Abstract
There is a strong connection between malocclusion and obstructive sleep apnea (OSA).
Keywords: orthodontics, obstructive sleep apnea, temporomandibular disorders, malocclusion
In recent years, obstructive sleep apnea (OSA) has become a challenging medical problem. More and more patients are diagnosed with this disorder, and the awareness of OSA is increasing among physicians as well as dentists. Obstructive sleep apnea is a disorder in which, during sleep, muscles relax so much that they can block the airways, so by definition this is a muscular condition. Since the dentist is a frequently visited healthcare provider, often, it is them who can screen the patient for the diagnosis of OSA.
Some recent studies indicate that the phenomenon could be strongly linked with temporomandibular disorders (TMD), which are also related to muscular tension, with bruxism being the manifestation of such disorders; the coincidence of those conditions is well known in today’s medical world.1, 2, 3 Temporomandibular disorders comprise the disorders of temporomandibular joints (TMJs), the masticatory muscles and the surrounding structures.4, 5 The reduced sleep time and the low quality of sleep increase the risk of TMD and other disorders.2 Those disorders might be related to many general medical conditions, i.a., many systemic diseases, like hypertension, hyperinsulinism and rheumatoid arthritis.1, 2, 3, 4, 5 Temporomandibular disorders also strongly affect sleep, lowering its quality. They might be related to the occurrence of OSA as well. Impaired sleep quality and insufficient oxygenation during sleep lead to the worsening of the psychosocial condition of individuals, causing general health problems and hindering the patient’s well-being.6 On the other hand, the psychosocial background of TMD is undeniable, as stress is one of the most common factors influencing TMJs and the orofacial muscles, as mentioned in the literature.4, 7 Also, the presence of oral behaviors, such as sleep bruxism, causes hypoxia in the patient, leading to sleep-related breathing disorders (SRBD) of various intensity.8 Yet, this relationship needs further investigation, as the definition of bruxism has changed; it is no longer considered ‘parafunctional behavior’, and instead, 2 conditions are differentiated – sleep and awake bruxism.9 The orofacial complex could be compared to a structure of communicating vessels, in which one element strongly influences another. Therefore, researchers should investigate any connections between those elements.
Recently, there has been a strong dispute on whether or not TMD are connected with malocclusion in any way, and if orthodontic treatment influences TMJs. In some studies, TMD are reported as the 2nd most common (after apical root resorption) complication of orthodontic treatment,10, 11 though the connection between TMD and malocclusion, as well as orthodontic treatment, is highly disputable and not quite clear.12 Some researchers found a strong relationship between malocclusion and TMD,13 while others deny the existence of it.14 The connection is inexplicit, although in the maxillofacial and orofacial regions, the parts of the stomatognathic system obviously impact each other. It is evident, though, that TMD have a multifactorial background and the definition of their origin is challenging.1, 2, 3, 4, 5 Today, we are witnessing a swing of interest with regard to TMD; the crucial issue seems to be determining the cause of those problems, as this might be the key to establishing successful treatment methods for patients in the future.
As mentioned above, TMD may co-occur with OSA. The main cause of OSA is the narrowing of the airways. However, the new guidelines suggest avoiding surgical treatment in OSA patients, as it may cause considerable discomfort.15
It is a well-known fact that orthodontic treatment may affect the dimensions of the airways.16 Also, the coincidence of malocclusion and OSA remains a huge problem.17 Both maxillary and mandibular advancement enlarges the dimensions of the upper airways. In Class II malocclusion, the functional advancement of the mandible, generating its forward movements, increase the airway volume measured at the 3rd cervical vertebra (C3).16 On the other hand, the traction of the maxilla in Class III malocclusion also increases the airway volume.17 Furthermore, it has been shown that OSA patients present with narrower maxillae. In children, the potential treatment can be guided by maxillary expansion with both removable and (preferably) fixed appliances, while in adults, surgically assisted maxillary expansion is required.18 Also, while in children it is possible to use functional treatment for Class II patients and maxillary protraction for Class III patients, in adults, the problem becomes more complex. In many of those patients, the only chance for stable orthodontic treatment is orthognathic surgery, especially according to face-driven orthodontics, which is a current treatment trend. The trend is also known as ‘facially driven orthodontics’, and consists in preserving or enhancing facial features, while improving the functional aspects, i.e., ensuring the correct contact of the teeth, wide airways and correct muscular tension. This is a shift from the “only occlusion matters” point of view to a holistic approach in orthodontics.19 Another issue is adenotonsillectomy, considered by some researchers as a predictor of OSA or an indication for treating OSA.17 In the patients requiring orthognathic surgery, the improper growth pattern may have a genetic background, yet the hindered airflow in the airways could cause changes in the person’s posture, leading to muscular function disorders and being a risk factor for malocclusion in the skeletal pattern. The question is how far could the surgical approach regarding the correction of malocclusion be modified, and would it influence the dimensions of the airways that much?
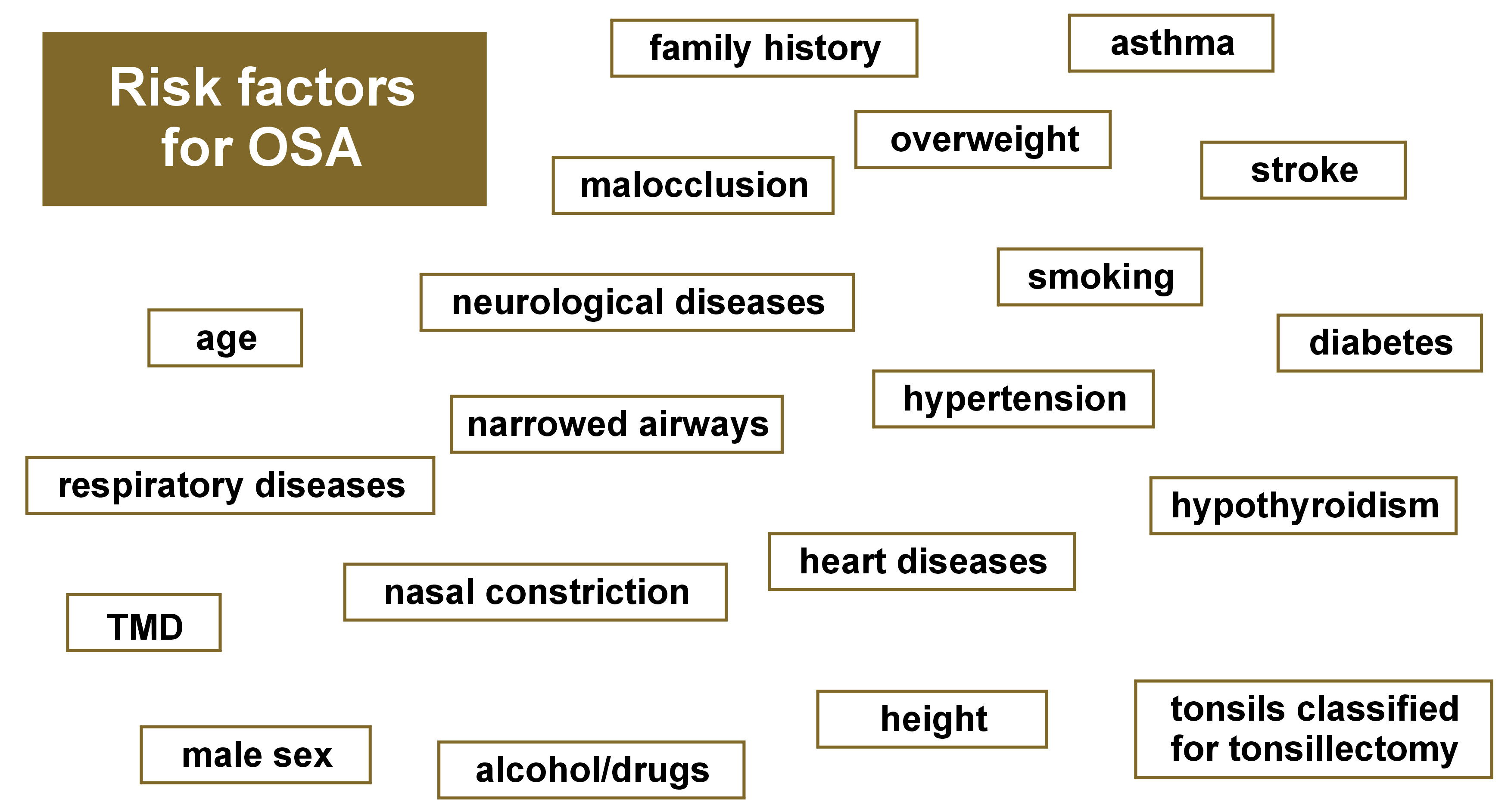
What is also problematic is the definition of the upper airways and the diagnosis of OSA. The measurement of the upper airway volume could refer to some other point, and not the height of the C3, as mentioned in the literature.16 The American Association of Orthodontists (AAO) published guidelines, according to which it is not the orthodontist who should diagnose severe breathing problems; the patient should be referred to a general practitioner, who makes diagnosis.20 Most of the published research concerning orthodontic treatment, as well as OSA, is initiated by dentists, including orthodontists, without the participation of general doctors, which could be a source of bias, with the possibly subjective conclusions drawn by orthodontists or orthognathic surgeons alone. Nevertheless, in the AAO White Paper, it is clearly stated that the orthodontist should be involved in the process of screening patients for OSA,20 as there might be a strong connection between orthodontic treatment needs and sleeping disorders, including sleep apnea.21 Even though the presented studies account for the important role of orthodontic treatment (especially when associated with orthopedic improvement, with either functional treatment or surgical advancement), the doubts still remain. The problem is that even if there is significant improvement in the airway volume, the real impact on health remains disputable. Although the airway volume measured by means of cone-beam computed tomography (CBCT) seems to be enhanced, the measured blood parameters may not confirm such improvement.21 Therefore, more studies based on polysomnography (PSG) and blood tests should be undertaken to confirm or reject the the effect of orthodontic treatment. Additionally, separate studies should be conducted with regard to functional treatment, palatal expansion and surgically associated orthodontics. This could be an interesting pathway for investigation in the nearest future. As a summary, Figure 1 collects all the most common causes of OSA.
To conclude, it is worth emphasizing that OSA should remain in the circle of physicians’ interest. The diagnostic and treatment procedures for OSA should be based on the guidelines of the American Academy of Sleep Medicine (AASM).22 Those are thought to be the most important guidelines for preventing, diagnosing and treating OSA. Investigating this condition may lead to interesting conclusions and change the perception of the problem. The questions still remain unanswered – What was first – OSA or malocclusion? Could we orthodontically modify the growth of children to avoid severe breathing problems? Is malocclusion a crucial risk factor for severe breathing problems?