Abstract
This perspective presents a new comprehensive proposal for sleep bruxism management.
Keywords: diet, lifestyle, sleep bruxism, sleep hygiene
Sleep bruxism latest definition, epidemiology and etiology
In accordance with the latest consensus, sleep bruxism (SB) is defined as a masticatory muscle activity during sleep, characterized as rhythmic (phasic) or non-rhythmic (tonic), and is not considered a movement disorder or a sleep disorder in otherwise healthy individuals.1 It is estimated to occur in up to 15% of the human adult population.2 Despite many years of research, SB still constitutes a significant diagnostic and therapeutic challenge. There are various risk factors that can contribute to SB: exogenous risk factors, such as smoking, heavy alcohol intake, caffeine, medications, or illicit drugs; psychosocial factors, including perceived stress and anxiety; sleep disorders, involving sleep arousal; and comorbidities, such as obstructive sleep apnea (OSA) and gastro-esophageal reflux disease (GERD).3 Recent research also indicates that SB may be related to the neurotransmission of the serotonin and/or dopamine pathway.4, 5 Severe SB seem to co-occur with lower serotonin blood levels, but is not correlated with the blood levels of the enzymes involved in the serotonin synthesis pathway.5 There are also studies supporting the genetic background of SB. The latest studies suggest that the polymorphisms occurring within the genes encoding dopamine and serotonin receptors may be linked with predisposition to SB and SB pathogenesis, and may contribute to the association between SB and OSA in adults.6 Similar associations with regard to the genes encoding dopamine receptors have been observed in children.7 In children, the additional factors increasing SB are the consumption of sugar, screen-time and sleeping habits.8, 9
Current management of sleep bruxism
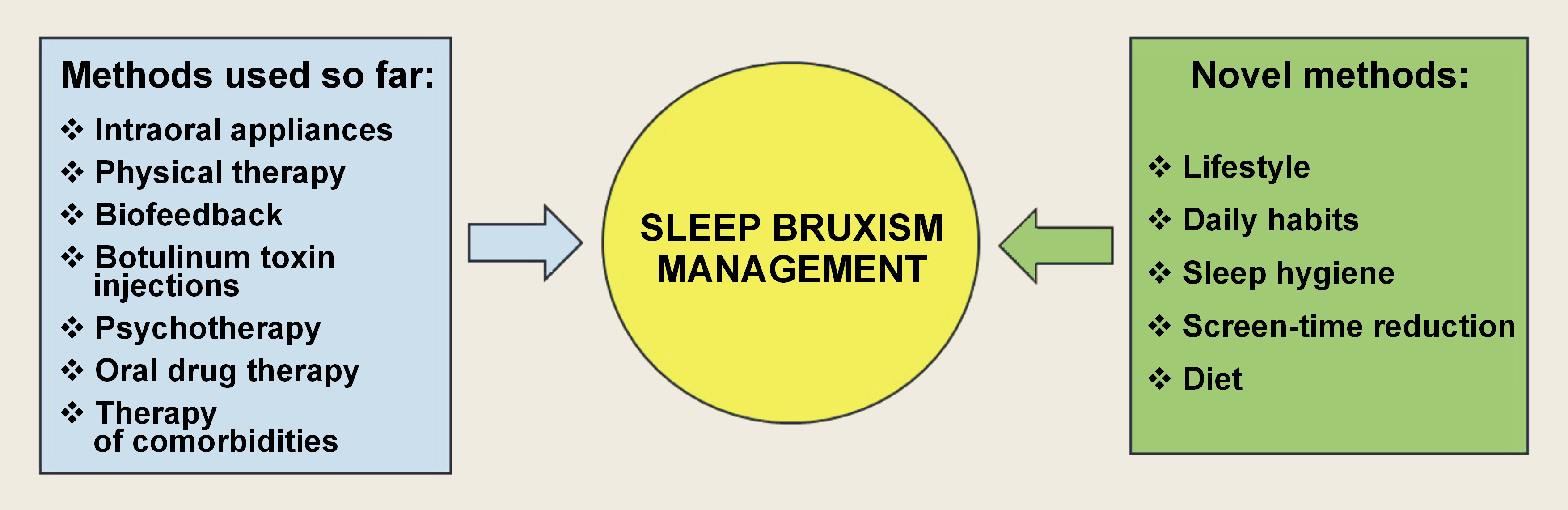
So far, the most popular methods of SB management in cases with poor health outcomes have focused on minimizing the negative effects of SB. The methods include the use of intraoral appliances, physical therapy, biofeedback, and botulinum toxin injections.1, 3, 10 Among the approaches aimed at eliminating the potential risk factors for SB, the most popular remain psychotherapy and therapies improving stress-coping strategies.1, 3 There are a few scientific reports suggesting that some drugs, e.g., opipramol, may be effective in reducing the number of SB episodes.11 The therapy of the comorbidities for which SB occurred as a protective factor (OSA, GERD) is also pointed to be important.1, 3, 10, 12 In case of OSA, management methods include continuous positive airway pressure (CPAP) and the use of a mandibular advancement device (MAD).12 With regard to the external factors influencing SB, prevention cannot be omitted.1, 3 Nevertheless, the available research is not conclusive, and does not provide clear evidence or a consensus on the most effective SB management methods.10
New approach for sleep bruxism management
Taking into account the latest research indicating the genetic basis,6, 7 the possible involvement of neurotransmission4, 5 and the importance of sleep structure9, 13 with regard to the occurrence of SB, it would be worth considering the inclusion of new methods in SB management. These methods could combine issues regarding lifestyle, daily habits, sleep hygiene, and diet, and would be based more on the elimination of risk factors than on the prevention of the negative consequences of SB.
Lifestyle, daily habits and sleep hygiene
As far as the lifestyle and daily habits are concerned, attention should be paid to 2 key elements of life that may have a significant impact on the occurrence of SB. These are psychological comfort (including stress and anxiety reduction) and sleep. A patient with SB should be aware of the harmful effects of chronic stress and poor-quality sleep. Some techniques should be used in everyday life to alleviate the symptoms of stress and improve stress-coping strategies. In recent years, much attention has been focused on everyday behaviors aimed at reducing stress. These include maintaining work–life balance, regular physical activity (especially outdoor, nature-related activities that are reported to reduce perceived stress) and breathing exercises. However, for patients who have problems with stress coping, mindfulness (including meditation) and cognitive behavioral therapy (CBT) may be recommended as well.1, 2, 3, 8, 9, 10
Sleep hygiene is also of great importance, as it significantly affects the structure and quality of sleep. Patients with SB should avoid the consumption of alcohol and coffee, smoking, and quit sugar intake at bedtime. They should also remember to limit screen-time and exposure to blue light. Convenient sleeping conditions (silence, darkness, a proper room temperature), the appropriate number of sleep hours (depending on the individual) and sleep regularity also matter.1, 2, 3, 8, 9, 10
Exposure to light greatly influences the human circadian cycle. In recent years, devices emitting blue light have emerged. Electronic devices are very popular and are used by people of all ages. Electronic devices emitting blue light cause the stimulation of the nervous system, which may lead to problems with sleep. There are scientific reports suggesting that two-hour exposure to blue light (460 nm) in the evening suppresses the secretion of melatonin.14 What is more, one-hour exposure to bright light or blue light increases the levels of stress hormones in saliva, which means that the concentration of stress hormones can be altered by the type of light people are exposed to.15 The daytime and bedtime use of electronic devices have been both reported to be related to sleep measures, with an increased risk of short sleep duration, long sleep onset latency and increased sleep deficiency.16 The use of electronic devices among children is also a rising problem. The available studies indicate that screen-time can be related to an increased frequency of bruxism in children.8 All the above-mentioned aspects suggest the need to limit the use of electronic devices emitting bright light or blue light, especially at bedtime, as part of the prevention of sleep disorders and SB.
There are also scientific reports suggesting that the dysfunction of the autonomic nervous system related to arousal during sleep is considered an underlying cause of the cardiovascular implications of SB. Sympathetic activity has been reported to increase heart rate variability, the inflammatory process, oxidative stress, endothelial remodeling, and hormonal disturbances, leading to hypertension and other cardiovascular complications. Hence, physical activity and other habits influencing the cardiovascular system could also be regarded as beneficial in patients with SB.17
Diet
Diet may also play a potential role in SB management. Apart from the limitation of the intake of substances that seem to influence the severity of SB (caffeine, excess sugar, narcotics, some medications), patients should also consider the consumption of substances that have a beneficial effect on the functioning of the nervous and muscular systems, stress reduction and sleep improvement. These include microelements, such as magnesium (Mg), calcium (Ca), potassium (K), zinc (Zn), and iron (Fe). Vitamins used in SB management include B vitamins, essential for the functioning of the nervous system, and vitamin D, influencing sleep and preventing sleep disturbances. Some authors also indicate the importance of omega-3 fatty acids, which support the overall health of the nervous system.1, 18, 19 Moreover, in light of the latest research, it is worth noting that due to the reported role of neurotransmission, especially the neurotransmission related to the serotonin pathway, the diet of SB patients should be pro-serotonin, i.e., rich in tryptophan.4, 5 Such diet contains products rich in carbohydrates and protein, like fish, bananas, seeds, avocado, or eggs. There are also scientific reports that underscore the influence of dietary fiber consumption on SB. One of the studies showed that students with SB had a significantly lower dietary fiber intake than those without SB.20
Highlights
Sleep bruxism still constitutes a major diagnostic and therapeutic challenge due to its complicated and not fully understood characteristics. This creates the need to constantly search for new therapeutic paths. Nowadays, apart from the standard methods previously used to manage bruxism, more attention should be paid to aspects related to lifestyle, daily habits, sleep hygiene, and diet (Figure 1).