Abstract
Background. Dental anxiety is characterized by distress in anticipation of dental visits, which may result in a child’s refusal to undergo treatment and, ultimately, lead to parents’ reluctance towards dental care.
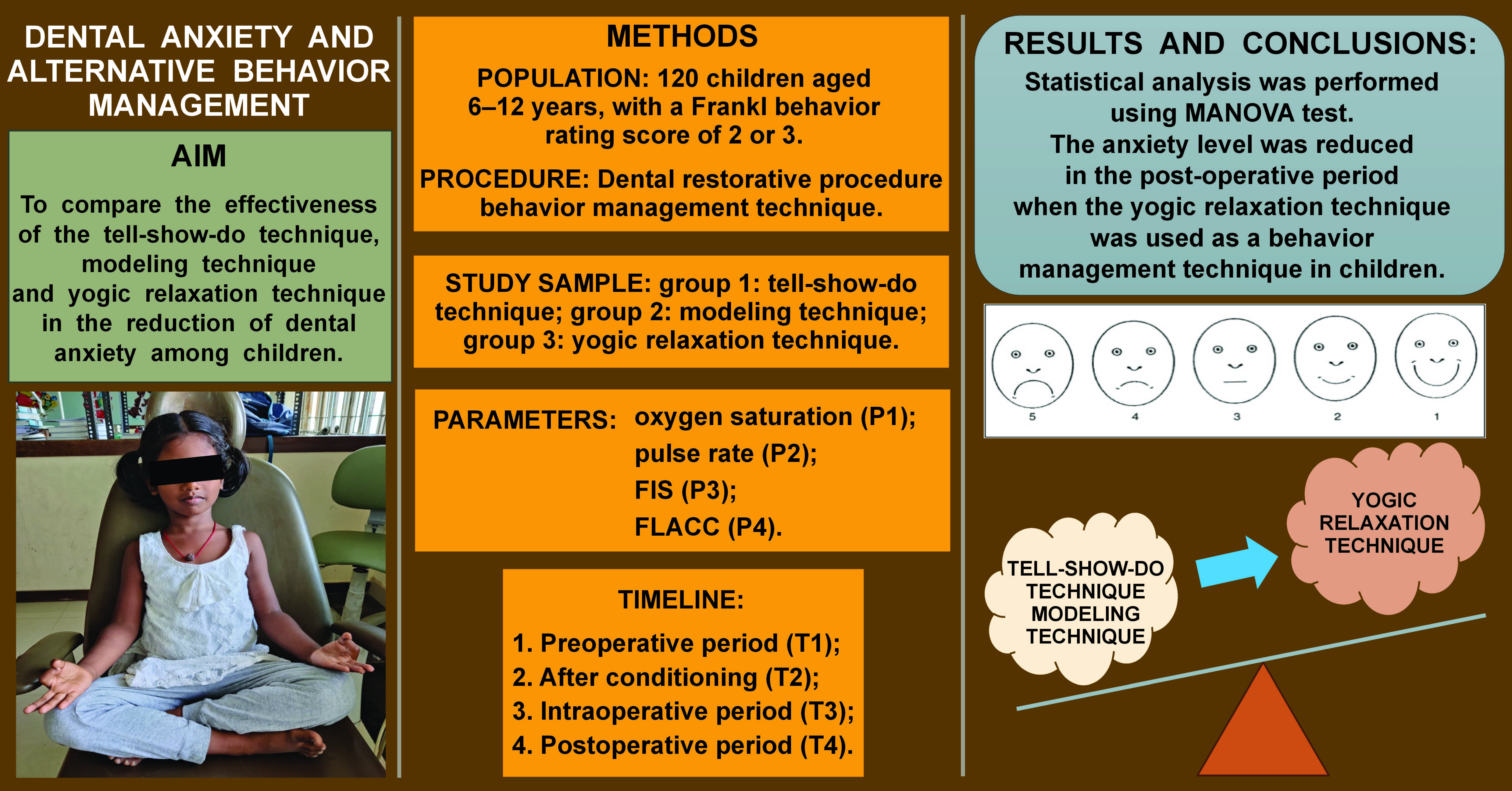
Objectives. The aim of this study was to evaluate and compare the effectiveness of the tell-show-do technique, modeling technique and yogic relaxation technique in the reduction of dental anxiety among children aged 6–12 years.
Material and methods. The study was an interventional, parallel-group, single-center, double-blind, randomized controlled trial conducted on 120 children who required restorative treatment without the use of local anesthesia. The participants were selected based on specific inclusion and exclusion criteria and were randomly divided into 3 groups: group 1 – tell-show-do technique; group 2 – modeling technique; group 3 – yogic relaxation technique. The dental anxiety levels were evaluated 4 times using both physiological (oxygen saturation and pulse rate) and behavioral parameters (facial image scale (FIS) and the Face, Legs, Activity, Cry, and Consolability scale (FLACC)). The data was assessed by 2 blinded and calibrated specialists.
Results. Statistically significant differences were observed in all 4 parameters among the 3 groups. During both the intraoperative and postoperative periods, the oxygen saturation levels were significantly higher in the yogic relaxation technique group. Moreover, the yogic relaxation technique group exhibited lower pulse rates, FIS and FLACC scores compared to the tell-show-do and modeling technique groups.
Conclusions. The practice of yoga has a positive influence on the general health of the individual. Consequently, it can be considered one of the alternative behavioral modification techniques for the reduction of dental anxiety in children.
Keywords: anxiety, dental anxiety, behavior, yoga, dental fear
Introduction
Anxiety is characterized by disruptions in mood, thinking, behavior, and physiological processes, and is often misunderstood as fear. A planned procedure may be avoided by patients who are experiencing anxiety, due to its unpleasant nature.1, 2 Thus, anxiety is an emotional state that occurs before the actual encounter with the threatening stimuli, which is not always identifiable. On the other hand, fear is a response to a real or hypothetical threat or danger.3 Dental anxiety is the 5th most common cause of anxiety.4 The prevalence of dental anxiety is estimated to range from 6% to 20% in children between the ages of 4 and 18.5 According to the Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV and the International Statistical Classification of Diseases and Related Health Problems,3 a condition associated with fear of dentistry along with hypertension, apprehension, trepidation, and uneasiness is referred to as odontophobia.3
Dental anxiety is defined as “the distressed expectation of a visit to a dentist to the extent where a child might avoid treatment.”6 Early onset of dental anxiety is associated with a greater incidence of dental caries, which may ultimately lead to the early removal of the affected tooth due to the child’s fear of attending the dental clinic. Compromised oral hygiene may result in a poor oral health-related quality of life. The sequence of events that an individual experiences during childhood will continue into adulthood through adolescence, having a negative impact on the oral health of the individual.7, 8, 9
Parent involvement has a significant impact on how well a child handles the pressures and stimuli associated with dental care.10 The cognitive behavioral treatment, which is widely utilized in psychology and psychiatry for both adult and pediatric patients, serves as the foundation for the behavioral management approach.11
The provision of dental treatment for anxious children requires a cautious approach. In addition to meeting their healthcare needs, it should address any behavioral issues. Behavior management is an important aspect in the treatment of pediatric patients, as it inculcates the basic coping mechanisms and helps the child handle the stressful situation in a more acceptable way. It is not possible to achieve this coping mechanism in subsequent dental visits through the use of pharmacological methods. Thus, behavior modification through a non-pharmacological approach is the optimal choice for establishing long-term coping mechanisms in children.12 However, if non-pharmacological methods of the behavior modification prove ineffective, pharmacological techniques such as sedation and general anesthesia can be employed.13 Furthermore, yoga and meditation address a child’s entire being, including their physical, mental, emotional, psychic, and spiritual well-being. Yoga provides total body synchronization and aids in the reduction of stress and anxiety. It is a simple and effective non-pharmacological intervention for the reduction of dental anxiety.14
Thus, the aim of this study was to compare 3 different behavior management techniques (the tell-show-do technique, modeling technique and yogic relaxation technique) for the reduction of dental anxiety in children aged 6–12 years.
Hypotheses
The alternative hypothesis suggests that the yogic relaxation technique has a better anxiolytic effect compared to the tell-show-do and modeling techniques.
The null hypothesis posits that the yogic relaxation technique has no or little anxiolytic effect in comparison to the tell-show-do and modeling techniques in reducing dental anxiety.
Material and methods
Study design
This study was designed as an interventional, parallel-group, single-center, double-blind, randomized controlled trial with a comparative analysis of the 3 groups among the pediatric population who presented to the Outpatient Department of Pedodontics and Preventive Dentistry (Chettinad Dental College and Research Institute, Chennai, India) between September 2022 and March 2023.
The study was approved by the ethical clearance board of Chettinad Academy of Research and Education, Chennai, India (approval No. IHEC-I/1302/22).
Study sample
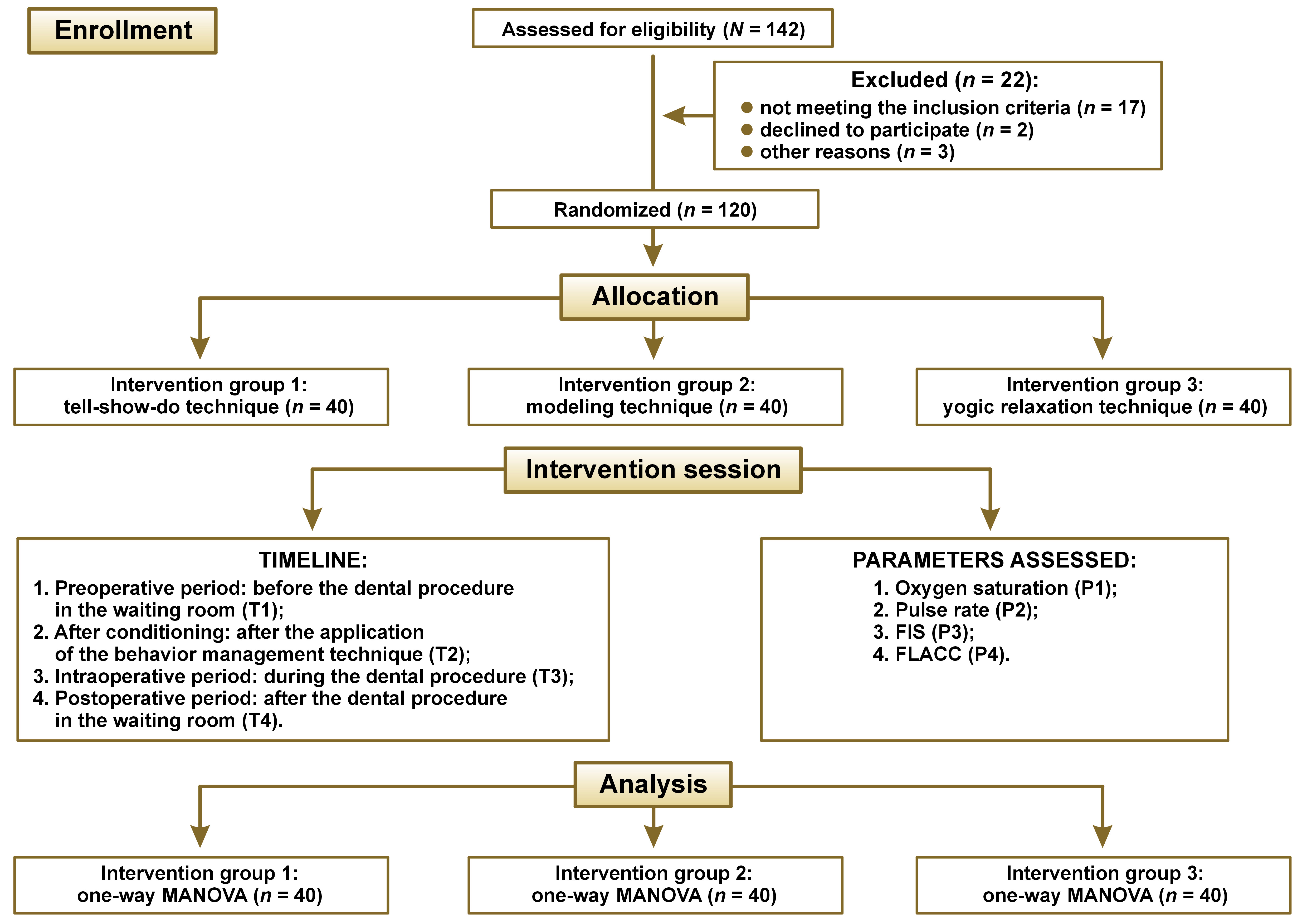
The study sample included children aged 6–12 years who were in the pre-operational and concrete operational stages of cognitive development. A total sample size of 120 was calculated using G*Power software (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower), with an alpha error of 0.05, a beta power of 0.9 and an effect size of 0.33. The children and their parents reported with the chief complaint of dental caries. After initial clinical diagnosis and screening, children experiencing pain that required more invasive procedures were excluded from the study.
Inclusion criteria
The inclusion criteria for the study were as follows: children aged between 6 and 12 years; children attending their first dental visit; children requiring restorative treatment for their decayed teeth; and children with a Frankl behavior rating score of 2 or 3 (negative/positive).
Exclusion criteria
The study excluded children with mental or cognitive issues that could impair their comprehension or participation in the study, medically compromised children with systemic abnormalities that could influence the child’s pulse rate and heart, children with a previous history of trauma to the teeth with pulpal involvement, children whose parents were not willing to consent to the treatment, and children requiring endodontic treatment or extraction for their chief complaint.
Study sample selection
After the comprehensive screening process, 64 boys and 56 girls (N = 120) were selected for inclusion in the study. The children were randomly allocated into 3 equal groups using the lottery method, based on the type of behavior management technique they received: group 1: tell-show-do technique; group 2: modeling technique; group 3: yogic relaxation technique.
Data collection
The following parameters were evaluated in the course of the study: oxygen saturation (P1); pulse rate (P2); facial image scale (FIS) (P3); and the Face, Leg, Activity, Cry, and Consolability scale (FLACC) (P4).
The parameters were measured at 4 different time points during the course of the dental procedure:
1. Preoperative period: before the dental procedure in the waiting room (T1);
2. After conditioning: after the application of the alloted behavior management technique in respective groups (T2);
3. Intraoperative period: during the dental procedure (T3);
4. Postoperative period: after the dental procedure in the waiting room (T4).
The Consolidated Standards of Reporting Trials (CONSORT) flowchart, which provides a visual representation of the study procedure, is presented in Figure 1.
Intervention
Group 1: Tell-show-do technique
For children in group 1, the nature of the procedure was explained in a non-threatening and intelligible manner, in the language that the children were most comfortable with. Each child was presented with the required armamentarium and the procedure was mimicked in a typodont. The child observed the procedure being carried out by the dentist (Figure 2). After the observation phase, the child was reassured, and, with their consent, the dental procedure was initiated.
Group 2: Modeling technique
The child observed the procedure that was carried out on a model, which allowed the patient to gain insight into the nature of the procedure (Figure 3). The model was either the child’s sibling or another patient in the same age group who was undergoing similar treatment. Once the procedure had been completed on the model, the child was reassured and, with their consent, the dental procedure was initiated.
Group 3: Yogic relaxation technique
The child was instructed to perform 3 different yoga poses while seated in the dental chair:
1. Pancha Kosha (Figure 4A);
2. Bhramari Pranayama (Figure 4B);
3. Nadi Shodhana (Figure 4C).
The child was asked to watch a virtually recorded visual demonstration of the yoga poses. Each pose was performed for 5 min under the supervision of the dental professional. Once the yoga session was completed, a 10-min interval was given, after which the dental procedure was initiated.
The values for 3 different parameters (P1–P3) evaluated in the study were recorded on 4 occasions (T1–T4) for each group. The FLACC scores (P4) were recorded only during the intraoperative period (T3).
Dental procedure
After the intervention, the children in all 3 groups were prepared for the dental procedure. A class 1 or class 2 dental cavity preparation was carried out in primary/permanent molars. The surface was etched, rinsed, and a bonding agent was applied and cured. An appropriate shade of composite restoration was then placed and cured, and the occlusal adjustments were made. The entire procedure, from the initial stage of the cavity preparation to the placement of the restorative material and occlusal adjustment was completed in 20–30 min.
Statistical analysis
Descriptive and inferential statistics were analyzed using the IBM SPSS Statistics for Windows software, v. 20.0 (IBM Corp., Armonk, USA). The mean (M) and standard deviation (SD) were used to summarize the quantitative data. Multivariate analysis of variance (MANOVA) was employed to conduct intergroup comparisons of the 3 groups for the analyzed parameters (P1–P4) at various time points (T1–T4). A p-value of less than 0.05 was considered statistically significant.
Results
Preoperative period
The MANOVA test was conducted to examine the multivariate effects of the variable “group” on the dependent variables. The Pillai’s trace test statistic yielded a significant result (F = 4.873, degrees of freedom (df) = 6.000, error df = 52.000, p = 0.001), indicating that there is a statistically significant multivariate effect of the “group” variable on the dependent variables. The effect size, as indicated by partial eta squared, was moderate (0.360). Additionally, the Wilks’ lambda test statistic yielded a significant result (F = 5.351, df = 6.000, error df = 50.000, p < 0.001), providing additional evidence for the presence of a significant multivariate effect. The effect size was moderate (0.391). The Hotelling’s trace test statistic was found to be significant (F = 5.807, df = 6.000, error df = 48.000, p < 0.001), providing further evidence of a significant multivariate effect, with a moderate effect size (0.421). Finally, the Roy’s largest root test statistic yielded a highly significant result (F = 10.896, df = 3.000, error df = 26.000, p < 0.001), indicating a substantial multivariate effect of the “group” variable on the dependent variables. The effect size was large (0.557). Overall, the results of the MANOVA test demonstrate that the variable “group” has a significant and meaningful multivariate effect on the dependent variables (Table 1).
Table 2 shows the results of the between-subject effects analysis for the dependent variables “oxygen saturation”, “pulse rate” and “FIS” in relation to the independent variable “group.” With regard to the dependent variable “oxygen saturation”, the Type III sum of squares was 44.067, and the mean square was 22.033. The F-value was 2.821, and the p-value was 0.077, which is not statistically significant. The effect size, as measured by partial eta squared, was 0.173, indicating a small effect. With regard to the pulse rate, the Type III sum of squares was 48.200, and the mean square was 24.100. The F-value was 0.817, and the p-value was 0.452, indicating that the observed effect is not statistically significant. The effect size was small (0.057). In contrast, for the dependent variable “FIS”, the Type III sum of squares was 11.667, and the mean square was 5.833. The F-value was 13.938, and the p-value was <0.001, indicating a statistically significant effect. The effect size was considerable (0.508). In summary, the analysis demonstrates that the variable “group” has a significant influence on the dependent variable “FIS”, with a large effect size. No statistically significant effects of the “group” variable on the oxygen saturation and pulse rate were identified, although a small effect size was observed for the “oxygen saturation” variable.
After conditioning
Table 3 presents the results of the multivariate test after conditioning, examining the effects of the variable “group” on the dependent variables. The Pillai’s trace test statistic yielded a non-significant result (F = 0.585, df = 6.000, error df = 52.000, p = 0.740), suggesting that there is no statistically significant multivariate effect of the “group” variable on the dependent variables after conditioning. The effect size, as measured by partial eta squared, was 0.063, indicating a small effect. Similarly, the Wilks’ lambda test statistic yielded a non-significant result (F = 0.578, df = 6.000, error df = 50.000, p = 0.746), further confirming the abscence of a significant effect of the “group” variable on the dependent variables. The effect size was small (0.065). Additionally, the Hotelling’s trace test statistic was found to be non-significant (F = 0.570, df = 6.000, error df = 48.000, p = 0.752), with a small effect size (0.066). Finally, the Roy’s largest root test statistic also yielded a non-significant result (F = 1.162, df = 3.000, error df = 26.000, p = 0.343). The effect size was small (0.118). In summary, the results of the multivariate test after conditioning demonstrate that there is no statistically significant multivariate effect of the variable “group” on the dependent variables. The observed effect sizes are small, suggesting that the variable “group” has a minimal impact on the dependent variables after conditioning.
Intraoperative period
Table 4 presents the results of the multivariate test, indicating the effects of the variable “group” on the dependent variables in the intraoperative period. The Pillai’s trace test statistic yielded a significant result (F = 3.913, df = 8.000, error df = 50.000, p = 0.001), suggesting a statistically significant multivariate effect. The effect size, as measured by partial eta squared, was moderate (0.385). Similarly, the Wilks’ lambda test statistic yielded a significant result (F = 6.187, df = 8.000, error df = 48.000, p < 0.001), providing further evidence for the presence of a significant multivariate effect. The effect size was moderate (0.508). The Hotelling’s trace test statistic was found to be statistically significant (F = 8.838, df = 8.000, error df = 46.000, p < 0.001), with a large effect size (0.606). Finally, the Roy’s largest root test statistic yielded a highly significant result (F = 19.109, df = 4.000, error df = 25.000, p < 0.001), indicating a substantial multivariate effect of the variable “group” on the dependent variables. The effect size was large (0.754). In summary, the results of the multivariate test demonstrate that the variable “group” has a significant and meaningful multivariate effect on the dependent variables. The observed effect sizes are generally moderate to large, indicating a notable impact of the variable “group” on the dependent variables in the intraoperative period.
Table 5 presents the results of the between-subject effects analysis, examining the impact of the variable “group” on the dependent variables. With regard to the dependent variable “oxygen saturation”, the Type III sum of squares was 76.067, while the mean square was 38.033. The F-value was 3.506, and the p-value was 0.044, indicating a statistically significant result. The effect size, as measured by partial eta squared, was moderate (0.206). Regarding the dependent variable “pulse rate”, the Type III sum of squares was 447.200, and the mean square was 223.600. The F-value was 5.337, and the p-value was 0.011, which is statistically significant. The effect size was moderate (0.283). In relation to the FIS, the Type III sum of squares was 20.867, and the mean square was 10.433. The F-value was 8.668, and the p-value was 0.001, indicating a statistically significant effect. The effect size was large (0.391). Finally, for the dependent variable “FLACC”, the Type III sum of squares was 81.867, and the mean square was 40.933. The F-value was 17.599, and the p-value was <0.001, indicating a highly significant effect. The effect size was large (0.566). In summary, the analysis reveals that the variable “group” has a considerable influence on the dependent variables. Significant effects were observed for all examined variables. The effect sizes were generally moderate to large, suggesting that the variable “group” has a notable impact on these dependent variables.
Postoperative period
Table 6 presents the results of the multivariate test, which examines the effects of the variable “group” on the dependent variables in the postoperative period. The Pillai’s trace test statistic yielded a significant result (F = 4.824, df = 6.000, error df = 52.000, p = 0.001), indicating a statistically significant multivariate effect. The effect size, as measured by partial eta squared, was moderate (0.358). Similarly, the Wilks’ lambda test statistic yielded a significant result (F = 6.612, df = 6.000, error df = 50.000, p < 0.001), further supporting the presence of a significant multivariate effect. The effect size was moderate (0.442). The Hotelling’s trace test statistic was found to be significant (F = 8.531, df = 6.000, error df = 48.000, p < 0.001), with a moderate effect size (0.516). Finally, the Roy’s largest root test statistic yielded a highly significant result (F = 18.137, df = 3.000, error df = 26.000, p < 0.001), indicating a substantial multivariate effect of the variable “group” on the dependent variables. The effect size was large (0.677). In conclusion, the results of the multivariate test demonstrate that the variable “group” has a significant and meaningful multivariate effect on the dependent variables. The observed effect sizes were generally moderate to large, indicating a notable impact of the variable “group” on the dependent variables.
Table 7 presents the results of the analysis for the between-subject effects, examining the effects of the variable “group” on the dependent variables. With regard to the dependent variable “oxygen saturation”, the Type III sum of squares was 130.200, while the mean square was 65.100. The F-value was 4.929, and the p-value was 0.015, indicating a statistically significant result. The effect size, as measured by partial eta squared, was moderate (0.267). Regarding the dependent variable “pulse rate”, the Type III sum of squares was 534.067, and the mean square was 267.033. The F-value was 4.575, and the p-value was 0.019, indicating a statistically significant effect. The effect size was considered moderate (0.253). With regard to the dependent variable “FIS”, the Type III sum of squares was 34.200, and the mean square was 17.100. The F-value was 13.383, and the p-value was <0.001, indicating a highly significant effect. The effect size was large (0.498). In summary, the analysis reveals that the variable “group” has a significant influence on the dependent variables. The effect sizes are generally moderate to large, suggesting that the variable “group” has a notable impact on these dependent variables.
Discussion
Dental anxiety originates from the sight of an anxious stimulus, which can be inculcated during childhood and subsequently propagated into adulthood. The dentist should address the root cause in order to provide an uncompromised treatment.15 A variety of methods have been employed for behavior management in children, including behavior shaping and positive reinforcement, tell-show-do, enhancing control, distraction, systemic desensitization, and modeling.16 The United Nations General Assembly adopted June 21st as the International Day of Yoga.17 The yogic relaxation technique represents a less invasive alternative behavior management technique due to its novel approach and ease of application.
The concrete operational stage of cognitive development is observed in children between the ages of 7 and 11. As the study required the patients to understand and reproduce various yogic relaxation techniques, the age group of 6–12 years was selected for the study.18
Based on the learning theory of behavior management, the tell-show-do technique prepares the child to overcome their fear. It reduces uncertainty, alleviates anticipatory anxiety, and facilitates patient education and behavior guidance.19, 20
Modeling is based on learned experience and observation of the visual impulses, which can be conducted through a live model or delivered through videos.21, 22 Live modeling is an essential alternative to the tell-show-do technique. Using parents as a live model is a tangible technique in dental clinical practice.23, 24 The tell-show-do and live modeling techniques have been shown to reduce anxiety in pediatric patients.23, 25, 26, 27, 28 Thus, these techniques have been selected as the standard comparison methods for the yogic relaxation technique.
Yoga is used as an alternative treatment modality in various fields of medicine, including oncology. It improves the psychological well-being in adult cancer patients.29, 30, 31, 32 In the pediatric population, yoga has been shown to mitigate the emotional and psychological challenges associated with chemotherapy and radiotherapy.33, 34
Yoga, along with visual modeling and pedagogy in mass education has been demonstrated to enhance the learning capability of children with autism spectrum disorder (ASD) in tooth brushing.35 It also enhances motor activity and imitation skills, 36 and improves attention and hyperactivity among ASD children.37 Additionally, it has been shown to reduce stress, anxiety and depression,38, 39, 40 and to improve attentional control and heart rate variability.41, 42 The practice of yoga and mindfulness improves the socio-emotional function and regulatory skills, such as behavioral self-regulation and executive function.43 Yoga has an anxiolytic effect in the management of adult patients undergoing endodontic treatment.44
Yoga modulates breathing activity, balances the sympathetic and parasympathetic systems, reduces the workload on the heart and the oxygen requirement, decreases the pulse rate, increases oxygen saturation, and induces relaxation.45
The pulse rate can be considered a psychological marker of anticipatory anxiety.46, 47 Fear and anxiety are triggered by breathlessness, a dysfunctional respiratory control mechanism, hypoxia, and hypocapnia.48 Stress can alter the respiratory rate pattern, influencing the oxygen saturation and partial pressure of carbon dioxide in the blood.49 The FIS is a reliable method for evaluating children’s dental anxiety.50, 51 The FLACC is accurate and sensitive in measuring procedure pain.52, 53 Hence, the abovementioned parameters were selected to assess the anxiety and pain levels during the course of the study.
In the study, during both the intraoperative and postoperative periods, oxygen saturation was significantly higher in the yogic relaxation technique group. Additionally, the yogic relaxation technique group exhibited lower pulse rates, FIS and FLACC scores compared to the tell-show-do and modeling technique groups. The yogic relaxation technique was implemented through the use of 3 different yoga poses; however, no subgroups were designated to assess the efficacy of individual poses. To the best of our knowledge, our study was the first to use a yogic relaxation technique as a behavior modification technique among pediatric patients in a dental setting.
Conclusions
The practice of yoga has a positive influence on the general health of the individual. Various behavior management techniques, including the tell-show-do technique, have been know to reduce dental anxiety in children. Our study has shown the anxiolytic effect of the yogic relaxation technique in comparison to the tell-show-do and modeling techniques. Thus, the yogic relaxation technique can be considered an alternative behavioral modification technique for reducing dental anxiety among pediatric patients.
Ethics approval and consent to participate
The study was approved by the ethical clearance board of Chettinad Academy of Research and Education, Chennai, India (approval No. IHEC-I/1302/22).
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.