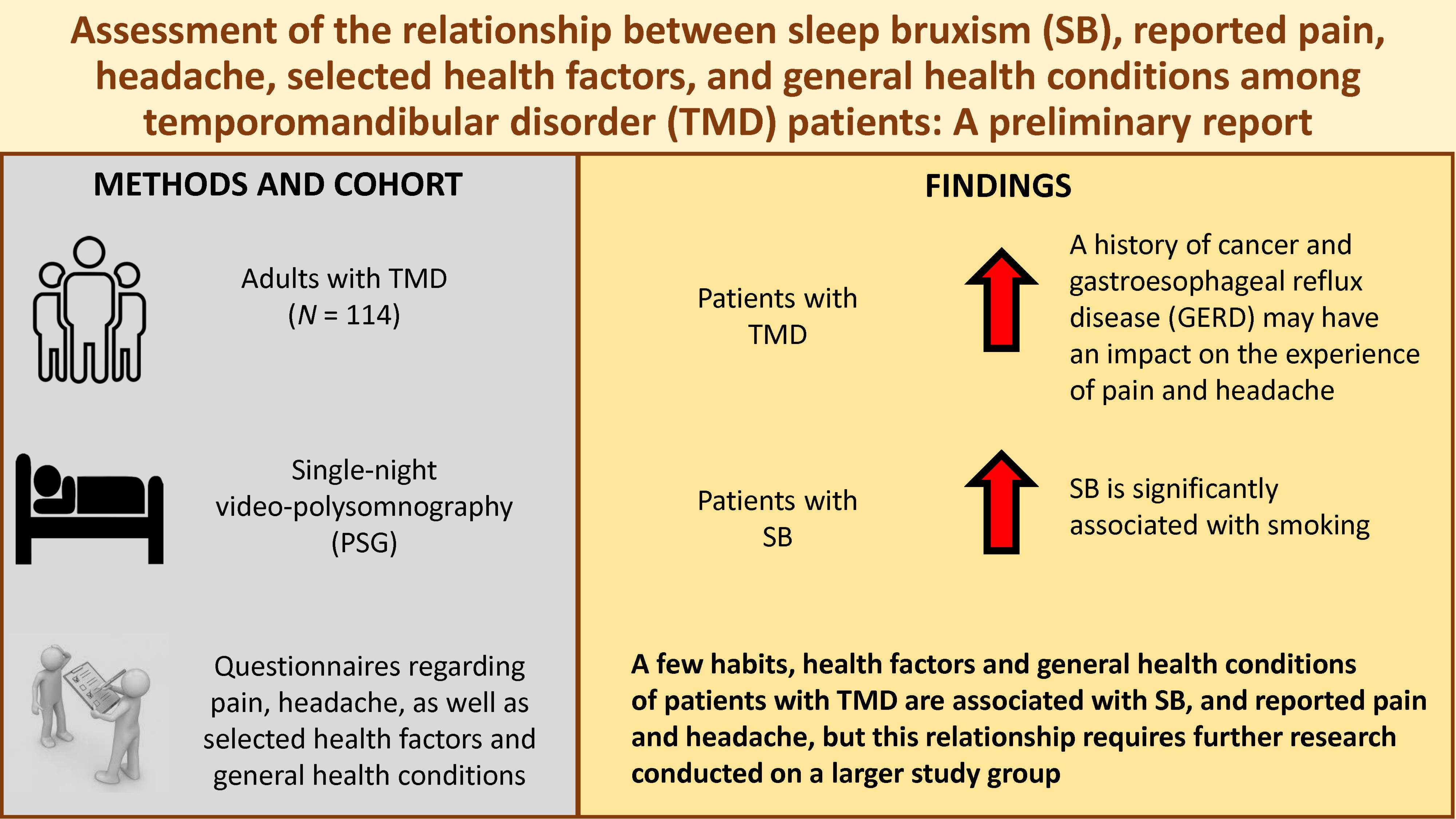
Objectives. The present preliminary study aimed to assess the relationship between SB, reported pain and headache, selected health factors, and general health conditions among TMD patients.
Material and methods. A total of 114 patients from the Outpatient Clinic for Temporomandibular Disorders in Wroclaw, Poland, had single-night video-polysomnography (PSG) performed. The patients completed questionnaires about their pain experience, headache and health condition, including the presence or history of diseases such as hypothyroidism, arterial hypertension, cancer, diabetes, myocardial infarction, stroke, gastroesophageal reflux disease (GERD), and were asked about the frequency of alcohol consumption, smoking, caffeine use, and physical activity. The collected data was statistically analyzed.
Results. It seems that among patients with TMD, a history of cancer and GERD may have an impact on the experience of pain and headache. Smoking was significantly associated with the occurrence and intensity of SB.
Conclusions. A few habits, health factors and general health conditions of patients with TMD are associated with SB, and reported pain and headache, but this relationship requires further research conducted on a larger study group.
Keywords: habits, TMD, general health, headache, sleep bruxism
Introduction
Temporomandibular disorders (TMD) include masticatory muscle or temporomandibular joint (TMJ) pain, limited jaw movements, joint sounds, such as clicking or crepitus, myofascial pain, and headache.1 They are considered the 2nd most common cause of oral and facial region pain, following odontalgic pain.2 Additionally, it is ranked as the 2nd main cause of musculoskeletal pain, after chronic low-back pain.1 The prevalence of TMD is estimated to be between 5% and 12% in the general population, with a higher incidence of up to 30% among young adults.3 In the Polish population, approx. 55.9% of individuals experience at least one symptom of TMD.4 Gender differences are apparent, with women more commonly affected by TMD in the Polish population.4
Sleep bruxism (SB) is a repetitive jaw muscle activity characterized by the clenching and/or grinding of the teeth, which is classified under sleep-related movement disorders (SRMD) in the International Classification of Sleep Disorders – Third Edition (ICSD-3).5 Sleep bruxism is a common phenomenon worldwide, with a prevalence of 8–13% in the general population.6
Orofacial pain (OFP) encompasses a heterogeneous group of conditions, such as dental, mucosal, musculoskeletal, neurovascular, and neuropathic pain.7 In OFP and headache, chronic pain is defined as the pain occurring more than 15 days per month and lasting more than 4 h per day for at least the last 3 months.8, 9
The aim of this preliminary study was to assess the relationship between SB, reported pain and headache, selected health factors, and general health conditions among TMD patients.
Material and methods
Participants
The project was approved by the Ethics Committee of Wroclaw Medical University, Poland (KB-794/2019). All of the study participants were fully informed about the purpose of the study and agreed to take part in it. The study was carried out following the Declaration of Helsinki for experiments involving humans.
Patients with TMD were examined using single-night video-polysomnography (PSG). They were also interviewed about their health condition, with regard to the presence or history of diseases such as hypothyroidism, arterial hypertension, cancer, diabetes, myocardial infarction, stroke, gastroesophageal reflux disease (GERD), and were asked about the frequency of alcohol consumption, smoking, caffeine use, and physical activity.
Inclusion criteria
The patients were included in the study if they met the following criteria: age above 18 years; the presence of OFP or headache, as determined using the Graded Chronic Pain Scale (GCPS), the Headache Impact Test-6 (HIT-6), the Migraine Disability Assessment (MIDAS), the short-form McGill Pain Questionnaire (SF-MPQ), and the TMD pain screener; and willingness to participate in the study.
Exclusion criteria
The exclusion criteria were as follows: addiction to a drug or a medication; using medicines that significantly affect the function of the nervous and muscular systems; severe systemic diseases and severe mental disorders, including significant mental disabilities or the presence of cancer; less than 4 h of sleep recorded using PSG; pregnancy; the presence and treatment of sleep apnea; and the lack of consent to participate in the study.
Video-polysomnography examination
The intensity of bruxism was assessed using the bruxism episode index (BEI), indicating the number of bruxism episodes per hour of sleep. The cut-off points were determined in accordance with the guidelines of the American Academy of Sleep Medicine (AASM) ICSD-3: BEI < 2 – irrelevant SB; BEI of 2–4 – mild to moderate SB; and BEI > 4 – severe SB.10
Pain assessment
Pain intensity was determined using validated questionnaires, such as SF-MPQ,11 GCPS,12 MIDAS,13 HIT-6,14 and the TMD pain screener.15
Health questionnaire
The patients from the study group were asked to complete a questionnaire on general health and habits, which consisted of 10 parts regarding the patient’s medical history, diseases in the family, the medications taken, the patient’s eating habits, alcohol consumption, smoking, caffeine use, and physical activity, as well as demographic data.
Database
The participants’ medical history, questionnaire responses and PSG data were entered into a database using Microsoft Excel (Microsoft Corporation, Redmond, USA). The elements of the database were subjected to statistical analysis.
Statistical analysis
The U Mann–Whitney correlation coefficient was used to check the relationships between the variables. The choice of the coefficient was dictated by the fact that the variables did not have a normal distribution. A p-value for a correlation coefficient below 0.05 was considered significant. Statistica™, v.13.1 (StatSoft, Krakow, Poland), was used for the statistical analysis of the data. The prediction of the sample size (N) was established with the use of the power.cor function and the genefu package (https://rdrr.io/bioc/genefu/man/power.cor.html).
Results
Characteristics of the study sample
Age and gender
A total of 114 adult participants were included in the study (72 women and 42 men). The female-to-male ratio in the group was 1.71:1. All participants were Caucasians, aged 21–71 years (mean age: 37.67 years).
Reported pain
The level of pain severity was determined by the participants using 4 independent questionnaires, as illustrated in Table 1.
Severity of sleep bruxism
The percentage distribution of the BEI values according to gender is shown in Table 1.
Reported selected health factors and general health conditions
Hypothyroidism occurred in 2 study participants (1.75%). Arterial hypertension was reported by 5 patients (4.39%). In all cases, the patients declared that they took medications regularly and their blood pressure was regulated. Four patients (3.51%) had an oncological history. Three respondents were treated for diabetes (2.63%). The study group did not include any patients reporting a history of myocardial infarction or stroke. However, as many as 33 patients (28.95%) reported the occurrence of GERD.
Forty-two patients admitted to drinking alcohol, which constituted 36.84% of the study group; 5 patients (4.39%) stated that they consumed alcohol regularly and 37 patients (32.46%) only occasionally. There were 12 cigarette smokers, representing 10.53% of the study group. Twenty patients (17.54%) admitted to drinking coffee regularly, while 6 patients (5.26%) drank coffee occasionally, which gives a total of 26 patients, i.e., 22.8% of the respondents. Physical activity was reported by 64 patients (56.14%), with only 11 patients (9.65%) exercising every day, 19 patients (16.67%) reporting physical activity 3–4 times a week, 28 patients (24.56%) practicing 1–2 times a week, and 6 patients (5.26%) practicing less than once a week.
Reported selected health factors and general health conditions and reported pain
The data on the environmental factors were compared with the level of pain reported by the patients in the GCPS, MIDAS, HIT-6, SF-MPQ questionnaires, and the TMD pain screener, using the Mann–Whitney U test (Table 2).
There were no statistically significant relationships between the level of pain and hypothyroidism, arterial hypertension, diabetes, alcohol consumption, smoking, caffeine use, and physical activity (p > 0.05).
However, the Mann–Whitney U test showed a statistically significant relationship between reported pain and a history of cancer. This relationship occurred for the HIT-6 questionnaire (p = 0.037) and the MIDAS questionnaire (p = 0.032). No statistically significant relationships for the GCPS and SF-MPQ questionnaires, and the TMD pain screener were noted (p > 0.05).
We also noticed a statistically significant relationship between the level of pain reported by the patients and the co-occurring GERD. The last correlation concerns the GCPS questionnaire (p = 0.039). This means that patients suffering from GERD report higher levels of pain and pain-related disability. There were no such statistically significant relationships with regard to the HIT-6, MIDAS and SF-MPQ questionnaires, and the TMD pain screener (p > 0.05).
Reported selected health factors and general health conditions and sleep bruxism
Statistical analysis with the use of the Mann–Whitney U test was also performed to investigate the relationships between hypothyroidism, arterial hypertension, cancer, diabetes, GERD, alcohol consumption, smoking, caffeine use, and physical activity and the occurrence and severity of SB (Table 2). The analysis showed that only in the case of smoking can we speak of a statistically significant relationship (p = 0.016).
Among cigarette smokers, only 1 patient had BEI < 2 (8.33% of all smokers). Similarly, mild to moderate SB (BEI of 2–4) occurred in 1 patient (8.33%), while 10 patients (83.33%) were classified as presenting severe bruxism due to BEI > 4.
Discussion
Østensjø et al. found that the factors influencing the occurrence of painful TMD are female gender, living in urban areas, complaining of severe menstrual pain, and frequent headaches.16 Women not only reported pain more often, but the intensity of the pain was greater.16 The results regarding gender are consistent with the findings of our study, in which the predominant group were women, and in this group, the pain was more intense and caused greater disability than in men. However, the authors of the abovementioned study reported that physical activity could have an alleviating effect on the pain felt.16 Many other studies also point to the reduction of pain in the group of people regularly engaging in physical activity.17 In our study, the relationship between physical activity and reported pain was not statistically significant, although physical activity certainly had a greater impact on pain reported in GCPS (p = 0.065) than on the occurrence of SB (p = 0.271).
A large study started in 2006 – the OPPERA project (Orofacial Pain: Prospective Evaluation and Risk Assessment) – aimed at identifying risk factors for the development of painful TMD.18 According to this research, TMD develop at a disproportionate rate in people with relatively poor health, whether in the form of comorbidities or otherwise pain, poor sleep quality or smoking.18
Grozdinska et al. in their study conducted on a group of 119 women, including 52 women in the study group diagnosed with Hashimoto’s disease and 67 healthy people in the control group, noticed markedly increased incidence of TMD in the study group.19 Muscle pain and stiffness were observed in 45 patients from the study group (86.5%) and 33 (63.5%) had disk displacement with repositioning.19 The results of that study showed that the prevalence of TMD, especially of muscle disorders in patients with Hashimoto’s thyroiditis, is higher than in the control group (p < 0.001).19 Our research did not show statistically significant relationships between reported pain and thyroid diseases, or between SB and thyroid diseases, but the study group included only 2 patients with hypothyroidism, so it was impossible to draw clear and valuable conclusions regarding this dependence.
Miettinen et al. in their work, in which the study group consisted of 8,678 participants (148 women and 8,530 men), tested with the use of questionnaires TMD symptoms, health behavior and background/demographic factors, and noticed higher prevalence for all TMD symptoms (except TMJ clicking) in the female population.20 Smoking was significantly associated with TMD symptoms, except for TMJ clicking. The consumption of alcohol at least once a week was significantly associated with facial pain, TMJ pain and TMJ clicking. The use of snuff was significantly associated with facial pain.20 The results presented by Miettinen et al. are consistent with those of Sanders et al., who showed that smoking was associated with TMD in women, but only in young adulthood.21 We can find contradictory results in Wänman’s study, which concluded that smoking was not related to the presence or development of the signs and symptoms of TMD among an adult population (30–65 years of age).22 In their research, Castroflorio et al. show that smoking, more than alcohol, seems to have an impact on the occurrence of SB.23 Similar conclusions come from our study. The Mann–Whitney U test confirms a relationship between smoking and SB at p = 0.016. However, with regard to pain and smoking, no statistically significant relationship was found (p > 0.05). Alcohol consumed both occasionally and regularly did not increase the intensity of pain (p > 0.05) and does not seem to have a significant impact on the occurrence of SB (p > 0.05). Also, the amount of coffee consumed did not have a significant influence on the intensity of pain, or an increase in the frequency and intensity of SB (p > 0.05), which is contrary to the findings of Frosztega et al., who reported that habitual coffee consumption was a risk factor for an increased intensity of SB.24
Our research shows that GERD may be associated with pain in patients with TMD (p = 0.039). Similar conclusions come from the work of Li et al., who report that symptomatic GERD is associated with chronic TMD pain.25 According to previously conducted research, the acidification of the esophagus not only increases the rhythm activity of the masticatory muscles, as well as the clenching and/or grinding of the teeth during sleep,26 but also increases the activity of the muscles during waking hours.27 Also, Nota et al. in their systematic review indicate a significant association between GERD and bruxism, mostly awake bruxism (AB).28
Kanclerska et al. emphasize the role of the dentist in making a proper diagnosis and providing care to the patient.29 They state that dental screening is necessary for patients with arterial hypertension, especially those presenting with the symptoms of SB. According to the researchers, nonapneic hypertensives showed greater SB intensity, altered sleep architecture, increased snoring, and decreased mean oxygen saturation as compared to normotensives.29 Martynowicz et al. in their study aimed to assess the intensity of SB in patients with arterial hypertension.30 A total of 70 adults participated in this study: 35 patients with hypertension (the study group); and 35 normotensive subjects (the control group). Data was recorded using a portable home cardiorespiratory polygraphy device. The BEI in the study group was found to be significantly higher as compared to the control group.30, 31 In our study, we did not demonstrate statistically significant relationships between arterial hypertension and reported pain, or between arterial hypertension and SB. However, it is worth mentioning at this point that the study group included an insufficient number of patients suffering from arterial hypertension to correctly determine this relationship, especially in the absence of a control group.
The study conducted by our research team has few limitations, but it allows us to outline the direction of further work on the topic discussed. First of all, a limitation of the study are small groups in terms of the incidence of hypothyroidism, arterial hypertension, cancer, diabetes, and GERD among patients with TMD or SB, and patients with a history of myocardial infarction or stroke. An additional limitation is the lack of a control group. Another limitation of the study is the fact that the occurrence and severity of pain were determined using questionnaires, as was TMD determined using the TMD pain screener. The occurrence of bruxism and the analysis of sleep quality were determined through a PSG examination, which is a great advantage of this study, while the PSG recording was carried out on the first night spent in hospital, without an adaptation night. Therefore, we are aware that the study has a high risk of interpretation bias and is a preliminary report.
Conclusions
A few habits, health factors and general health conditions of patients with TMD are associated with SB, and reported pain and headache, but this relationship requires further research conducted on a larger study group.
Ethics approval and consent to participate
The project was approved by the Ethics Committee of Wroclaw Medical University, Poland (KB-794/2019). All of the study participants were fully informed about the purpose of the study and agreed to take part in it.
Data availability
The datasets supporting the findings of the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.