Abstract
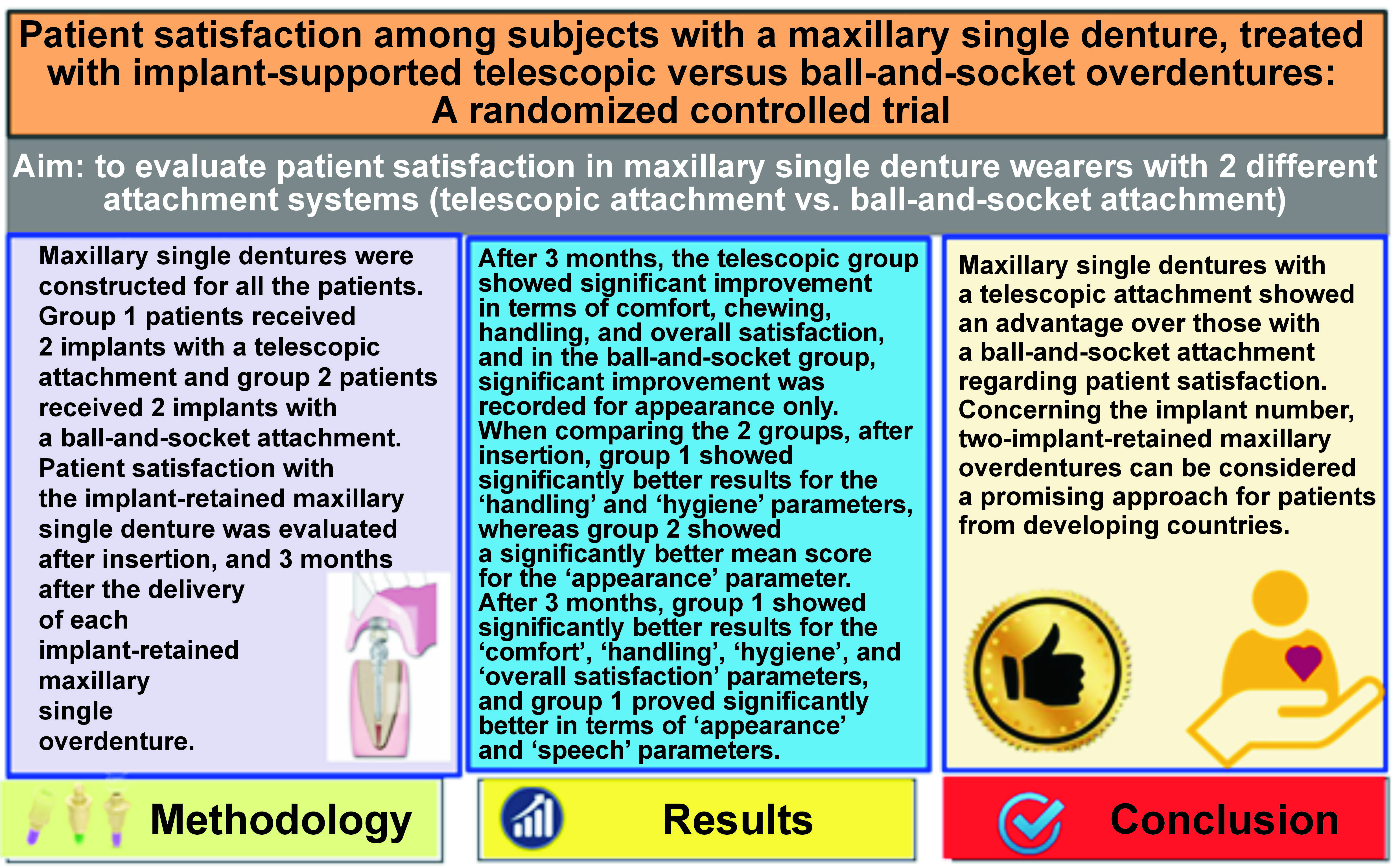
Background. The present study was performed to rehabilitate maxillary single denture cases with implant-retained telescopic or ball-and-socket attachments, and to evaluate the validity of two-implant-retained maxillary overdentures as a treatment approach in the maxillary arch.
Objectives. The aim of the present study was to evaluate patient satisfaction in maxillary single denture wearers with 2 different attachment systems (telescopic attachment vs. ball-and-socket attachment).
Material and methods. A total of 18 completely edentulous maxillary ridge patients (45–60 years old; mean age: 53 years) were selected for this study. Maxillary single dentures were constructed for all the patients. Group 1 patients received 2 implants with a telescopic attachment and group 2 patients received 2 implants with a ball-and-socket attachment. Patient satisfaction with the implant-retained maxillary single denture was evaluated after insertion, and 3 months after the delivery of each implant-retained maxillary single overdenture.
Results. All 18 patients completed the study. After 3 months, the telescopic group showed significant improvement in terms of comfort, chewing, handling, and overall satisfaction, and in the ball-and-socket group, significant improvement was recorded for appearance only. When comparing the 2 groups, after insertion, group 1 showed significantly better results for the ‘handling’ and ‘hygiene’ parameters, whereas group 2 showed a significantly better mean score for the ‘appearance’ parameter. After 3 months, group 1 showed significantly better results for the ‘comfort’, ‘handling’, ‘hygiene’, and ‘overall satisfaction’ parameters, and group 1 proved significantly better in terms of ‘appearance’ and ‘speech’ parameters.
Conclusions. Maxillary single dentures with a telescopic attachment showed an advantage over those with a ball-and-socket attachment regarding patient satisfaction. Concerning the implant number, two-implant-retained maxillary overdentures can be considered a promising approach for patients from developing countries.
Keywords: patient satisfaction, telescopic attachment, ball-and-socket attachment, implant overdenture, maxillary single complete denture
Introduction
Patients who are completely edentulous in one jaw, but have all or some of their natural teeth in the other jaw, represent one of the most frequent clinical scenarios. It is difficult, and perhaps nearly impossible, to get an effective complete denture for these people, There are 2 reasons that make the task so challenging. First, the occlusal form of the denture will be greatly influenced by the occlusal shape of the remaining natural teeth, which may be overerupted or slanted. Another issue is how hard and firm the natural teeth are when they are embedded in the bone.1
In the literature, maxillary implant overdentures are described with the implant survival rates ranging from 81% to 100% for up to 5 years, and being retained with 2–6 unsplinted implants.2, 3, 4 According to a systematic review, at least 4 implants should be placed, both anteriorly and posteriorly.5 However, short-term results from a prospective study show that outcomes with 4 unsplinted implants placed in the canine and molar regions were less successful.6 Later on, Boven et al. in their clinical study found that patients with all implants in the anterior position had marginally higher bone loss around 4 unsplinted implants as compared to splinted implants.7 In a crossover clinical trial, the placement of 2 and 4 unsplinted implants to retain a maxillary overdenture resulted in comparable clinical outcomes, although patients preferred 4 implants.8 Moreover, according to the systematic review performed by Klemetti, neither the number of implants nor the type of attachment in the maxilla had any influence on the long-term reliability of the final prosthesis or the satisfaction of the patient.9
Patients with edentulous maxillary arches now have new confidence with the advent of dental implant therapy, which improves prosthetic retention, support, stability, and biting force. Different attachment methods are employed to keep an overdenture in place, including studs, telescopes, bars with clips, and magnets. Studs have become very popular in clinical therapy due to their straightforward application. Bars are more difficult to clean and more technique-sensitive than solitary attachments.10
Due to the intimate fit between the primary and secondary copes, and the improved force dissemination caused by the axial transmission of the occlusal load, telescopic attachments offer excellent retention. Additionally, the overdentures are self-locating and simple to remove. In order to gage patient satisfaction, dentists should pay close attention to each patient’s perception of their degree of comfort, appearance, emotion, function, speech, and confidence. The ultimate objective is to reach a level where edentulous patients are completely satisfied with the therapy, and are more aware of how edentulism affects their quality of life.11, 12
Consequently, this clinical research was conducted to assess if implant-retained maxillary single dentures with a telescopic attachment are an effective alternative to implant-retained maxillary single dentures with a ball-and-socket attachment. The PICOT question addressed here was: In patients with maxillary single dentures (P), will implant-retained maxillary single overdentures with a telescopic attachment (I) result in the equivalence of patient satisfaction (O) in comparison with implant-retained maxillary single overdentures with a ball-and-socket attachment (C) after 3 months of follow-up (T) This trial was done following the CONSORT (Consolidated Standards of Reporting Trials) statement.
Material and methods
Trial design and setting
A parallel-group, 1:1 allocation ratio, randomized clinical trial (RCT) was intended for the investigation. A total of 18 Egyptian patients, 13 males and 5 females, aged 45–60 years (mean age: 53 years), with a fully edentulous maxillary arch opposite a fully or partially dentate mandibular arch, were chosen for this clinical trial from the outpatient clinic of the Department of Prosthodontics at Ahram Canadian University, 6th of October City, Egypt, and the dental clinic of the National Research Center, Cairo, Egypt. The chosen patients had either totally or partially dentate mandibular arches, as well as fully edentulous maxillary ridges. The patients were randomly assigned to the following groups: group 1 (intervention) – the patients received maxillary single dentures retained with a telescopic attachment (a resilient, custom-made telescopic crown); or group 2 (control) – the patients received maxillary single dentures retained with a ball-and-socket attachment (Dentis Implant System Attachment; Dentis Co., Ltd., Daegu, South Korea).
Randomization process
Using a research randomizer (https://www.randomizer.org), the 18 patients were randomly assigned to 2 groups (intervention or control), each containing 9 patients, after the manufacture of maxillary full dentures.
Allocation concealment
Only one investigator (M.H.M.), who took no part in patient selection or treatment, was aware of the randomization sequence and had access to the randomization lists kept on a portable computer that was password-protected. The randomly generated codes were placed in identical, sequentially numbered, sealed, opaque envelopes. The patients were asked to choose one of the envelopes. The investigator who was aware of the randomization procedure was then asked to designate the group, and the patient was treated appropriately.
Blinding
Apparently, neither the participants nor the care providers could be blinded, as the 2 attachment systems were obviously different, but the care providers were instructed to avoid commenting about treatment possibilities to the subjects. Patient satisfaction was assessed by an independent assessor, who was not aware of the type of intervention. The statistician was blinded.
Eligibility criteria for the selected cases
The inclusion criteria were as follows: patients having a completely edentulous maxilla; aged 45–60 years; free from any systemic diseases that may affect bone metabolism; non-smokers; with sufficient interarch space (not less than 15 mm); with maxillary ridges well-formed and covered with firm and healthy mucosa, free from inflammation, ulceration and flappy tissues; with angle Class I maxillomandibular relationship; at least 6–12 months having elapsed since the last tooth extraction; and no previous denture experience.
The exclusion criteria were as follows: patients with the dysfunction of the temporomandibular joint (TMJ), which would impair the prosthetic outcomes; medically compromised patients (an impact on the surgical placement of implants); subjects with a partially edentulous maxillary arch (it could affect the value of the study); uncooperative patients, who might not return for the follow-up, examinations or evaluation; and patients with a history of a surgical operation in the maxillofacial region.
All patients were requested to sign an informed consent form, which was translated into Arabic to be understood. The trial was conducted in accordance with the Declaration of Helsinki (2008).
Preparations
All the required mouth preparations were carried out for the lower natural teeth, including periodontal, surgical, restorative, and prosthetic procedures, as well as occlusal corrections. A conventional single maxillary denture was constructed after the rehabilitation and occlusal adjustment of the mandibular teeth. The patients were asked to wear their denture after it was modified by adding gutta-percha as a radiopaque detector for achieving dual scanning.
The cone-beam computed tomography (CBCT) radiograph of the maxillary arch was evaluated to determine the available bone height, using the Blue Sky Plan® software, v. 3.29.28 (https://blueskybio.com). Virtual implants (Dentis Implant System; Dentis Co., Ltd.) were placed and checked to be at least 2 mm away from any of the vital structures. Also, 1.5 mm of bone was checked to be present, both labially and lingually. Two virtual implants were placed in each maxillary edentulous arch, and the parallelism between them was checked. Once the positions of the implants were accepted in the virtual guide, 2 holes were designed in the software, corresponding to the prefabricated metal sleeves.
This trial was carried out using CBCT imaging and the flapless surgical technique to place 2 implants in the maxillary arch, utilizing tissue-supported computer-aided surgical guides. The 2 implants were then prosthetically restored with either telescopic or ball-and-socket attachments.
Surgical procedures
Root-formed, tapered, threaded dental implants, having dimensions of 4 mm in diameter and 12 mm in length (for canine regions) were prepared before surgery. Two implants were installed according to the flapless delayed implant placement protocol in the canine areas.
Prosthetic procedures
Once the implant osseointegration appeared satisfactory, patients were randomly divided into 2 equal groups according to the attachments used for retaining the maxillary overdenture.
The principles of clinical and laboratory procedures were followed for the construction of a single denture.
In group 2 (control), the ball-and-socket attachments were placed, and the direct pick-up technique was applied, as conventionally as possible.
For group 1, permanent transmucosal titanium (Ti) abutments (Octa®; Dentis Co. Ltd.) were fastened into the implant fixtures with an Octa driver until resistance was achieved, and then torqued up to 35 N·cm, using torque ratchets. Impression copings were placed over the abutments, and then splinted at the abutment level (the open-tray impression technique). The centric jaw relation was recorded using the wax wafer technique. The mounting and and setting up of cross-linked acrylic teeth (Vertex™ Quint Teeth; Vertex Dental, Soesterberg, the Netherlands) was performed like in conventional denture construction. The putty index was obtained using a rubber base (Labor Plus; Dental Line LTD, Inofita Viotias, Greece), and applied over the labial and occlusal surfaces to estimate the ideal size for primary and secondary copings. Then, an anti-rotational plastic cap was screwed to the analog and a resilient telescopic crown was fabricated. The wax pattern of the primary coping was built up with the use of milling wax. The primary copings of the telescopic attachments were cast into chrome-cobalt (Cr-Co) alloy. The primary crown was designed with a taper of 6° and a height of 5 mm. Next, secondary metal copings were fabricated over the primary copings. The secondary crown was designed with an occlusal free space of 0.4 mm between the primary and secondary crowns, and a small amount of circumferential space of 0.04 mm between the 2 crowns, so that vertical movement between the 2 crowns could be allowed. After waxing up, the try-in with artificial teeth in the patient’s mouth was done. Then, the laboratory procedures continued in the usual manner. The insertion of the final denture in the patient’s mouth was done following the same conventional steps.
Examination procedures – patient satisfaction
A valid version of the visual analog scale (VAS) questionnaire was used and translated to Arabic for recording patient satisfaction in terms of comfort, appearance, speech, retention, stability, chewing, handling, hygiene, and overall satisfaction. The patients were instructed to rate the denture parameters on a 100-point scale. Most patients were unsatisfied with their conventional single dentures and were looking for an implant therapy option.
The records were taken after implant insertion and 3 months post-insertion.
Sample size and power analysis
Taking into account the t test results based on the overall satisfaction scores at 3 months postoperatively (group 1: 90.5 ±2.56 vs. group 2: 86.8 ±1.48), the standardized mean difference two-tail effect size (d) amounted to 1.769 and the power (1β error probability) was 94.06%. A sample size of 9 patients per group (2 groups in total) was sufficient to conduct the study with a power >80%. The post hoc calculations were made using G*Power, v. 3.1.9.2 (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower).13
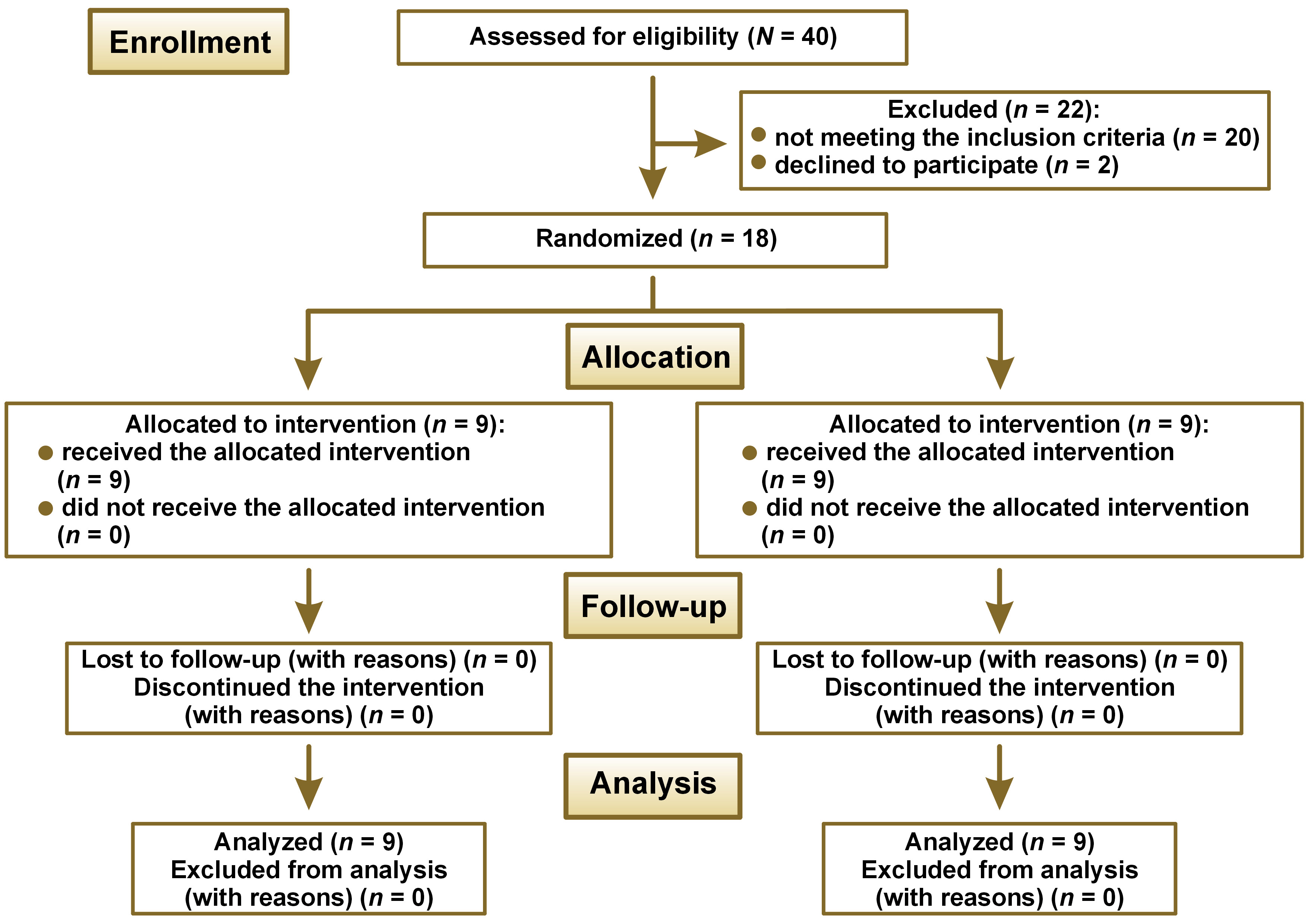
The study sample comprised 18 patients with a completely edentulous maxillary arch opposing a fully or partially dentate mandibular arch. A total of 36 implants were placed. The follow-up was completed by all patients. No implant failed in any of the included patients, giving a final follow-up success rate of 100% (Figure 1).
Statistical analysis
The mean and standard deviation (M ±SD) values were used to represent numerical data. To check for normality, the Shapiro–Wilk test was applied. The Mann–Whitney U test for intergroup comparisons and the Wilcoxon signed-rank test for intragroup comparisons were used to assess the non-parametric data. For all tests, the Bonferroni adjustment was used to adjust p-values for multiple comparisons. The significance level was set at p < 0.05. The R program, v. 4.1.3 (https://www.r-project.org), was used to conduct the statistical analysis.
Results
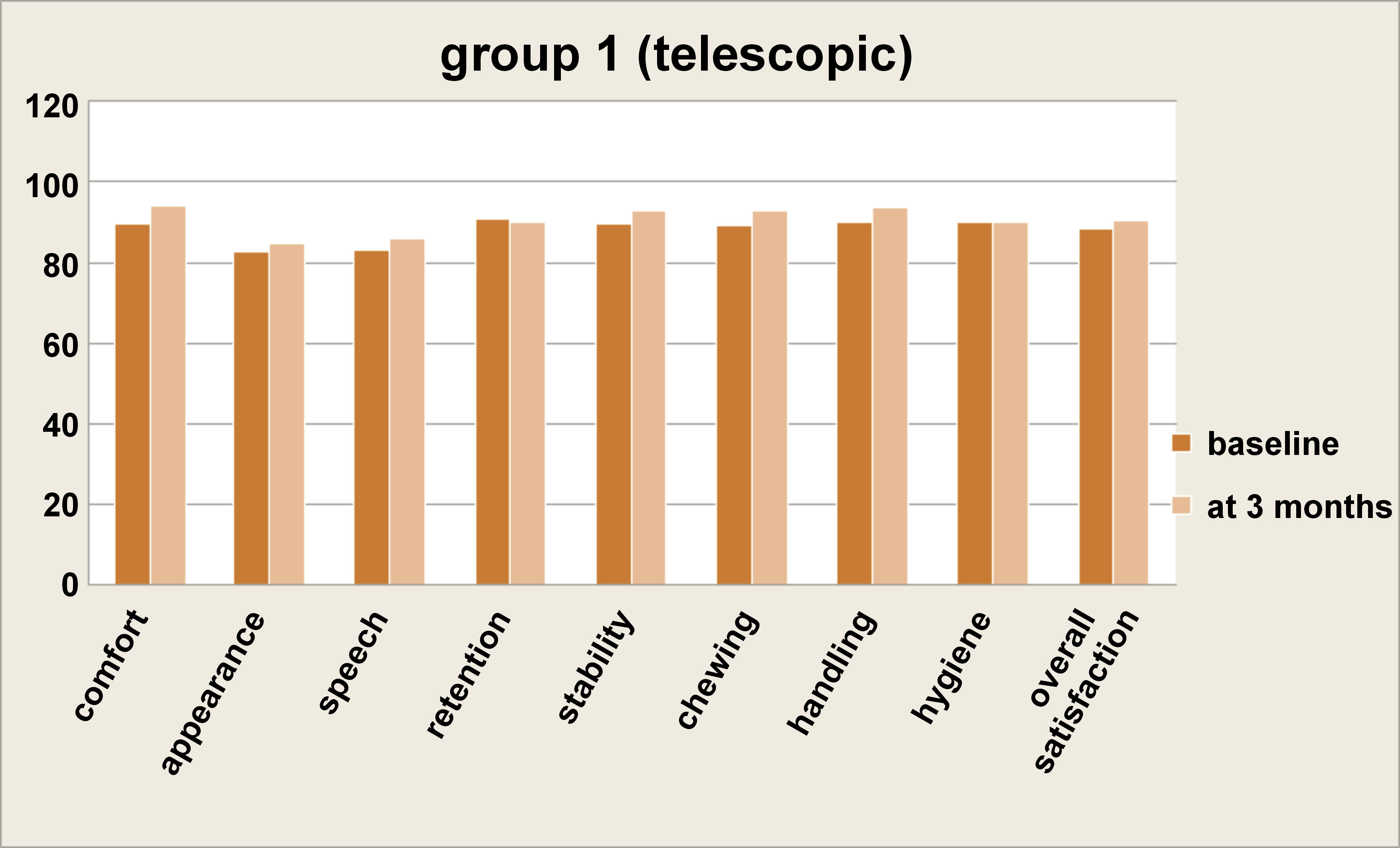
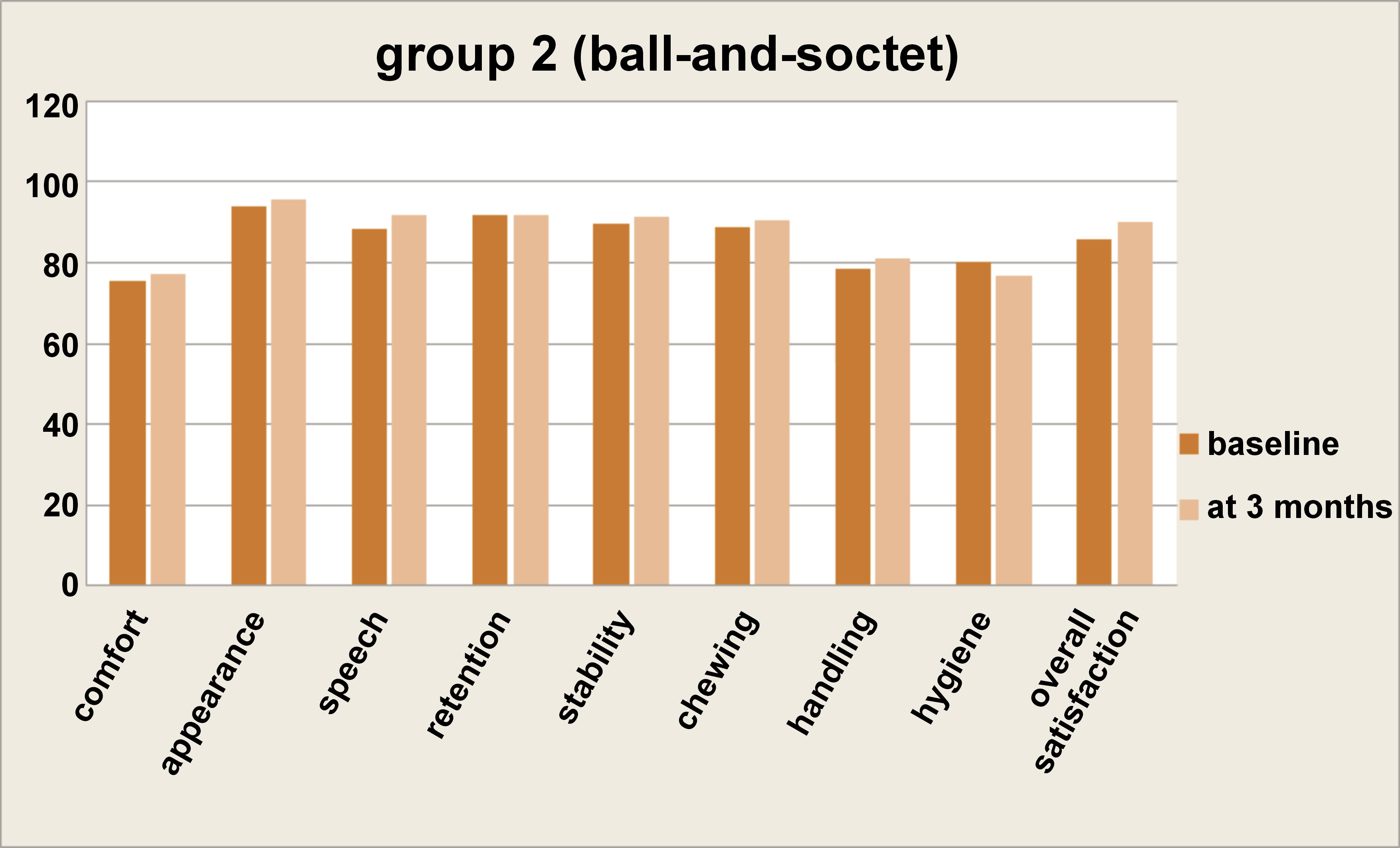
The results of intragroup comparisons for the satisfaction scores are presented in Table 1. They showed that in group 1 there was a significant increase in the measured scores after 3 months for the ‘comfort’, ‘chewing’, ‘handling’, and ‘overall satisfaction’ categories (p < 0.05), while in group 2 there was a significant increase in the ‘appearance’ parameter only (p < 0.05); for other parameters, the change was not statistically significant (p > 0.05). The mean satisfaction scores for the telescopic and ball-and-socket groups are presented in Figure 2 and Figure 3.
The results of intergroup comparisons for the satisfaction scores are presented in Table 2. After insertion, group 1 showed significantly better results for the ‘handling’ and ‘hygiene’ parameters, whereas group 2 showed a significantly better mean score for the ‘appearance’ parameter (p < 0.05). After 3 months, group 1 showed significantly better results for the ‘comfort’, ‘handling’, ‘hygiene’, and ‘overall satisfaction’ parameters, and group 1 proved significantly better in terms of ‘appearance’ and ‘speech’ parameters (p < 0.05).
Discussion
Our trial evaluated 2 different attachment systems – telescopic and ball-and-socket – in terms of their effect on patient satisfaction in the wearers of implant-retained maxillary single overdentures. At the end of the follow-up, the telescopic group in our study displayed a significantly higher level of comfort, handling, cleanliness, and general satisfaction as compared to the control group, whereas the ball-and-socket group displayed a significantly higher satisfaction level with regard to appearance and speech. The levels of patient satisfaction were measured using VAS.
With regard to the 1st assessment, our study found that the telescopic group showed significantly better results for the ‘handling’ and ‘hygiene’ satisfaction categories as compared to the ball-and-socket group. This could be due to a proper path of insertion and more freedom while placing the telescopic attachments as compared to ball attachments; which is in agreement with a previous study.14
Furthermore, there was a significant difference between the study groups concerning the ‘appearance’ parameter in the initial period, in favor of the ball-and-socket group. This could be explained by the presence of the primary and secondary copings of the telescopic attachment, which increased the bulk of the prosthesis and decreased the satisfaction level regarding appearance.
After 3 months, the telescopic group showed a significant increase in comfort, handling, hygiene, and overall satisfaction as compared to the ball-and-socket group, which confirms the fact that ball-and-socket attachments make it more challenging to position the denture in the mouth when compared to other attachments. Even with 2 such attachments, the patient still requires some additional ability to properly place a denture.15
As far as the telescopic attachments are concerned, our findings are in conformity with those of a previous study by Krennmair et al.16 The patients had no trouble with cleaning the overdenture, as evidenced by the periodic recall visits, which implied no signs of irritation of the tissues around the implants.16 The absence of the undercut stagnation areas in telescopic attachments is the reason for considering them as hygienic attachments, which allow easy access for cleaning.14, 17 This may explain the significant increase in satisfaction with the cleaning of the prosthesis.
After 3 months, the ball-and-socket group showed significant improvement in appearance and speech. On the other side, the telescopic group showed a decrease in the scores for appearance and speech due to the increased bulk of the prosthesis labially and palatally, affecting articulation and increasing lip fullness. Improvement in speech occurred also in the telescopic group at 3 months; yet, the intergroup comparison revealed a significant difference between the groups in this regard.
Despite the fact that the use of telescopes to retain conventional overdentures on the natural teeth is a well-known treatment method, there is a scarcity of information on the use of telescopic crowns with implant-supported overdentures. Thus, the findings far suggest that this approach can result in predictable long-term therapeutic effects.18
Telescopic crowns are utilized as abutments, as they have several advantages over other types of attachments where cost-effectiveness is a major priority. Despite costing more than simple ball-and-socket attachments, they might give the prosthesis additional stability and retention due to their design. The requirement for continuing maintenance may be lessened by the fact that telescopic crowns last longer than conventional attachments. Some dentists may also choose telescopic crowns due to their versatility in being employed as a component of a fixed prosthesis or as a support for a removable partial denture.16
According to a study that examined a resilient telescopic connection over a 10-year period, non-rigid telescopic connectors with 2 interforaminal implants appeared to be a long-term treatment option that was efficient and successful.19 This idea may offer benefits in terms of handling, cleanliness and long-term satisfaction, particularly in the care of senior patients. In our study, we used a resilient telescopic attachment to enable straightforward manipulation, reduce the stresses reflected on the implant and permit some degree of vertical movement, comparable to that observed for a ball-and-socket attachment.
Patients with severe maxillary resorption, who do not want to have reconstructive surgery, may benefit from two-implant-supported maxillary overdentures. In a previous study, the efficiency of maxillary overdentures supported by 2 implants in individuals with an atrophic maxilla was examined.20 The findings demonstrated positive implant and overdenture survival rates, while the masticatory function and patient satisfaction considerably improved with regard to baseline. The patients had a comparably significant chance of implant loss. Maxillary implant overdentures on 2 or 4 implants were both suggested, within the limitations of the study.20
A computerized stent can provide a high degree of parallelism among the dental implants needed for telescopic attachments, improving the passive fit of the superstructure, preventing determinant lateral forces on the implant fixture, and minimizing tipping forces on the implants during prosthesis placement and removal.21
Our results agree with the results of other studies, which suggested that implant-retained telescopic attachments may be an appropriate alternative for the standard ball-and-socket attachments. In comparison with other types of implant-supported solitary attachments, the application of a double crown over dentures provides a long-term therapeutic effect.22
Due to rotational stability and the presence of a frictional fit, the use of telescopic attachments may offer an acceptable and prosthetically straightforward retention modality. This kind of retention functions similarly as in other single attachments, including one-piece abutments, like a ball-and-socket attachment, because the abutment and the inner telescope form an integral unit. Nevertheless, it definitely offers broad prosthetic, technological, economic, and clinical benefits.23, 24
On the other hand, experimental investigations on implant overdentures that evaluated denture-bearing areas, using 4 types of attachments found that telescopic crowns showed similar results as bars, balls and magnets; some studies revealed that there was a low dropout rate in both the ball-and-socket group and the telescopic group throughout the whole follow-up period.25, 26
Additionally, a study comparing the retention of Ti and biocompatible high-performance polymer (BioHPP) telescopic abutments found that after simulating a year of overdenture use, the telescopic overdenture supported by abutments at a 2-degree angle demonstrated a significant decrease in the retentive force values. Titanium and BioHPP were both regarded as appropriate materials to hold telescopic implant overdentures in place.27
Patient satisfaction with a newly constructed implant-retained maxillary single overdenture was assessed using VAS, which is frequently employed as a guide for an agreed-upon or refused treatment outcome. Patients’ pleasure with their implant-retained maxillary single overdenture is often recognized as vital for adaptation to newly constructed overdentures. The VAS is considered a reliable and efficient tool for evaluating the main variances between different countries and cultures.28, 29
According to our study results, the telescopic attachment group showed a significant increase in overall satisfaction as compared to the ball-and-socket group; this is in agreement with a recent systematic review performed to compare the effects of different attachment systems.30
Due to higher expenses and the fact that more implants necessitate more expensive treatment, many patients decide not to receive four-implant overdenture therapy. Thus, the 2-implant maxillary overdenture with full palatal coverage acts as a bridge between the conventional complete denture and the four-implant overdenture.
The suggested treatment option is most successful in patients who have an atrophic maxilla, a shallow palatal vault or xerostomia, without an anterior maxillary undercut. In order to address the limitations of the current study (a short follow-up period and a small sample size), longer follow-up times and a larger sample size are required.
Conclusions
Within the constraints of this investigation, the following conclusion can be drawn:
Implant-retained maxillary single overdentures with a telescopic attachment showed an advantage over implant-retained maxillary single overdentures with a ball-and-socket attachment regarding comfort, handling, hygiene, and overall patient satisfaction.
Recommendation
It is advisable to do larger, expertly conducted RCTs, with extended follow-up times, and a range of functional, prosthodontic and patient-reported outcome measures.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee at the Faculty of Oral and Dental Medicine, Ahram Canadian University, 6th of October City, Egypt (approval No. IRB00012891#37). All patients provided written informed consent prior to the commencement of the trial.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.