Abstract
Background. The inferior alveolar canal (IAC) is a fundamental mandibular structure. It is important to conduct a precise pre-surgical evaluation of the IAC to prevent complications. Recently, the use of artificial intelligence (AI) has demonstrated potential as a valuable tool for dentists, particularly in the field of oral and maxillofacial radiology.
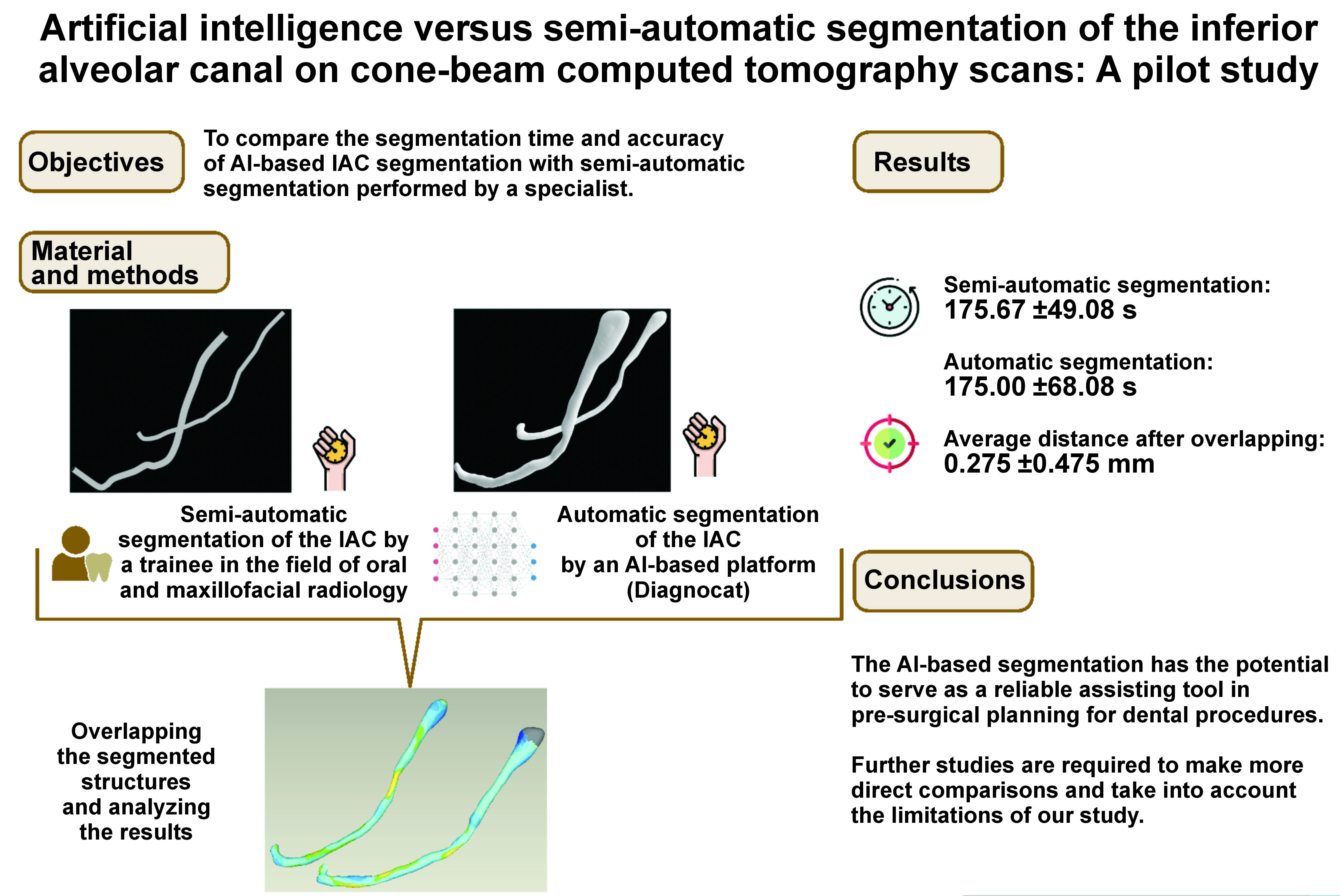
Objectives. The aim of the study was to compare the segmentation time and accuracy of AI-based IAC segmentation with semi-automatic segmentation performed by a specialist.
Material and methods. Thirty individual IACs from 15 anonymized cone-beam computed tomography (CBCT) scans of patients with at least 1 lower third molar were collected from the database of Poznan University of Medical Sciences, Poland. The IACs were segmented by a trainee in the field of oral and maxillofacial radiology using a semi-automatic method and automatically by an AI-based platform (Diagnocat). The resulting segmentations were overlapped with the use of Geomagic Studio, reverse engineering software, and then subjected to a statistical analysis.
Results. The AI-based segmentation closely matched the semi-automatic method, with an average deviation of 0.275 ±0.475 mm between the overlapped segmentations. The mean segmentation time for the AI-based method (175.00 s) was similar to that of the semi-automatic method (175.67 s).
Conclusions. The results of the study indicate that AI-based tools may offer a reliable approach for the segmentation of the IAC in the context of dental pre-surgical planning. However, further comprehensive studies are required to compare the methods and consider their limitations more comprehensively.
Keywords: accuracy, diagnosis, artificial intelligence, segmentation, inferior alveolar canal
Introduction
The inferior alveolar canal (IAC), also known as the mandibular canal, is a bony structure within the internal border of the mandible that carries the inferior alveolar nerve (IAN), artery and vein.1, 2 The IAN is responsible for providing sensory innervation to the lower lip, mandibular teeth, chin, lower gingiva, and buccal mucosa, as well as motor innervation to the jaw muscles, enabling movement.3, 4 Damage to the IAC can result in numbness and paresthesia in the affected areas.5 Therefore, it is essential to conduct an accurate pre-surgical evaluation of the IAC based on the specific procedure being performed. Such procedures include implant placement, extraction of third molars, root canal treatment, and orthognathic surgery, among others.6, 7, 8, 9 This evaluation is typically conducted through radiographic image analysis, such as two-dimensional (2D) panoramic X-rays or three-dimensional (3D) X-rays, to prevent complications.
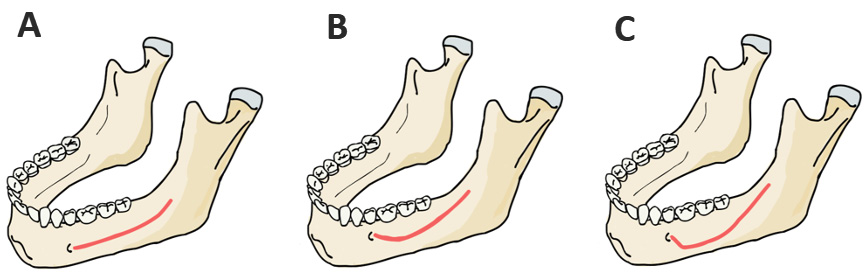
Cone-beam computed tomography (CBCT) is a commonly used imaging technique in dentistry that generates images using a fan-shaped beam of X-rays.10 Cone-beam computed tomography produces high-resolution images that can be reconstructed into a 3D image, rendering it a valuable tool for evaluating facial anatomy, including the IAC and its variations.11, 12, 13 Ozturk et al. identified 3 distinct configurations for the IAC within the mandible (Figure 1).14
The term “artificial intelligence” (AI) is used to describe the ability of computer systems and other machines to simulate human cognitive functions, including decision-making, problem-solving and visual perception.15, 16 In recent years, AI has been increasingly adopted in the field of dentistry, reflecting a transition toward the 4th industrial revolution, also known as Industry 4.0.17 This term refers to the integration of modern technologies, such as AI, robotics and the Internet of things (IoT), into various sectors.17, 18
Machine learning (ML) algorithms are a type of AI that enables computer systems to enhance their performance on a specific task through experience.19 Deep learning (DL) is a form of ML that is particularly useful for tasks that require processing large amounts of data and extracting complex patterns and features.19 The accuracy of AI, including DL algorithms, in performing automatic segmentation of the IAC has been evaluated in previous studies.20 However, to the best of our knowledge, none of these studies have compared the segmentation time of AI-based segmentation to semi-automatic segmentation. Furthermore, the methodologies used in these studies differed from those employed in our research. Our retrospective pilot study aims to address this gap by comparing the segmentation time and accuracy of AI-based IAC segmentation with semi-automatic segmentation performed by a specialist.
Material and methods
Image dataset
Fifteen anonymized CBCT images, performed for the purposes of implant planning and third molar extractions, were obtained from the database of Poznan University of Medical Sciences, Poland. The scans were selected in accordance with the established inclusion criteria (Table 1). Each of the scans included both the right and left canals, allowing for a total of 30 IACs to be retrospectively analyzed. The CBCT images were registered during the years 2020 and 2021 using dental imaging system (CRANEX® 3D; Soredex, Milwaukee, USA) and stored in the DICOM (Digital Imaging and Communications in Medicine) file format. The CBCT images were taken using the following settings: an X-ray tube voltage of 90 kV; an X-ray tube current of 10 mA; a voxel size of 0.25 mm; and a field of view (FOV) ranging from 600 mm × 800 mm to 1,600 mm × 1,300 mm.
Semi-automatic segmentation
The IAC tracing, integrated into the Romexis® software, v. 6.2 (Planmeca, Helsinki, Finland), was employed to perform the semi-automatic segmentation (ground truth method) of the IAC on cross-sectional views of the 15 images collected. The tool requires the user to designate points along the canal, with the software automatically computing the canal’s pathway through progressive extension from these designated points. The task was performed by a trainee in oral and maxillofacial radiology (JI). During the segmentation process, the diameter of the cylinder representing the nerve replica was set at 1.50 mm. Subsequently, the IACs on both sides were saved as a single STL (Standard Triangle Language) file (Figure 2). The time required to complete the segmentation was recorded from the commencement of the process to its conclusion.
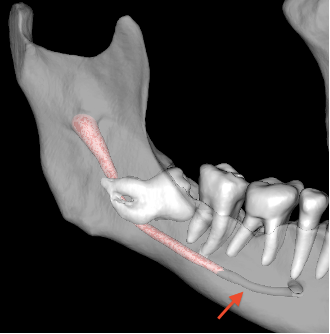
Automatic segmentation
Artificial intelligence was used to perform the automatic tracing of the IAC in the same anonymized images that had been previously segmented semi-automatically. The images were uploaded to Diagnocat (DGNCT LLC, Miami, USA), an online AI-based platform designed for the storage and processing of dental images based on a U-Net-like architecture algorithm. The AI algorithm automatically generated the IAC tracing and saved it as an STL file (Figure 3). The time required to complete the process was recorded, with an average Internet speed of 290 Mbps.
Evaluation of the 3D models obtained from 2 segmentation methods
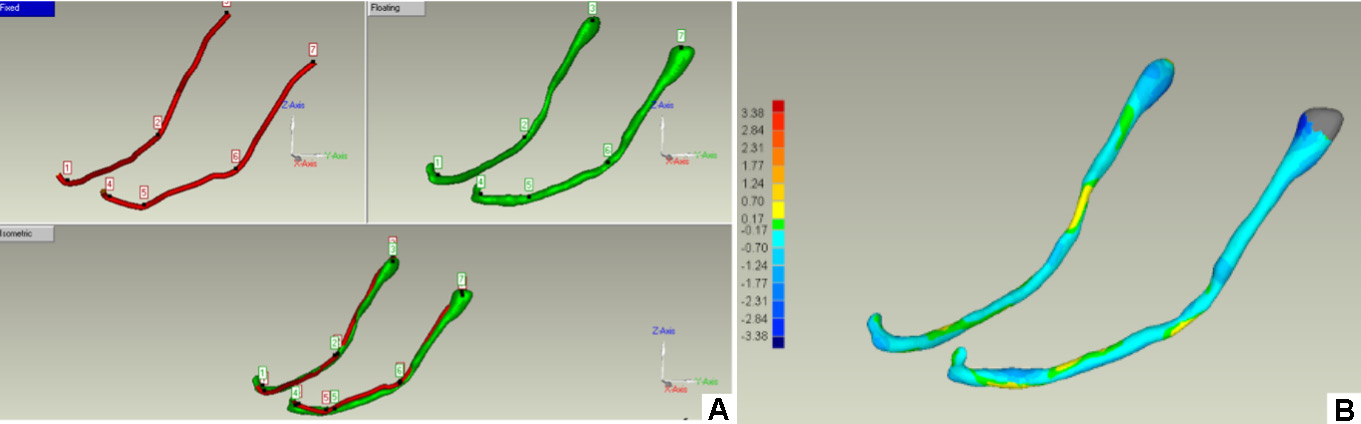
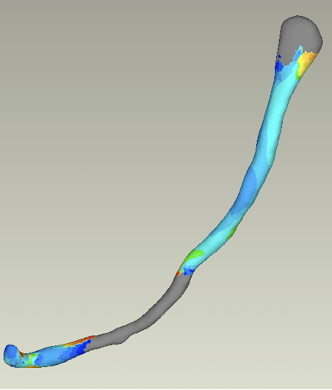
Following the completion of the segmentation process using both methods, the STL files were exported to Geomagic Studio (3D Systems, Morrisville, USA). The software was used to overlap the segmented IAC produced by both methods onto the same image (3D registration), facilitating a 3D visualization for the purpose of evaluating the accuracy of the AI model in comparison to the semi-automatic method (Figure 4).
As a first step, a pre-registration was conducted using the 3-point method to ensure accurate orientation of the models in relation to one another within the 3D space. This step was performed by an experienced Geomagic Studio user (MR). In the second step, the automatic registration procedure was initiated (Figure 4A).
The software uses 100 iterations to calculate and minimize the mean square error of the global distance between the surfaces of the overlapping structures without requiring input from an operator. To compare the surface results of the 3D models, the 3D Compare command in Geomagic Control software (Geomagic Studio; 3D Systems) was used, which generated numerical results, including volumetric deviation and average distance, as well as a color map with 15 segments, each representing a different level of volumetric deviation. The average distance was then compared for the purpose of visualizing and assessing the deviation in the individual IAC areas of the 3D models (Figure 4B).
Statistical analysis
The statistical analysis was conducted using the IBM SPSS Statistics for Windows software, v. 29.0 (IBM Corp., Armonk, USA). The numerical results of the 3D evaluation were subjected to a descriptive statistical analysis and summarized using mean and standard deviation (M ±SD). The normality of the numerical variables was evaluated using the Shapiro–Wilk test, with a significance level of p < 0.05. Subsequently, an inferential statistical analysis was performed using the non-parametric Mann–Whitney U test for numerical variables with a non-normal distribution. All inferential tests were conducted in accordance with the assumptions of a 95% confidence interval (CI) and a p-value of less than 0.05.
Results
The results of the overlap analysis between the semi-automatic and automatic segmentation methods, in terms of average distance, are shown in Table 2. These values were calculated for each side (left and right) of the included patients. The mean value of the average distance across all patients was found to be 0.275 ±0.475 mm.
The segmentation time was recorded for both methods and subjected to the Mann–Whitney U test for comparison. The recorded times for the semi-automatic and automatic segmentation methods were 175.67 ±49.08 s and 175.00 ±68.08 s, respectively. The Mann–Whitney U test demonstrated that the difference in time between the 2 methods was not statistically significant (p = 0.389).
Discussion
Imaging techniques such as CBCT have significantly improved the ability to detect and segment the IAC.21 Accurate detection of the IAC is vital in pre-surgical planning for dental procedures to prevent injury, particularly in view of the diverse variations that may be encountered.22, 23 However, semi-automatic detection of the IAC in CBCT images can be time-consuming and prone to human error.
Recently, there has been a growing trend in using and developing automated algorithms for the detection of the IAC in CBCT images.20 These algorithms employ ML techniques, such as DL, to analyze the images and accurately locate the IAC. Artificial intelligence has the potential to markedly enhance the efficiency and precision of pre-surgical planning for dental procedures, reducing the risk of nerve injury. Additionally, AI has the potential to significantly increase the speed and efficiency of tasks such as image analysis, as well as assist in diagnosis.24, 25 The automation of repetitive and time-consuming tasks by AI enables medical professionals to prioritize direct patient care, ultimately improving patient outcomes.24, 25 This research compares the AI-based IAC segmentation performed by Diagnocat (DGNCT LLC) with the semi-automatic segmentation performed by a specialist in terms of segmentation time and accuracy.
The average distance, representing the level of deviation between the points on the surface of the overlapped structures, was used in order to evaluate the accuracy of IAC segmentation performed by both methods. The average distance is a recommended metric for assessing non-regular complex shapes and quantitatively evaluating overlapping structures.26, 27, 28 The results obtained from comparing the average distance of the overlapped semi-automatic segmentation and Diagnocat segmentation of the 30 IACs present the value of 0.275 ±0.475 mm. In contrast to a study conducted by Jaskari et al., our research yielded superior outcomes, with an average symmetric surface distance of 0.45 mm for both canals (with a SD of 0.12 mm for the left canal and 0.11 mm for the right canal).29 These results suggest that the segmentation generated by Diagnocat is highly accurate, approaching the precision of the semi-automatic segmentation performed by an operator. A lower average distance indicates greater similarity in shape and volume between the 2 structures, and a higher accuracy of the automatic segmentation.
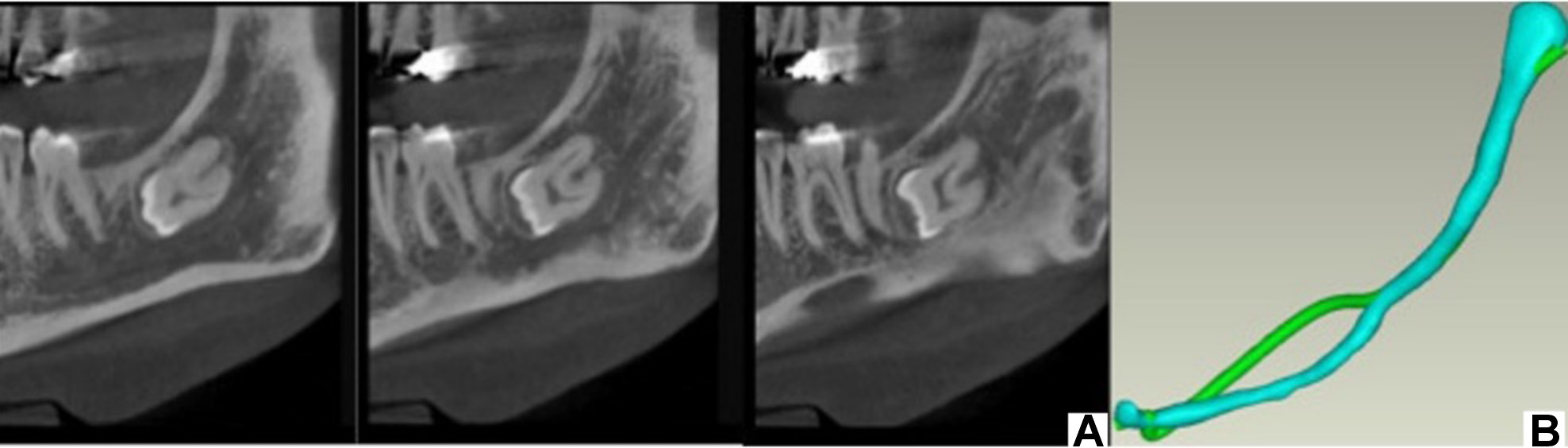
A variety of methodologies exist for medical image segmentation. Some involve user interaction for support, a process known as energy minimization. Others utilize DL, which enhances accuracy by comparing its predictions with real data.30 However, the second method encounters challenges with including user feedback and potential corrections in the process.30 Upon investigating the reasons behind the average distance differences observed in certain cases, we observed that Diagnocat tends to segment the IAC along the radiolucent path, following a straight pattern. However, in practice, some discrepancies were noted (Figure 5).
The results of the segmentation time analysis indicate that the semi-automatic and automatic segmentation methods require a similar amount of time. The mean time for the semi-automatic method was 175.67 ±49.08 s, while the mean time for the automatic method was 175.00 ±68.08 s. The Mann–Whitney U test revealed no statistically significant difference in time between the 2 techniques. A standardized assessment technique was used in our study to ensure a comprehensive and uniform comparison. For the semi-automatic method, the time was recorded from the initiation of segmentation by the operator until its completion. For the AI-based evaluation, the time was recorded after the activation of the segmentation command until the generation of the segmented output. This is in contrast to a study conducted by Lahoud et al., in which the overall time was recorded from the initial DICOM file upload to the software/AI-based model to the visualization of results.31 Their findings demonstrated that AI exhibited a significantly higher processing speed than the manual segmentation, with a factor of 107.31
Limitations
This study has several limitations that should be considered when interpreting the results. The 3D models of the IAC obtained from the semi-automatic and automatic segmentation methods differ in shape. In the semi-automatic procedure, the shape of the IAC is that of a tube with a fixed diameter. In contrast, the shape of the IAC in the automatic procedure varies along the length of the canal.
Another limitation is that Diagnocat segmentation results in a wide segmentation of the IAC at the mandibular entrance. In contrast, the semi-automatic method yields a narrow segmentation at the same location. This discrepancy in segmentation width may lead to errors when the results of the 2 methods are overlapped and compared (Figure 6).
Additionally, in the case of the AI-based automatic segmentation, the algorithm did not correctly detect the IAC in some areas of the CBCT image. This resulted in an underestimation or even complete absence of the IAC diameter, which in turn led to the exclusion of portions of the 3D model (Figure 7).
The current findings must be viewed with caution, as the sample size was relatively small. Further research with a larger number of participants is required to confirm these results.
Conclusions
The results of our study demonstrated a low mean distance and a non-significant discrepancy in time between the AI-based and semi-automatic segmentation methods. The findings indicate that the AI-based segmentation has the potential to serve as a reliable assisting tool in pre-surgical planning for dental procedures. Further studies are required to make more direct comparisons and take into account the limitations mentioned in our study.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and exempted from ethical approval on the grounds of its observational nature. The Ethics Committee of Poznan University of Medical Sciences granted a waiver of patient consent for the use of anonymized radiographs in this retrospective study.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.