Abstract
Symmetry is present in various aspects of everyday life. A symmetrical face is considered attractive, whereas a lack of facial symmetry is regarded as a source of functional and aesthetic problems. Most of the people exhibit slight asymmetries, but some of them reveal severe asymmetries. Among patients presenting with severe facial asymmetries, there may be those with congenital defects. Congenital defects may manifest at the time of birth or be a result of birth trauma.
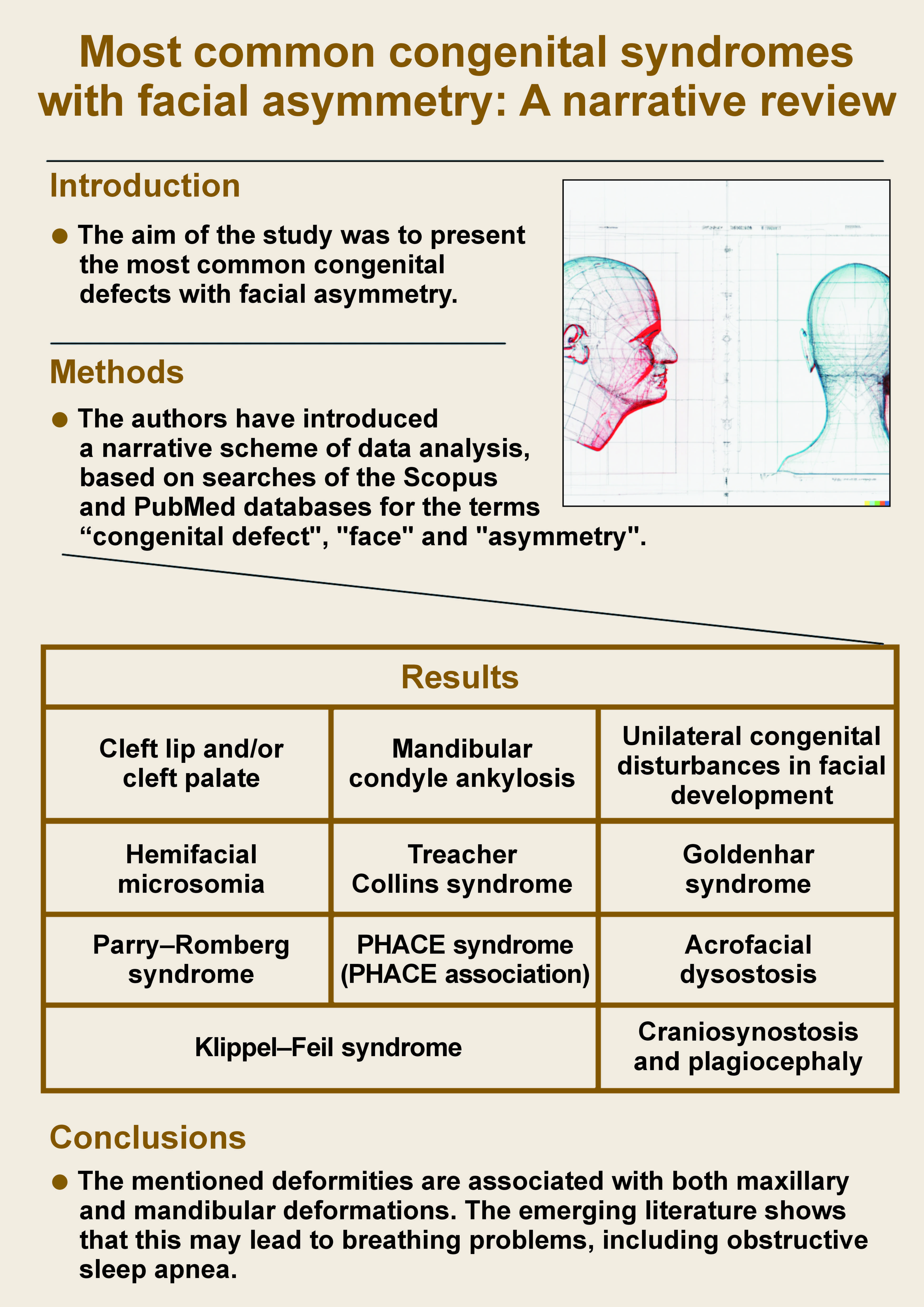
One of the most prevalent asymmetrical birth defects is cleft lip and/or cleft palate. Other congenital defects include craniofacial syndromes, such as Treacher Collins syndrome (TCS) and Goldenhar syndrome. Among the rare syndromes with facial asymmetries, Klippel–Feil syndrome (KFS), PHACE (posterior fossa brain malformation, hemangiomas, arterial anomalies, cardiac anomalies, and eye abnormalities) syndrome, plagiocephaly, and Parry–Romberg syndrome are worth noticing. The majority of craniofacial asymmetries require surgery to improve the patient’s facial appearance. The treatment is multidisciplinary and long, and the most common procedures involve reparative and regenerative surgeries. The aim of this review was to present the most common congenital defects with facial asymmetry.
Keywords: congenital abnormalities, cleft lip, facial asymmetry, cleft palate, PHACE syndrome
Introduction
Symmetry is a factor that influences our perception of beauty. It is present in various aspects of everyday life, including architecture and art. Symmetry is often equated with elegance.1 An aesthetic smile is considered more attractive,2 and the attractiveness of a smile is one of the key factors influencing the cooperation during the orthodontic and aesthetic dental treatments.3 Teeth size and gingival margin symmetry contribute to the perceived attractiveness of a smile.4 A symmetrical face is recognized as attractive, and a lack of symmetry may cause facial and functional problems.5 Craniofacial asymmetry is a normal condition, especially when compared to orthodontic diagnosis. Asymmetries have a strong genetic background, as demonstrated by Babczyńska et al.6 Additionally, this topic has been described in the context of other dental specialties.7 Based on the analysis of the patients treated orthodontically in North Carolina, 74% of cases were observed in the lower third of the face, 36% in the middle part, and the least asymmetries (5%) were observed in the upper part of the face.8 According to Kozanecka et al.,9 bite asymmetries (including crossbites) are one of the most common causes for good patient cooperation during the orthodontic treatment, which supports the thesis that facial aesthetics is a crucial factor in this process. It is also worth mentioning that males tend to assess dental asymmetries with greater precision than females.2
However, there are certain conditions that are not caused by malocclusions but rather are the result of congenital syndromes. These conditions usually have a genetic background.10 Nowadays, the use of distractors in the treatment of facial asymmetries is becoming increasingly popular. It may facilitate the treatment of asymmetries in hemifacial underdevelopment by elongating the mandible or rotating it in the gonial angle.11 The main causes of facial asymmetry are congenital disorders and developmental deformities.5
The aim of this study was to present the most common birth defects associated with facial asymmetry and congenital diseases. This paper collates the most important data on prevalent congenital syndromes that are characterized by craniofacial asymmetry. Such conditions may manifest at the time of birth or be a result of birth trauma. The article presents recently collected data on congenital syndromes that have not been previously summarized.
Material and methods
For the purpose of this paper, the Scopus and PubMed databases were searched. The terms “congenital defect”, “face” and “asymmetry” were used to determine the most common defects affecting the orofacial area. The study included articles from the last 10 years, as general knowledge about rare congenital diseases is increasing. The majority of the papers focused on cleft lip and cleft palate. Therefore, we incorporated this anomaly into the research. However, we excluded it from the search criteria to identify other articles about the facial asymmetry.
Cleft lip and/or cleft palate
Cleft lip and cleft palate are the most common congenital anomalies, occurring in 1:700–1:1,000 patients. The non-syndromic cleft occurs in the 5th–12th week in utero. It is usually a multifactorial condition, with a genetic background identified in approx. 20% of cases.12 The lips and the nose (especially the philtrum, columella and the vermilion border of the upper lip) are the most asymmetrical regions. This condition is more prevalent before the surgical procedure of closing the cleft lip and improves after surgery. Unfortunately, growth is unfavorable in this case, resulting in pronounced facial assymetry as the scar on the clefted side develops.13 The asymmetry is also more pronounced when a total cleft is present, when compared to an isolated cleft lip.14 Patients with clefts present with asymmetry not only in the face but also in the occlusion and dental arch form. Asymmetry of the dental arch is observed in all cases. Malocclusions are also asymmetrical, as crossbites are the most common conditions in cleft patients.15, 16 Hereditary dental anomalies, such as hypodontia, hyperdontia or tooth impaction, are also common and occur more frequently in cleft patients than in the general population.17 Cleft deformities have a strong genetic background. The genetic pattern is based on multiple genes and is strongly influenced by environmental factors, which makes this problem even more difficult to diagnose.18
Patients with clefts require a multidisciplinary approach that should be initiated at the neonatal period.19 The approach depends on the type of cleft and the individual treatment needs. The procedures focus on the reconstruction and plastic surgery, but other aspects like speech therapy and orthodontic treatment are also very important. The most common procedures performed in patients with clefts are presented in Table 1.
The first procedures performed in patients with clefts concentrate on the presurgical preparation of the patient for lip and/or palate closure. The procedures involve a lip massage to lengthen soft tissues and reduce the pressure of the prospective scar. All presurgical actions are aimed at reducing the stigma associated with cleft lip and cleft palate. To reduce columella and mold the palate, nasoalveolar molding (NAM) plates, introduced by Grayson and Maull, can be used.18, 20 The NAM plate rotates the premaxilla and, therefore, reduces the cleft of the alveolus.
The first surgical procedure concerns the lip and/or palate closure, which is typically performed between the 3rd and 6th month of age.21 The soft tissues are restored, but the fissure in the bone requires filling. This is achieved through bone grafting, which is most frequently derived from the iliac crest.22 The palate of the operated patient is shortened and has lower mobility. A number of procedures can be performed to restore the palate to its normal length. Of these, Furlow palatoplasty is the most commonly performed procedure. It is a simple Z-plasty surgery, in which the soft tissues are mobilized to lengthen the palate. The purpose of this procedure is to seal the oral cavity and prevent oronasal communication. Furlow palatoplasty is usually performed between the ages of 8 and 12 years.23
During the entire treatment period, the patient requires orthodontic care. The presence of soft tissue scars results in a repetitive narrowing of the arch. It is necessary to widen the upper arch of the patient, which may be achieved through the use of removable or fixed appliances. A face mask is worn for maxillary protraction. As the majority of patients present with crossbites and maxillary hypoplasia, it is important to determine whether the patient would benefit from orthognathic surgery in adulthood.14, 18
Mandibular condyle ankylosis
Temporomandibular joint ankylosis is defined as a permanent constriction of the jaws and a limited mouth opening to a maximum of 30 mm (measured between the incisal edges). Due to the limited mandibular movement, the ability to chew, speak and swallow may be impaired.24 Mandibular condyle ankylosis may result from injury at birth or complications during labor (17.8%). Temporomandibular joint ankylosis is a dangerous condition in children, as it may lead to facial asymmetry. This condition is mostly caused by trauma during the childhood (48.9%).25 If left untreated, the ankylosis in a child will result in facial widening and crossbites. Additionally, severe class II and skeletal open bite may result from the impairment of potential growth caused by the growth cone on the mandibular head. This can lead to disturbances in both mandibular length and ramal height.26, 27 The limited mouth opening is comparable to that observed in rheumatoid arthritis and may impede proper oral hygiene, increasing the risk of caries and periodontal disease.28, 29 In addition to limiting mandibular movement, this condition does not influence muscular tonus and function.30 To reduce the presented consequences of mandibular condyle fractures, early rehabilitation is essential.30 Prompt management of mandibular fractures plays a key role in reducing growth disturbances in mandibular dimension and morphology.25, 26
Unilateral congenital disturbances in facial development
Several disturbances in facial development are observed, and in the majority of cases, these are asymmetrical. The most common unilateral congenital anomalies affecting the face include hemifacial microsomia, Treacher Collins syndrome (TCS) and Goldenhar syndrome. These anomalies pertain to malformations of the 1st and 2nd pharyngeal arches.31, 32 Most of the symptoms manifest in the face and dental region. A common issue is the potential for a dentigerous cyst, which may cause disturbances in tooth eruption. The typical treatment for this condition is marsupialization or the extraction of the affected tooth.33
Hemifacial microsomia
Craniofacial microsomia (CFM) appears in 1:3,500 to 1:5,600 live births, which situates this malformation as the 3rd most common congenital craniofacial anomaly, preceded by cleft lip, cleft palate and craniosynostosis. Patients with CFM present with asymmetries in mandibular body and ramal lengths. This leads to the retrusion of the mandible. In addition, hypoplasia of the ear occurs in 66–99% of the individuals.34 The full etiology of this condition remains unclear, but it manifests during embryonic development. The possible models for this condition include vascular abnormalities, hemorrhage or neurocristopathy among the nasal placode and the 1st and 2nd pharyngeal arches.35, 36 In rare instances, bilateral microsomia is observed, which is symmetrical (present in 5–15% of cases).34 There is no specific diagnostic criterion for microstomia. However, most of the patients present with the underdevelopment of half of the face, specifically the mandible, maxilla, facial soft tissues, ear, orbit and/or facial nerve. This might influence facial movements, food intake, breathing, and disrupt hearing. The facial appearance is interrupted and easily noticeable.32 The treatment requires bone and soft tissue reconstruction, as well as the correction of auricular anomalies.37 Despite extensive knowledge of the genetic basis of CFM, the definitive genetic background of this anomaly remains unclear.38
Treacher Collins syndrome
Treacher Collins syndrome, also known as Franceschetti syndrome or mandibulofacial dysostosis, is a genetically driven condition caused by abnormal differentiation of the 1st and 2nd pharyngeal arches. The deformity is observed in 1 in 50,000 live births with a strong hereditary background, with 40% of cases having a family history. Genetically, 4 variants of mutations within genes have been observed: TCOF1; POLR1D; POLR1C; and POLR1B.39 It is probably the first and the most studied cranial neural crest anomaly.40
The facial features of TCS include hypoplasia of bones such as midface hypoplasia, microtia and hemifacial micrognathia. The other characteristics are conductive hearing loss and slanting palpebral fissures with the possibility of coloboma of the lateral part of the lower eyelid. On occasion, cardiovascular problems associated with cleft palate, esophageal and/or choanal atresia or stenosis are observed. Due to the severe craniofacial malformation and retruded mandible, nocturnal apnea may be observed, which could potentially be a life-threatening situation.39, 41 Additionally, the hairline is displaced.40 In individuals with TCS, clockwise rotation of the mandible may result in an open bite and class II malocclusion, which may subsequently lead to temporomandibular joint disorders.42 On cephalometric X-rays, a shortening of the posterior and anterior cranial bases can be observed.43 Due to the hearing problems, most patients present with speech issues. Other senses are also affected, including impaired sight and feeding.39, 41 Due to the severe craniofacial malformations, patients require surgical and reconstructive treatment. These procedures involve soft and hard tissues, especially the orbit zygomatic and maxillary regions.39, 41 The malformations result in poor oral hygiene in individuals with TCS, increasing the risk of calculus and caries.42
Goldenhar syndrome
Goldenhar syndrome, also known as ocular-auricular-vertebral (OAV) syndrome, is a congenital condition resulting from a defect in the 1st and 2nd brachial arches. This anomaly is caused by a combination of genetic and environmental factors.44, 45 Lately, a candidate gene on the 22q chromosome has been found to play a crucial role in OAV syndrome.46 Facial asymmetry, ear-eye abnormalities, congenital problems, vertebral anomalies, and severe obstructive sleep apnea and sialorrhea are typical manifestations of Goldenhar syndrome.44 The clinical presentation of the condition may vary, from slight facial asymmetry to severe craniofacial deformities. There are no minimum inclusion criteria defined.45, 47 In 100% of cases, hemifacial hypotrophy is observed. Auricular anomalies are observed in 80% of individuals. In 90% of cases, there is unilateral ophthalmic involvement, with upper eyelid coloboma (75.76%), lipodermoid (54.55%) and limbal dermoid (30.3%) being the most common.48 Individuals with Goldenhar syndrome often require surgical procedures, such as the repair of eyelid colobomas.48 The potential vertebral anomalies and the limitations of head and neck movement present a challenge to the successful performance of laryngoscopy and intubation.49
Acrofacial dysostosis
Miller syndrome and Nager syndrome are the most common acrofacial dysostoses.50 Nager syndrome is very similar to TCS and may be misdiagnosed. The syndrome manifests with preaxial limb defects, hypoplasia or the absence of the thumbs. Additionally, recent studies found mutations in the SF3B4 gene in approx. 60% of cases.50, 51, 52 Hearing loss, present in 45% of cases, is probably caused by defective middle ear ossicles.53
Another syndrome that belongs to this group of malformations is Miller syndrome. It is also referred to as post-acrofacial dysostosis (POADS), Wildervanck–Smith syndrome or Genée–Wiedemann syndrome. The presence of downward slanting of palpebral fissures, hypoplasia of the zygomatic complex, coloboma of the lower eyelid, microtia and micrognathia as well as hearing loss, presents a significant challenge in differentiating POADS from TCS. It was determined that the condition is caused by autosomal recessive or heterozygous mutations in dihydroorotate dehydrogenase (DHODH).50, 51 The gene encodes the enzyme in the pyrimidine de novo biosynthesis pathway. It has been identified in the mitochondrial intermembrane space.54
The differentiation of these syndromes may be challenging. In order to organize the data and features concerning the 4 clinical units, a summary of the facial features of the previously described congenital disorders is presented in Table 2.
PHACE syndrome (PHACE association)
PHACE syndrome is a rare congenital condition, occurring in less than 1 in 1,000,000 cases, that is characterized by the presence of large facial hemangiomas (sometimes also of head and neck) and other systemic malformations. The acronym stands for the association of the following syndromes: posterior fossa brain malformation; hemangiomas; arterial anomalies; cardiac anomalies; and eye abnormalities. In most cases, hemangiomas can be successfully treated with oral propranolol. Large infantile hemangioma is often correlated with malformations of the posterior cranial fossa. Additionally, midline or ventral anomalies are a common feature. Cerebrovascular involvement is present in 80% of cases. Other anomalies do not refer to the face and are instead associated with anomalies of the central nervous system, cardiac defects, endocrine problems (e.g., thyroid dysgenesis), coarctation of the aorta, and ocular abnormalities.55, 56, 57 The etiology of PHACE is not fully understood. It has been observed that PHACE syndrome is more frequently observed among females.58
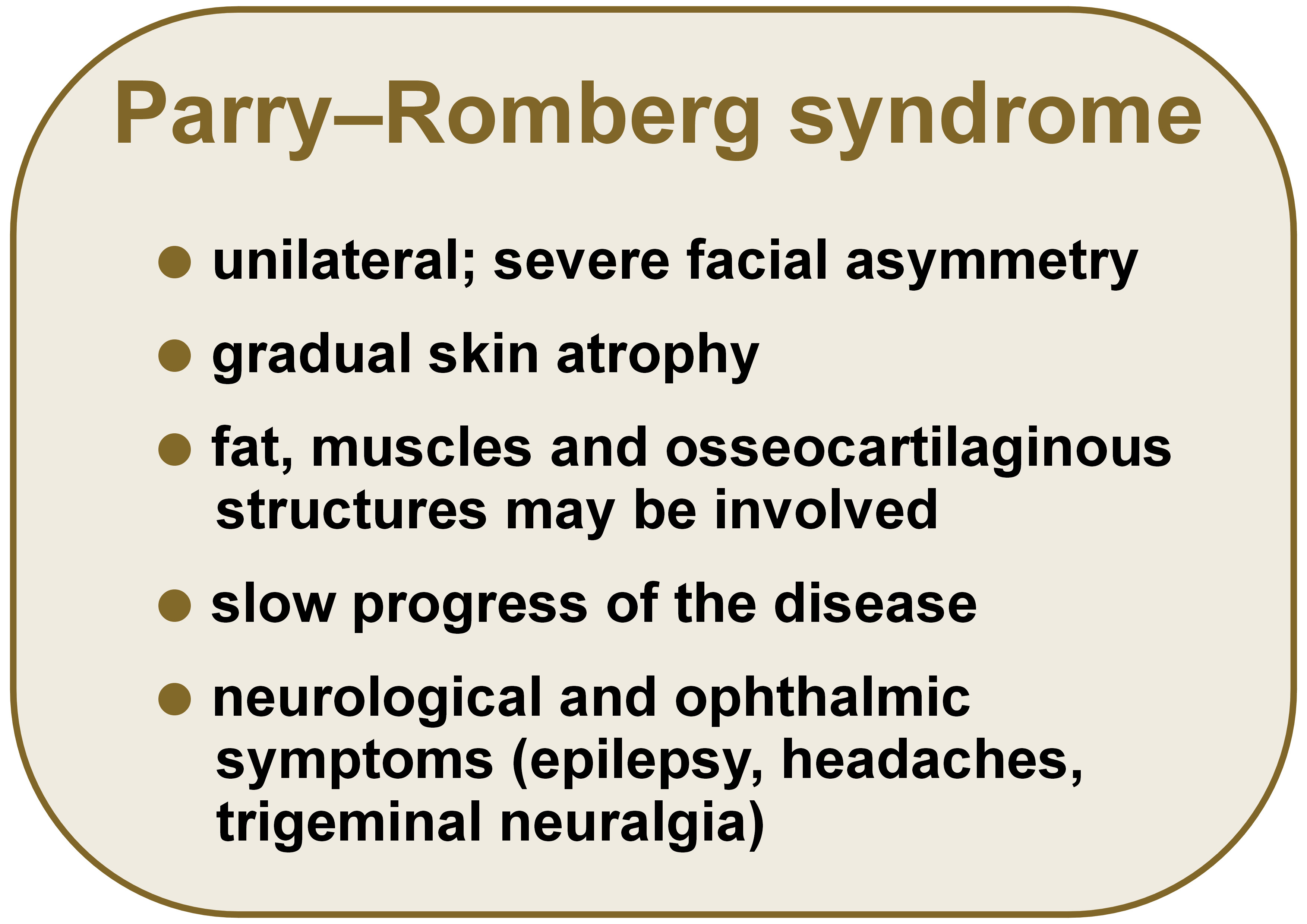
Parry–Romberg syndrome
Parry–Romberg syndrome is a rare condition that is characterized by progressive hemifacial atrophy. The etiology of the disorder remains unknown. The characteristic feature is the unilateral, gradual atrophy of the skin. The process may involve the underlying tissues, including fat, muscles and osseocartilaginous structures. This results in a severe facial asymmetry.59 The syndrome typically affects patients under the age of 20 years, with a higher prevalence among females. The younger the patient, the more severe the course of the symptoms.60 In more severe cases, the neck and the other half of the face may also be involved.61 The most common features of Parry–Romberg syndrome are presented in Figure 1.
The progress of the disease is rather slow, but it frequently becomes complicated by the involvement of other systems (e.g., neurological, ophthalmic).60 The most common neurological complications, such as epilepsy, headaches and trigeminal neuralgia, are described.61
Following the stabilization of the disease, the reconstruction of lost tissues is performed to restore facial asymmetry. Fat grafting is usually a method of choice. It shows favorable results when the reconstruction requires mild to moderate soft tissue deficiency. In more severe cases, free tissue transfers are necessary.59 When complicated with melasma, skin bleaching is also indicated for aesthetic reasons.62
Craniosynostosis and plagiocephaly
Craniosynostosis is a condition that involves premature fusion of skull sutures.63 It is typically an isolated condition, but in some cases it may be a feature of specific syndromes, such as Apert syndrome or Crouzon syndrome. In most cases, treatment is necessary to reduce the likelihood of developmental delay and other neurological complications, as well as abnormalities within the skull (e.g., facial, sensory, respiratory).64 It is important to differentiate this condition from positional plagiocephaly, which is caused by an improper position of the fetus rather than the premature suture closure. It may be caused by injuries during birth, pregnancy and prematurity.65 Craniosynostosial plagiocephaly has an influence on a child’s development, and if not diagnosed promptly, may result in mental retardation.66
The term “plagiocephaly” is derived from Ancient Greek, where “plagios” means “oblique” and “kephalē” signifies “head”. The typical presentation is asymmetry of the head due to unilateral flattening. Plagiocephaly is classified as a non-syndromic craniosynostosis, occurring at one of the sutures, specifically the coronal or lambdoid. It causes head and face asymmetry. When premature fusion concerns the coronal suture, the asymmetry manifests in the anterior region of the skull. Premature fusion of the lambdoid suture leads to posterior synostosis.63 In cases of positional plagiocephaly, a conservative approach involving the use of a special helmet is recommended. If the condition is the result of premature suture closure, surgical procedure is the preferred method of treatment.65
Klippel–Feil syndrome
The defining characteristics of Klippel–Feil syndrome (KFS) arise from the fusion of cerebral vertebrae, most frequently C2 and C3 (more rarely, C5 and C6). In some cases, additional vertebrae are involved. Due to this condition, the neck is shortened and restricted in its mobility. Individuals with KFS also present with a low posterior hairline.67 The latest report considered a possible fusion of C1 and C2 vertebrae, which results in limitations in head rotation.68 Facial asymmetry is observed on the side of torticollis. The syndrome occurs with a prevalence of 1:42,000 births, and most of the cases concern females (60%).69 The observed torticollis may “hide” the shortening of the neck.70 The real prevalence is not known, although genetic factors (homeobox genes and differentiation factors, such as MEOX1, GDF6 and GDF3) appear to play a crucial role in this syndrome.69 Due to the severity of cervical vertebral fusion, Gunderson et al. divides KFS into 3 types: type I – fusion of multiple vertebrae, including the thoracic vertebrae; type II – fusion of 2 or 3 vertebrae; type III – fusion of both the cervical and lower thoracic or lumbar vertebrae.48, 71 Most of the patients receive non-surgical treatment. Only cases with severe neurological complications require surgical intervention.72, 73
Conclusions
This study presents an overview of the most common congenital deformities characteristic of facial asymmetry, providing a summary of their most frequent features. Interestingly, the abovementioned deformities are associated with both maxillary and mandibular deformations. The emerging literature shows that this may lead to breathing problems, including obstructive sleep apnea.74, 75, 76, 77 This represents a potential area for future research, as, to the best of our knowledge, there is no existing data on this topic. It would be interesting to consider the potential benefits of splint therapy. This influences the position of the mandible and, in most cases, increases the volume of the airways.78, 79 One must, however, take into account that the properties of the materials used for splint preparation change with time, and the problems with durability and general structure may occur due to material aging and the influence of saliva.80 Furthermore, teledentistry has emerged as a novel trend, especially during the coronavirus disease 2019 (COVID-19) pandemic.81 Although teledentistry may offer certain advantages, the cooperation with a dental practitioner remains the most important aspect, given the necessity for precise diagnostic tools for the intraoral examination. In such cases, the appropriate treatment can be administered.81, 82, 83
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.