Abstract
Background. The durability of the materials used in the prosthesis is a determining factor for the success of the rehabilitation.
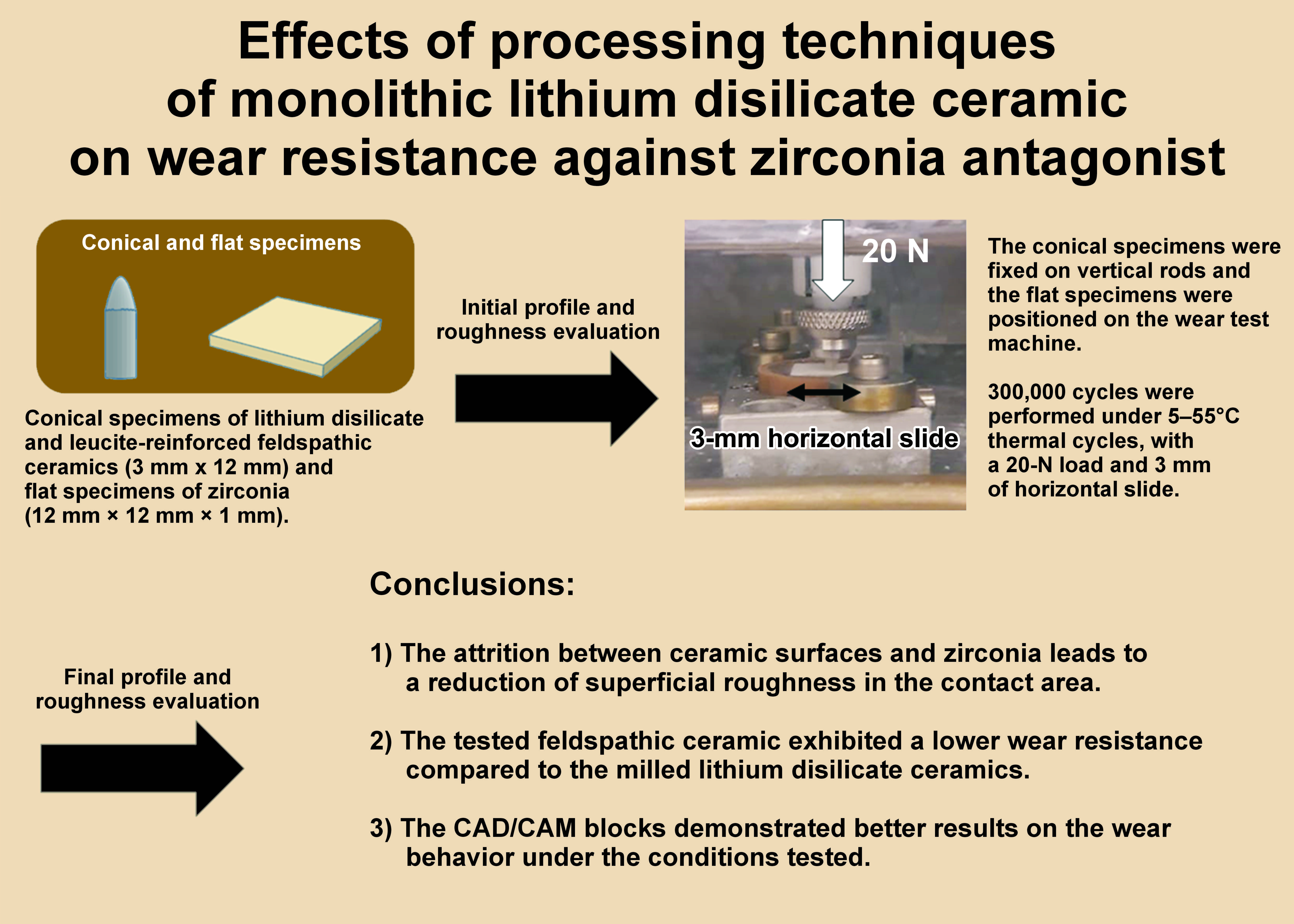
Objectives. The aim of the study was to evaluate the wear resistance of monolithic lithium disilicate ceramics processed by heat pressing and computer-aided design/computer-aided manufacturing (CAD/CAM) methods, with a leucite-reinforced feldspathic ceramic processed by CAD/CAM serving as a control group.
Material and methods. Monolithic lithium disilicate ceramic samples, processed as CAD/CAM milled blocks or heat-pressed ingots, were tested against flat zirconia antagonists. A CAD/CAM leucite-reinforced feldspathic ceramic was used as the control specimen. Conical specimens were made for each group and subjected to thermomechanical cycling with a flat zirconia antagonist. The roughness of the conical and flat specimens was evaluated before and after thermomechanical cycling. The height loss in the conical specimens was also assessed. The data concerning height loss was analyzed using one-way analysis of variance (ANOVA) and Tukey’s post hoc test. The data obtained from the roughness analysis of the conical and flat samples was evaluated using a linear model of repeated measures and Bonferroni complementary test.
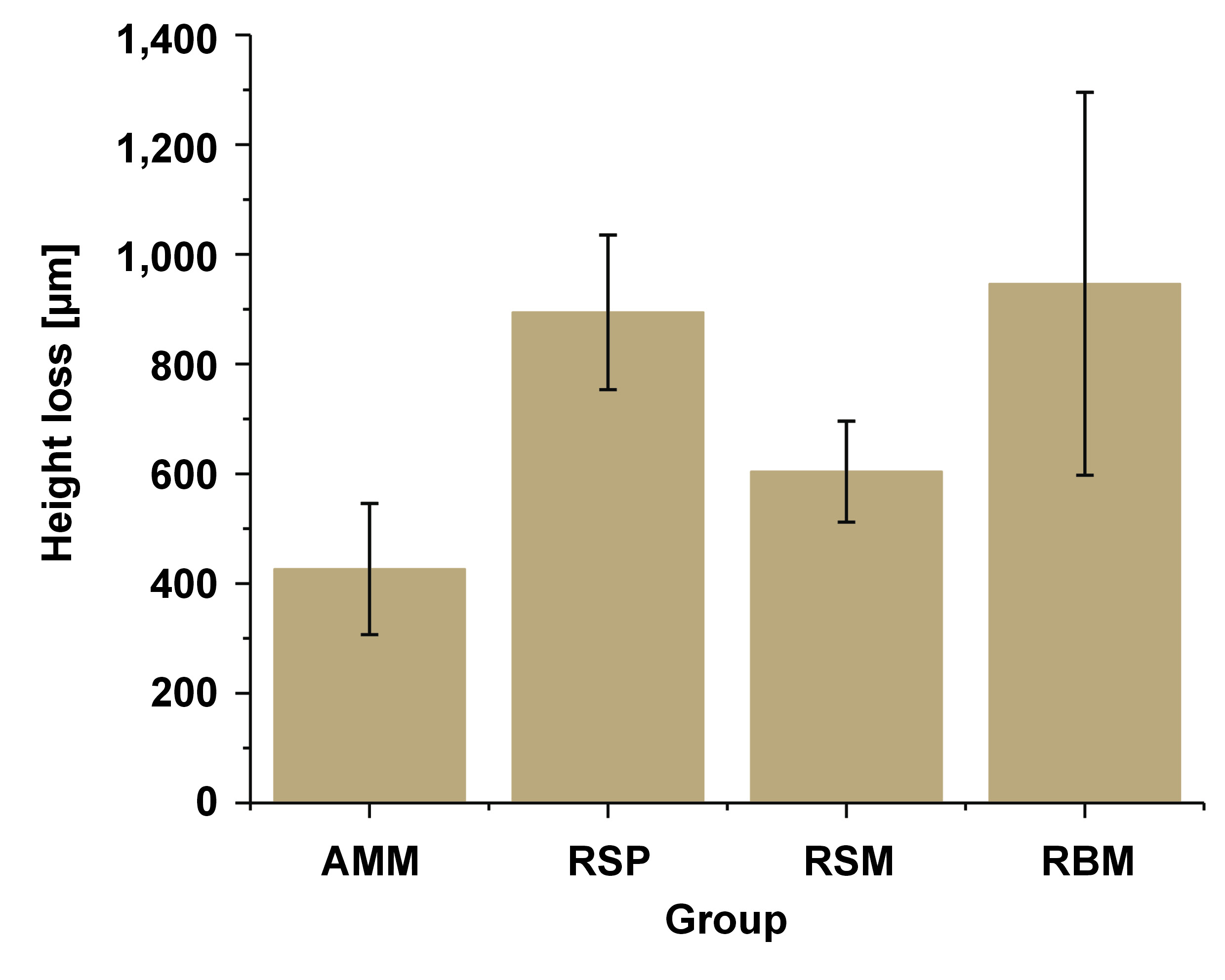
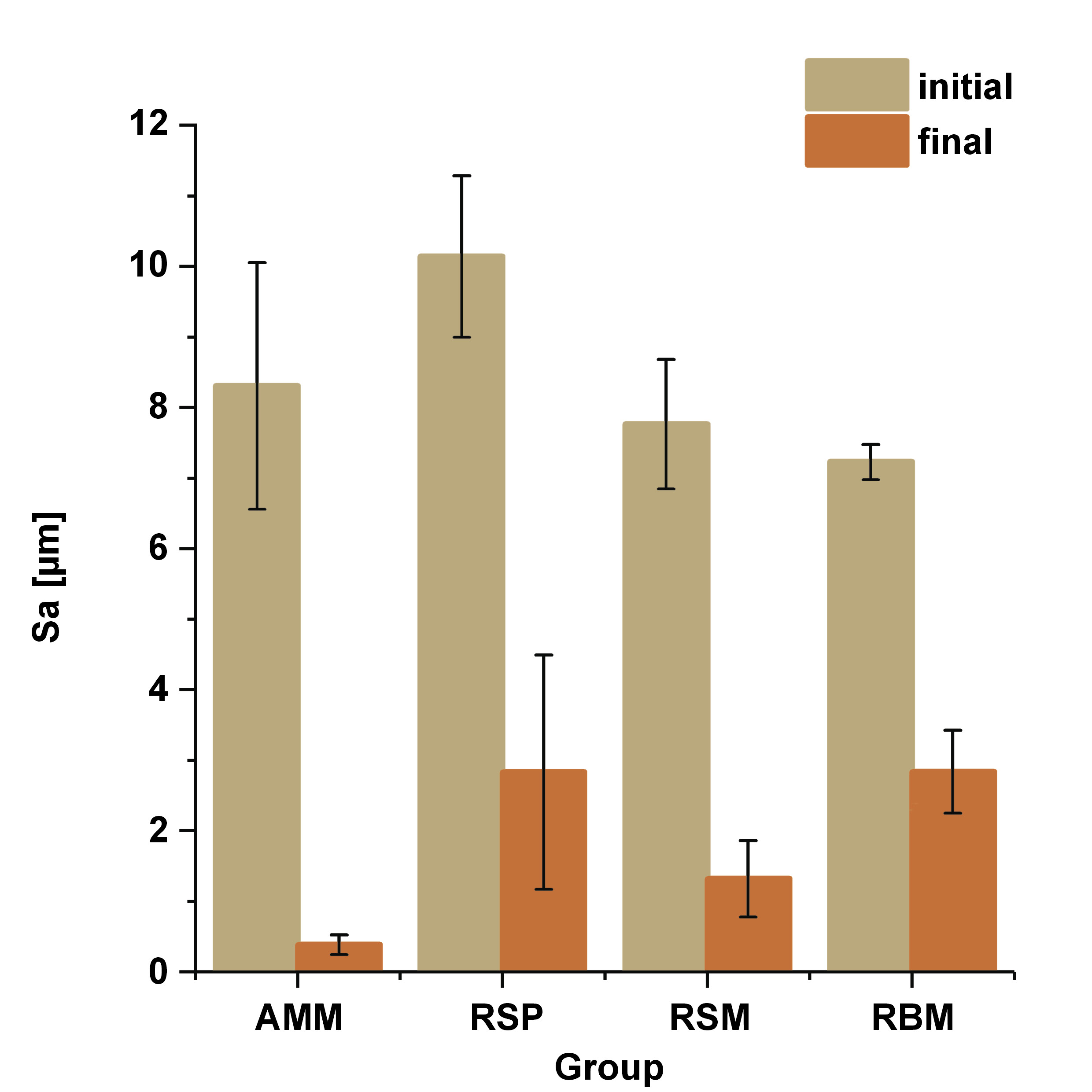
Results. A significant difference was observed in the extent of height loss among the ceramics under consideration. Amber® Mill (AMM) exhibited a lesser extent of height loss in comparison to Rosetta® SP (RSP) (p = 0.010) and Rosetta® BM (RBM) (p = 0.005), yet it demonstrated congruence with Rosetta® SM (RSM) (p = 0.525). Additionally, a significant difference was noted between the initial and final roughness values for both the conical (p = 0.017) and flat (p < 0.05) samples, with the final roughness values being lower than the initial values.
Conclusions. The attrition between ceramic surfaces and zirconia led to a decrease in superficial roughness (Sa). In the context of lithium disilicate ceramics, milled ceramics demonstrated superior performance in terms of wear behavior. The tested feldspathic ceramic exhibited a lower wear resistance compared to the milled lithium disilicate ceramics; however, its wear behavior was similar to that of the heat-pressed lithium disilicate ceramic.
Keywords: dental porcelain, computer-aided design, dental restoration wear, dental materials, lithium disilicate
Introduction
Complete dental ceramic restorations have become a component of oral rehabilitation due to their aesthetic properties, durability and biocompatibility.1 However, the benefits achieved by restoring a dental element with ceramic materials may be overshadowed by potential wear occurring in the natural dentition or in restorations in the opposing teeth.1, 2 Furthermore, few studies have evaluated the wear resistance of these materials, which is an important factor given ceramics’ propensity for wear and subsurface crack formation. These cracks can disseminate, resulting in the loss of fragments.3 Wear is a factor that is related to occlusal stability and, consequently, can influence the clinical success of the restoration.2, 4
The wear of the materials used in oral rehabilitation when subjected to the forces resulting from dental contact during chewing, swallowing and speaking can result in the flattening of the cusps of posterior teeth and the incisal shortening of anterior teeth, leading to decreased aesthetics and functionality. Consequently, it is important that the materials used in clinical settings exhibit wear characteristics similar to those of dental enamel to ensure optimal long-term outcomes.5 The wear of a ceramic prosthesis is a continuous and progressive phenomenon, which is related to material properties and structures, such as surface quality and manufacturing, as well as the environment to which the prosthesis is subjected. The environmental factors include the pH value of saliva, chewing habits, the type of food ingested, and the magnitude of the chewing forces.6
Wear is a complex phenomenon that is influenced by several factors, including the microstructural characterization of the materials, the environment in which they are inserted, and the interaction of materials in their environments. The consequences of this condition are the loss of dental anatomy and a reduction in the vertical dimension of occlusion. This, in turn, can lead to physiological and pathological disorders, as well as aesthetic and functional impairment of the restorations.7
Thus, the present study aims to evaluate the wear resistance of monolithic lithium disilicate ceramics processed using heat press and computer-aided design/computer-aided manufacturing (CAD/CAM) methods. A leucite-reinforced feldspathic ceramic processed by CAD/CAM will serve as a control group. The factors involved in the wear process, such as roughness and height loss, will be evaluated using a thermal and mechanical cycling test against zirconia antagonists. The null hypothesis posits that there are no differences between the ceramics tested.
Material and methods
Preparation of the specimens
The present study employed a pin-on-block design. Conical ceramic specimens were used, with flat zirconia specimens serving as antagonists. The composition and manufacturing method of the materials used in this study are described in Table 1.
For each ceramic type, specimens in conical shape and rounded tip (3.0 mm × 12.0 mm) were fabricated (n = 5 per ceramic type). Firstly, the ceramics for milling were cut using a diamond trephine with a 3-mm internal diameter (Cortag Revolution Tools, Mogi Mirim, Brazil) and an electric motor (Dremel 3000®; Bosch Power Tools B.V., Breda, Netherlands). This instrument was utilized under conditions of abundant water cooling, resulting in the production of 3-mm diameter cylinders. A cylindrical diamond bur was used in conjunction with a dental drill (D700; Dabi Atlante, Ribeirão Preto, Brazil), with an angle fixed at 30 degrees to the long axis of the cylinder to obtain a conical shape. The ceramic cylinder was affixed to a base in the MultiCP 2000 device (Department of Dental Materials and Prosthesis, School of Dentistry of Ribeirão Preto, Brazil) during the milling process. Subsequently, the specimens were polished using specialized ceramic finishing and polishing rubbers (EVE Diapol; Odontomega, Ribeirão Preto, Brazil) to obtain the rounded shape at the tip.
The obtained specimens were duplicated using heavy (Variotime Easy Putty; Heraeus Kulzer, Hanau, Germany) and light (Variotime Light Flow; Heraeus Kulzer) silicone to create organic wax patterns. These patterns were embedded in casting material (IPS PressVEST Speed; Ivoclar Vivadent, Liechtenstein, Germany) and used for the fabrication of pressed ceramic specimens identical to those obtained for CAD/CAM ceramics.
The specimens to be manufactured by heat pressing (Rosetta® SP (RSP); HASS Corp., Gangneung, South Korea) were vacuum-pressed according to the parameters recommended by the manufacturer. They were divested and blasted with glass beads (110-µm grain size and 4 bar/2 bar fine pressure), while Amber® Mill (AMM) (HASS Corp.) and Rosetta® SM (RSM) (HASS Corp.) were crystallized following the manufacturer’s guidelines. Due to the characteristics of Rosetta® BM (RBM) (HASS Corp.), it was determined that crystallization was not necessary after milling. The finishing and polishing of the ceramics was performed with the use of diamond polishers (EVE Diapol Kit; Odontomega).
For the fabrication of flat zirconia specimens, zirconia blocks (Ceramill® ZI; Amann Girrbach AG, Koblach, Austria) were cut to the dimensions of 14.4 mm × 14.4 mm × 1.2 mm using a diamond saw (IsoMet 1000; Buehler, Lake Bluff, USA) and sintered (inFire HTC speed; Dentsply Sirona, São Paulo, Brazil). The heating was initiated at a rate of 10°C/min, reaching a plateau at 700°C and holding for 10 min. Subsequently, the heating was continued at 8°C/min until a second plateau was attained at 900°C, following a holding period of 30 min. The heating was then resumed at a rate of 8°C/min until a third plateau was reached at 1450°C, where it was maintained for a duration of 120 min. Subsequently, the temperature was reduced at a rate of 5°C/min to 200°C. The final dimensions of the samples were 12 mm × 12 mm × 1 mm. The polishing process was executed using #280, #400 and #600 sandpaper, as well as diamond polishers. The samples were then embedded in acrylic resin (VIPI FLASH; VIPI, Pirassununga, Brazil) in polyvinyl chloride (PVC) rings with an outer diameter of 25 mm and a height of 25 mm.
Evaluation of roughness
The tip of the conical samples was analyzed with confocal microscopy (Olympus LEXT OLS4000; Olympus Europa Holding GmBH, Hamburg, Germany) before and after wear tests, and surface roughness values of this region were obtained. The surfaces of the flat samples were also analyzed, and it was possible to obtain the roughness values of the region formed by wear and control areas. The magnification used for the analyses was ×5.
Wear test
Zirconia antagonists and conical specimens were positioned on a two-body wear testing machine (Biocycle; Biopdi, São Carlos, Brazil). The conical specimens were affixed to vertical rods within the machine, and they underwent vertical movements with a 20-N load. The flat specimens were fixed to the base, which slid horizontally for a distance of 3 mm. The frequency of these movements was 2 Hz, and they were performed for 300,000 cycles, which represents 1 year of masticatory function at the average human masticatory frequency.7, 8 Concurrently with mechanical cycling, thermal cycles ranging from 5°C to 55°C were performed. The experimental tank reached maximum capacity in 20 s, maintained that level for 60 s and then discharged in 25 s. This resulted in the completion of 734 thermal cycles in each group.
At the beginning and conclusion of the wear tests, the profiles of the conical specimens were traced using a profile projector (Nikon Profile Projector 6C; Nikon, Tokyo, Japan) at ×10 magnification on a transparent sheet. The positioning of the specimens was standardized before and after the tests. The height loss of the conical specimens was measured using a pachymeter with 0.01-mm precision (Mitutoyo Sul Americana Ltd., Suzano, Brazil). The mass loss was determined by calculating the difference between the final and initial values.
Statistical analysis
The data concerning mass loss and height loss was assessed using the Shapiro–Wilk normality test (p > 0.05) and analyzed according to one-way analysis of variance (ANOVA) and Tukey’s post hoc test. The data obtained from the roughness analysis with confocal microscopy of the conical and flat samples was analyzed using a linear model of repeated measures and Bonferroni complementary test. The α level used for the comparisons between the groups was set at 5%. The statistical analysis was conducted using the IBM SPSS Statistics for Windows software, v. 20.0 (IBM Corp., Armonk, USA). The statistical power for the between-group comparisons regarding height loss (95%) and roughness (98.8%) was calculated.
Results
The results for height loss and superficial roughness (Sa) evaluations are presented in Table 2, and Figure 1 and Figure 2. The statistical analysis revealed a significant difference in height loss after thermocycling between the groups tested (p = 0.003). Tukey’s post hoc test showed that AMM demonstrated a reduced degree of height loss in comparison to RSP (p = 0.010) and RBM (p = 0.005), and exhibited similarity to RSM (p = 0.525).
Visible chipping of specimens was observed in the RSP (1 event) and RBM (1 event) groups. However, these events did not impede the progression of the test. The roughness results of the conical samples before and after wear tests are illustrated in Figure 2. The statistical analysis revealed that for the conical specimens, roughness values exhibited a statistically significant difference between the groups (p = 0.001), between the evaluated times (initial condition × final condition) (p < 0.05) and between the group-time interactions (p = 0.015). The surface roughness data of the conical specimens indicates a difference between the initial values. Amber® Mill demonstrated a similarity to all specimens (p > 0.05), however, RSP, a heat-pressed ceramic, was different from RSM (p = 0.029) and RBM (p = 0.006), 2 milled ceramics. After thermocycling, a statistically significant difference was detected between AMM and both RSP (p = 0.005) and RBM (p = 0.005), and similarity was identified between AMM and RSM (p > 0.05). A reduction in surface roughness was noted in all groups after thermocycling (p < 0.05). A comparison of the mean difference of the conical specimen roughness reveals a discrepancy between the RSP group and all other groups (AMM: p = 0.001, RSM: p = 0.002 and RBM: p = 0.025).
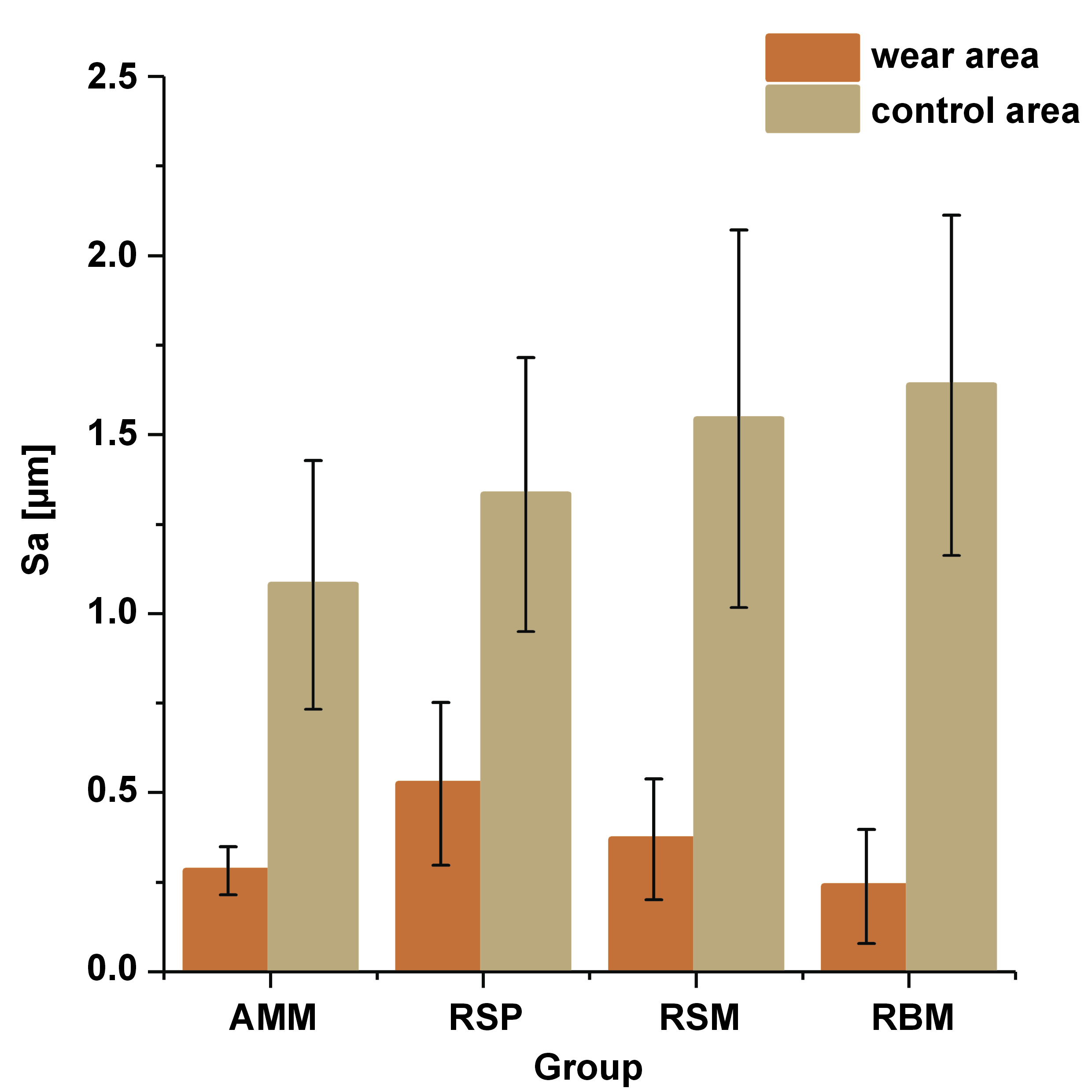
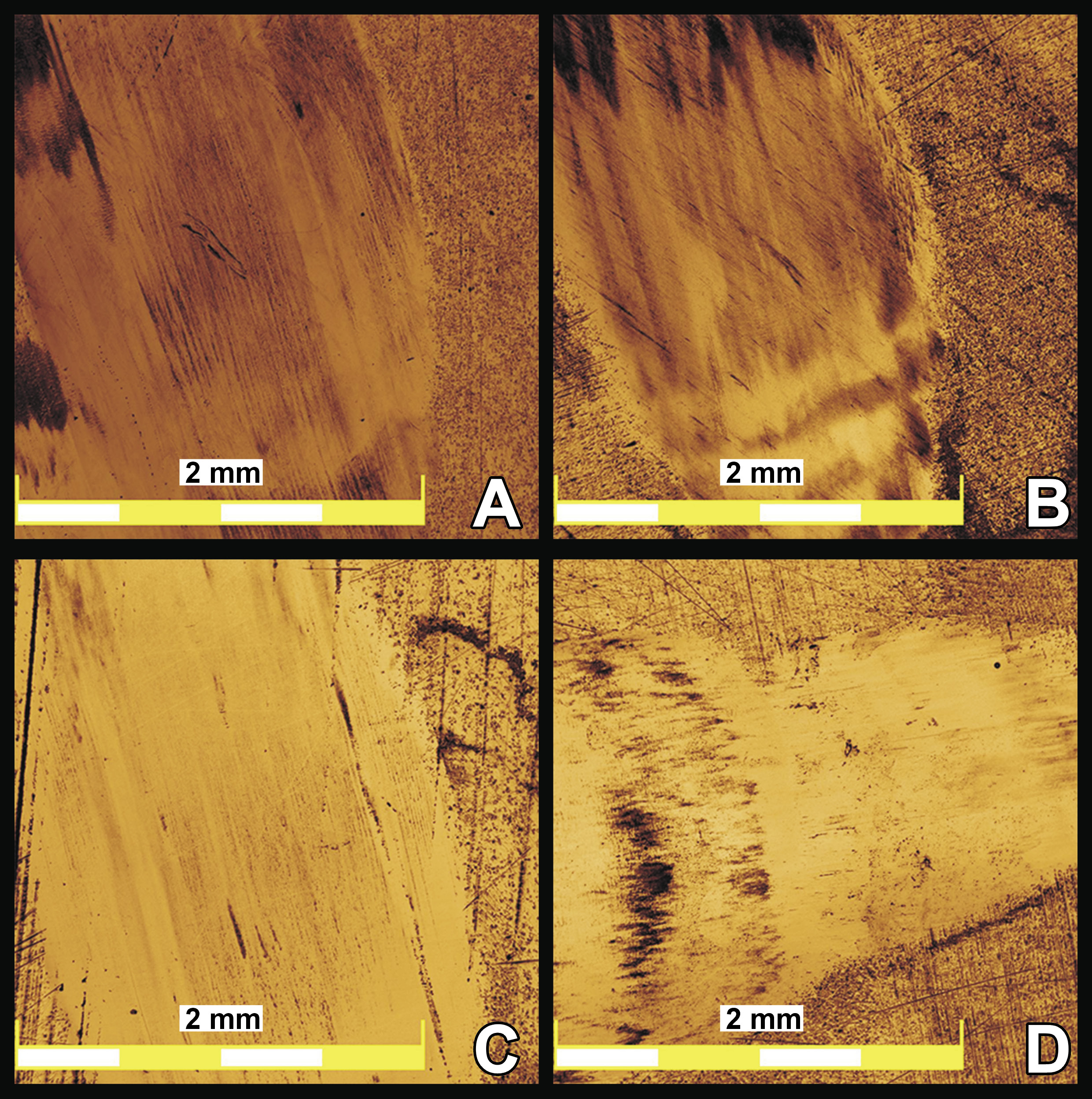
The analysis of the data collected on the flat specimens enabled a comparison of a wear area with control areas that exhibited no wear action, as illustrated in Figure 3. A statistically significant difference was identified between the roughness levels observed in the control area and those measured in the wear area. Specifically, the roughness levels in the wear area were found to be lower than those in the control area (p < 0.05). However, no significant difference was detected between the groups (p > 0.05). Figure 4 presents the images of the zirconia surface obtained by confocal microscopy following the wear test.
Discussion
The present study aimed to evaluate the behavior of lithium disilicate ceramics fabricated with the use of heat press and CAD/CAM methods. A leucite-reinforced feldspathic ceramic was used as a control, and zirconia was utilized as an antagonist material. The conical specimen is a representation of the cuspid occluding on the flat antagonist, and thermomechanical cycling is a representation of the masticatory movement between them. The roughness of the surfaces in contact during the simulated masticatory movement was evaluated before and after the test. The null hypothesis was rejected based on the findings concerning height loss, which revealed a difference between the ceramics tested.
The present study employed a pin-on-block methodology, simulating the contact of the tip of the cuspid, a moment of attrition and disocclusion, added to thermal cycling. The movements performed in this study attempt to simulate the materials and conditions encountered during the application of masticatory forces in localized functional contacts in occlusal rehabilitations. The representation of masticatory forces is methodologically complicated and, in the tests performed in the literature, is described as the continuous cyclic contact between 2 bodies.8, 9, 10 The same difficulty is encountered when simulating the temperature variations occurring inside the oral environment. In this study, cycles ranging from 5°C to 55°C were used to model these variations. A variety of methodologies have been employed in studies on the impact of wear tests on dental ceramics. These methodologies vary with regard to several factors, including the applied force, contact geometry, the role of lubricants, and the number of cycles. This diversity can be attributed to the development and utilization of different cycling devices to replicate the stress conditions of the material within the oral environment.7, 11
Research has demonstrated that heat-pressed ceramics exhibit superior performance in terms of crown fracture rates, flexural strength, fatigue strength, and survival rate when compared to other materials.12, 13, 14 These properties can be attributed to the enhanced surface finishing achieved through heat pressing. However, the current study demonstrated that CAD/CAM ceramics exhibited superior performance in mitigating height loss, with the exception of RBM. The behavior of the RBM group can be attributed to its composition, which consists of a feldspathic ceramic reinforced by leucite. The wear resistance of lithium disilicate exceeds that of feldspathic ceramics, as indicated by the findings of several studies.15, 16 In the present study, lithium disilicate ceramics, with the exception of RSP, performed better than the leucite-reinforced feldspathic ceramic (RBM). The composition of feldspathic ceramics is predominantly characterized by the glass matrix, making them highly aesthetic and suitable for use in the rehabilitation of anterior teeth.5, 17 However, the aesthetic characteristics are improved at the expense of the mechanical properties of this material.5 In the context of wear, crystalline particles with dimensions below 5 µm have a strong influence on surface roughness.1, 7 Lithium disilicate ceramics consist of ultra-fine particles (4 µm) arranged in various orientations.7, 18 This could reflect the wear of the flat samples due to friction between the bodies involved in the wear process and also to changes in the coefficient of friction.1, 7 A similar phenomenon occurs when analyzing ceramics containing leucite, where the size of the particles, their distribution, concentration, and density of the glass matrix influence the wear resistance.1, 16
Heat-pressed ceramics can present porosities in their structure, a consequence of the manufacturing process. These porosities promote the propagation of microcracks,3, 19 which may underlie the occurrence of chipping in the RSP ceramic group. Chipping in RBM may be associated with the milling process and structural changes that occur in the production process.14 Chipping of ceramic prostheses is not an atypical event and can be caused by surface failures, which reduce the critical loads that generate larger fractures.16 Milling performed on CAD/CAM blocks can induce a cascade of events on the surface and in the structure, leading to lateral and radial fractures, chipping, and introduction of residual stress. These phenomena are potential initiators of fracture and consequent failure of the obtained restorations.14, 20 The crystallization process is not necessary for RBM, which is just milled. Crystallization has a positive influence on the presence of microfractures on the ceramic surface when compared to non-crystallized ceramics.21, 22 This process could influence the degradation of the glass matrix and generate more favorable residual stresses at the glass-crystal interface.22 The influence of these factors on the results obtained in this study is a subject for further investigation, as the lithium disilicate ceramics that underwent this process (AMM and RSM) had smaller height loss values.
One of the wear mechanisms encountered in clinical settings is the two-body wear, defined as the direct contact between the prosthesis and the antagonist, or contact between the tooth and the prosthesis during the process of saliva swallowing or speech. Abrasive wear is a reaction caused by the friction between 2 bodies with distinct surfaces in continuous or dynamic contact. This reaction is evidenced by the plow pattern on the evaluated surface.1, 6 In the present study, the pattern can be visualized in the flat specimens (Figure 3), indicating frictional wear between the surfaces. The three-body wear occurs when food is chewed and there is dynamic tooth–food–prosthetic contact.2, 6 The literature includes methodologies that use artificial saliva, glycerin and polishing pastes to perform the tests, characterizing the wear between 3 bodies and changing the coefficient of friction.1, 7, 8, 23 Multiple microcontacts, represented by the roughness of an antagonist body or debris from the abraded surface at the sliding surface, can be associated with an increase in wear intensity.16 A number of studies have indicated a correlation between wear and material characteristics, compositions, and the presence of external factors such as abrasives and surface roughness.1, 2 In the present study, the wear between 2 bodies was conceptualized. However, even with abundant irrigation of the wear area by the thermomechanical cycling machine, a layer of debris remains between the conical and the flat specimens, which may cause additional wear. Furthermore, the presence of microscopic cracks is indicative of three-body wear.3, 24
Surface roughness is an important factor to be evaluated. Elevated surface roughness values can lead to a number of changes in the mechanical properties of materials, including the occurrence of caries, food impaction and excessive wear of antagonist and adjacent teeth.2, 25 The obtained results indicate a significant decrease in surface roughness of the conical samples after thermomechanical cycling across all the evaluated groups. The surface characteristics of the material are a significant factor in the initial stages of the wear process. However, upon altering the surface characteristics, the material properties become the determining factor in wear behavior.26 Roughness analyses performed using confocal laser scanning microscopy on the flat specimens revealed significant differences between the wear and control areas, with lower roughness values observed in the wear area for all the groups evaluated. Roughness and the coefficient of friction can change depending on the duration of a test and the materials being tested, which may explain the low association between these 2 properties and the amount of wear.22, 26, 27 With the methodology employed in this study, there was a decrease in the roughness of conical and flat specimens in all groups after thermocycling.
It is challenging to evaluate the different variables that contribute to enamel wear and the materials involved in a single study. The majority of studies use dental enamel or enamel analog materials as antagonists.2, 3, 5, 7 Thus, it is intriguing that studies of commercially available materials are performed against various antagonists, thereby ensuring homogeneity in the evaluations. This homogeneity is not guaranteed when using natural dental enamel,28 as it is typically obtained from multiple donors. In this study, zirconia was utilized as an antagonist to the materials tested. Although the use of zirconia as an antagonist could be regarded as one of the study’s limitations, its implementation ensured that the ceramics were exposed to identical test conditions for the assessment of wear. Although this combination is not the most frequent in the buccal cavity, the homogeneity of the antagonist ensured more standardized conditions during the tests. This is in contrast to the conditions present in the mouth, where natural variations in human dental enamel are observed.
This study is subject to other limitations regarding the fractographic interpretation of the materials after testing. Confocal laser scanning microscopy analysis is intended to measure the depth of irregularities in the materials. This analysis does not enable to obtain high-resolution images of their surface, which infers that possible cracks located in the wear areas are interpreted as roughness data.13, 21, 23 Another analysis that could be performed to help interpret the obtained values is the evaluation of step height in the antagonist specimens. However, this analysis could not be performed on the flat specimens.
Conclusions
In consideration of the study’s limitations, it can be concluded that the attrition between ceramic surfaces and zirconia leads to a reduction in Sa in the occlusal contact area. Furthermore, within the group of lithium disilicate ceramics, milled ceramics demonstrated better results in terms of wear behavior under the conditions tested. The enhanced homogeneity of CAD/CAM blocks for machining has been demonstrated to ensure superior resistance to wear. Therefore, clinicians should consider these materials a priority. The findings of the study indicated that the tested feldspathic ceramic exhibited a lower wear resistance compared to the milled lithium disilicate ceramics. However, its wear behavior was similar to that of the heat-pressed lithium disilicate ceramics.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.