Abstract
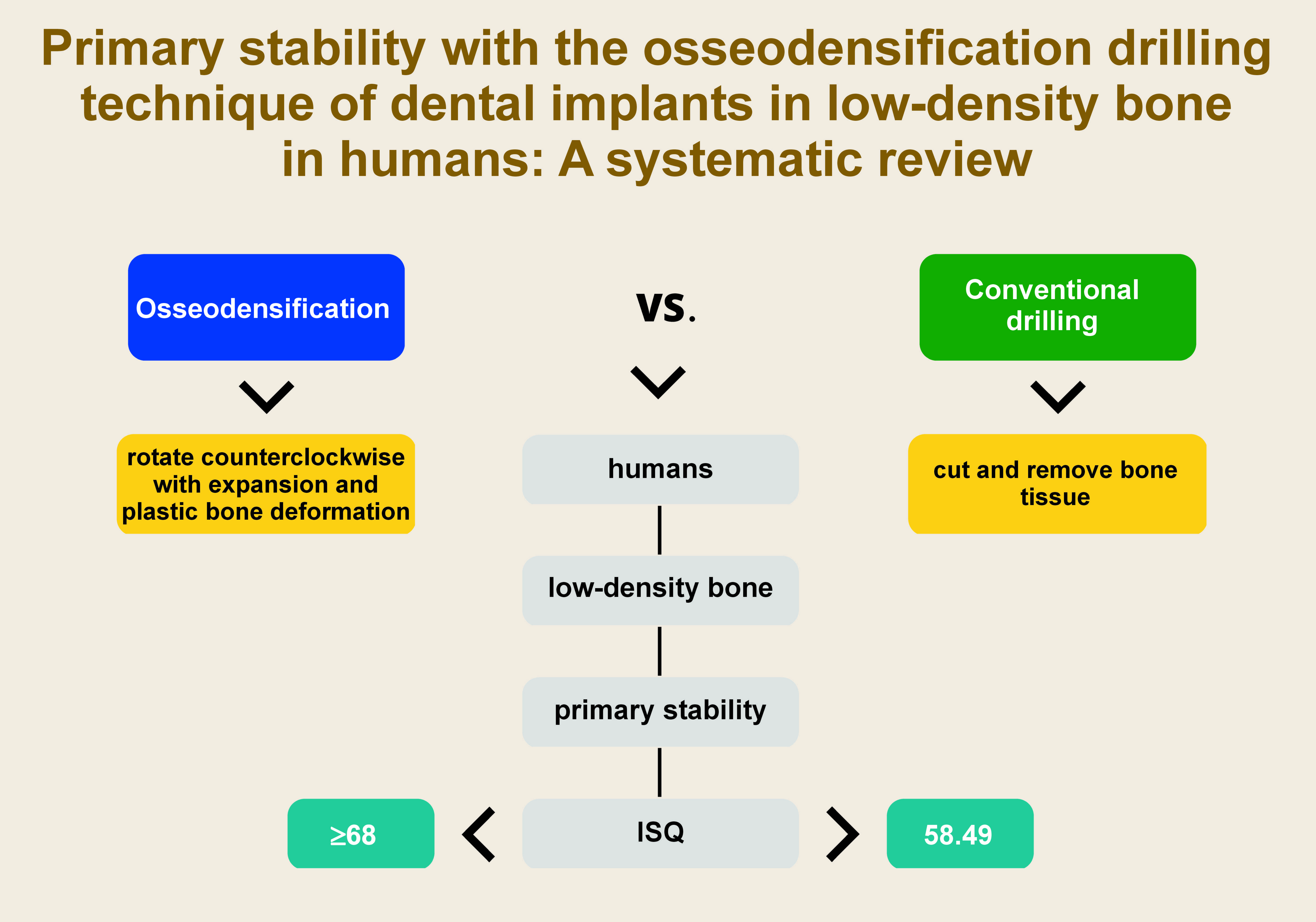
Currently, a new non-subtractive drilling technique, called osseodensification (OD), has been developed. It involves using specially designed drills with large negative cutting angles that rotate counterclockwise, causing expansion through plastic bone deformation, thus compacting the autologous bone to the osteotomy walls, which improves the primary stability of the implant.
The present systematic review aimed to determine whether the OD technique can increase the primary stability of dental implants in the posterior maxilla region as compared to the conventional drilling (CD) technique.
Five databases were searched up to June 30, 2022. The inclusion criteria embraced observational clinical studies, randomized and non-randomized controlled trials, human studies in vivo, comparing OD and CD, with the measurement of the primary stability of implants in the posterior maxilla region by means of the implant stability quotient (ISQ). The tools used to assess the risk of bias were RoB 2 and the Newcastle–Ottawa Scale (NOS).
Seven articles met the inclusion criteria, with 4 classified as having a low risk of bias and 3 with a moderate risk of bias. The OD technique consistently demonstrated an average ISQ value of 73 KHz across all studies, whereas CD yielded an average value of 58.49 kHz (p < 0.001 for 5 articles).
It can be concluded that in comparison with CD, OD improves primary stability at baseline in low-density bone, such as the maxilla.
Keywords: dental implant, primary stability, osseodensification, low-density bone
Introduction
Dental implants have become the first choice for replacing missing teeth due to the predictable results of the procedure.1 However, success depends mainly on the anchorage of dental implants in the surrounding bone, which is called osseointegration. The term was introduced by orthopedic surgeon and researcher Per-Ingvar Brånemark, who defined osseointegration as a direct and functional connection between the bone and the surface of a load-bearing implant at the microscopic level.2, 3, 4, 5
For osseointegration to occur, it is essential to achieve primary stability through the initial mechanical coupling of the implant with the cortical bone. Obtaining osseointegration depends on the shape of the implant, the surgical technique and bone density.5
Various protocols have been proposed to assess primary implant stability, such as Periotest® measurements, insertion torque assessment, experimental implant removal, or resonance frequency analysis (RFA).6
Modern RFA devices, such as the Osstell device (W&H Dentalwerk Bürmoos, Bürmoos, Austria), provide an assessment of the primary stability of dental implants. These devices measure the implant resonance frequency in kilohertz (kHz), allowing the implant stability quotient (ISQ) to be calculated.6
The ISQ scale comprises values from 0 to 100. The values are not distributed linearly; values below 60 kHz correspond to low stability, values between 60 kHz and 69 kHz indicate medium stability, and values above 70 kHz correspond to high stability. Values greater than 68 are considered predictive of successful osseointegration.6, 7, 8
According to Lekholm and Zarb, the oral cavity contains different types of bone classified by bone quality: Class 1 –almost exclusively homogeneous compact bone; Class 2 – wide, compact bone surrounding dense cancellous bone; Class 3 – thin cortex surrounding dense cancellous bone; and Class 4 – thin cortex surrounding sparse cancellous bone.9 Recent scientific research has shown implant failure rates for different bone types: 3.38% (Class 1); 3.13% (Class 2); 4.27% (Class 3); and 8.06% (Class 4), indicating that Class 4 bone has the highest failure rate.10 This type of bone is frequently found in the maxilla in the posterior area, which is considered a structure of low bone density, where a reduced success rate in the placement of dental implants has been demonstrated.11, 12
Generally, conventional drilling (CD) is used to prepare the implant bed. It involves using drills of different diameters and heights to cut and remove bone tissue.13 Currently, a new non-subtractive drilling technique, called osseodensification (OD), has been developed. It involves using specially designed drills with large negative cutting angles that rotate counterclockwise, causing expansion through plastic bone deformation, thus compacting the autologous bone to the osteotomy walls, which improves the primary stability of the implant.14, 15
The literature reports that OD brings promising and encouraging clinical results due to a significant increase in bone biomechanical properties as compared to CD, achieving high primary stability and a higher survival rate of dental implants in the short term; however, studies evaluating the success of OD have mostly been performed based on animal models and in vitro demonstrations.16, 17, 18
The purpose of the present study was to perform a systematic review addressing the following research question: Does the use of OD increase the primary stability of dental implants placed in the posterior maxilla region in humans as compared to CD?
Methods
The methodology used in this research adheres to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) 2020 statement.19
Eligibility, inclusion and exclusion criteria
The PICO framework was as follows: P – patients requiring implant placement; I – intervention (OD); C – comparison (CD); and O – outcome (ISQ).
The inclusion criteria comprised human studies in vivo, dental implants placed in the posterior maxilla region, studies comparing OD with CD, observational clinical studies (cases and controls), randomized and non-randomized controlled trials, and studies that measured the primary stability of dental implants with the use of ISQ.
The exclusion criteria comprised studies evaluating only OD, studies comparing OD with techniques other than CD, case reports, case reviews, review articles, systematic reviews, meta-analyses, case surveys, in vitro studies, studies conducted in animals or in synthetic sites (a dental typodont, or acrylic or plastic models), and studies that did not measure primary implant stability.
Sources of information
The search for information was conducted up to June 30, 2022, in 5 databases – PubMed via MEDLINE, Google Scholar, Cochrane, Scopus, and ScienceDirect.
Search strategy
An exhaustive bibliographic search was performed in the abovementioned databases to identify relevant articles published up to June 30, 2022, without limitations with regard to the language or the year of publication. The search strategies used keywords based on the PICO question, separated with the Boolean operator OR and combined with the Boolean operator AND. Additionally, gray literature was searched through the bibliographies of the articles included in this research.
The database search was carried out independently by two of the authors. The keywords used were: “dental implant”; “low density”; “implant”; “dental implants”; “dental implantation”; “endosseous implants”; “osseodensification”; “osseodensification osteotomy”; “versah drills”; “versah burs”; “osteotomy”; “implant osteotomy”; “drill”; “regular drilling”; “conventional drilling”; “peri-implant marginal bone loss”; “marginal bone loss”; “crestal bone loss”; “bone loss”; “bone remodeling”; and “primary stability” (Table 1).
Study selection
The studies identified by the search were independently examined in duplicate by two investigators to assess their adherence to the inclusion criteria based on titles and abstracts. Articles on which both authors agreed, achieving a kappa concordance value of 0.937, were selected.
The full text of the selected articles was read to evaluate their titles and abstracts. Then, the references listed in all the selected articles were reviewed manually and compared with the inclusion criteria. Any disagreement regarding inclusion was resolved through discussion with a third author.
Scientific articles that met the inclusion criteria were selected and read in full text to evaluate the methodological quality of observational clinical studies and randomized and non-randomized controlled clinical trials comparing OD and CD in living humans. The assessment focused on the primary stability of dental implants placed in the maxilla, with low bone density, in terms of ISQ values.
Data extraction
A data extraction protocol was defined; the form was elaborated in Excel (Office Excel 2011 software; Microsoft Corporation, Redmond, USA) and included authors, year, study design, number of participants, number of implants placed, and ISQ results for each technique used.
Risk of bias assessment for individual studies
Version 2 of the Cochrane risk-of-bias tool (RoB 2) was used to assess the risk of bias in randomized clinical trials (RCTs).20 The Newcastle–Ottawa Scale (NOS) was used to assess the risk of bias in non-randomized studies, including observational studies.21 The 2 tools rated the included articles as having a low, moderate or high risk of bias.
Results
Search and selection
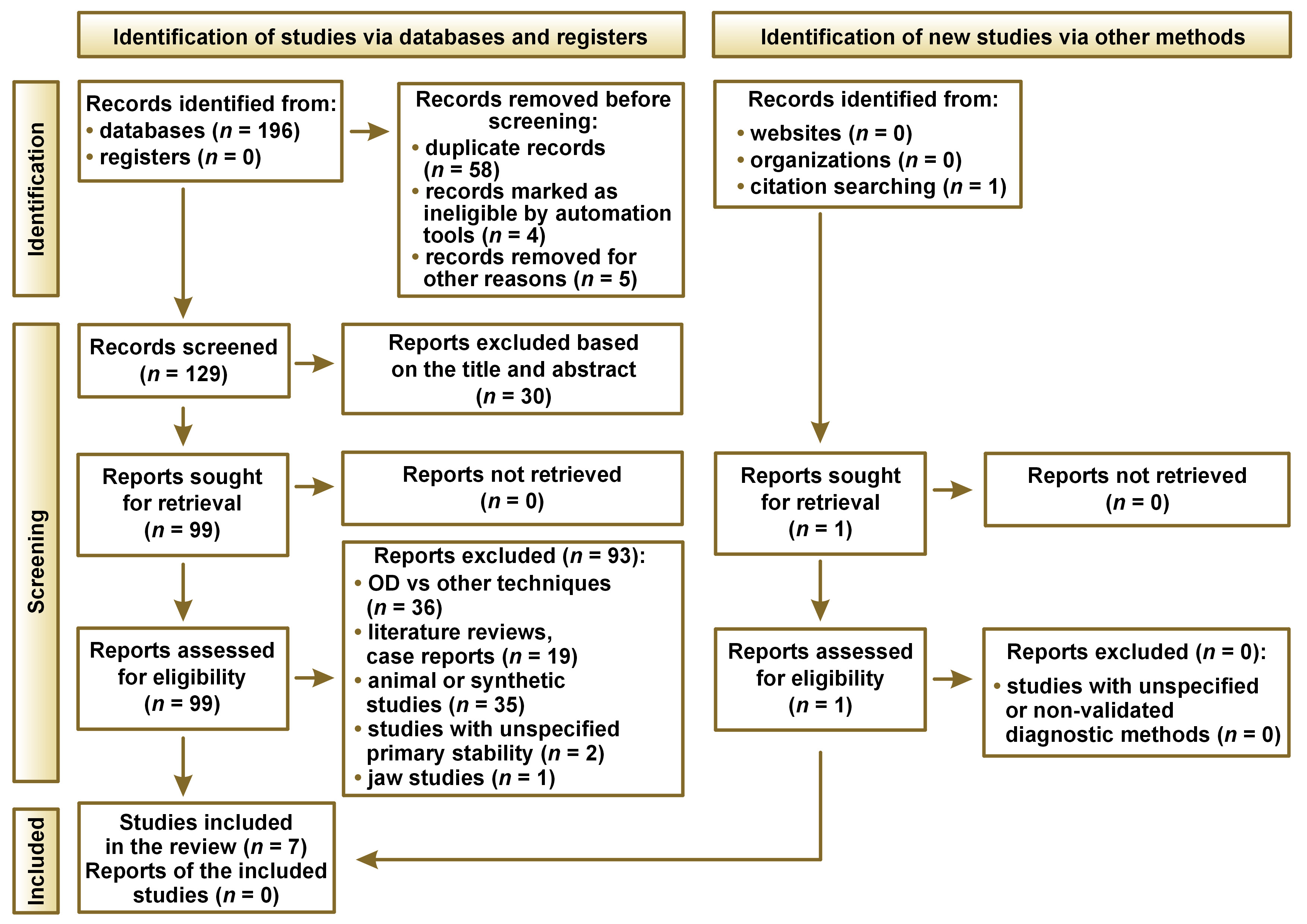
The systematic search yielded a total of 196 articles; after filtering out duplicate articles and articles without access, 129 were obtained; 30 were discarded based on the title and abstract. According to the inclusion and exclusion criteria, 93 articles were eliminated. Through the manual search of the bibliography of each article and relevant reviews, 1 article was included, resulting in a total of 7 articles included in the present review.
The PRISMA 2020 flowchart summarizing the selection process is shown in Figure 1.
Comparison of the drilling techniques
In the included articles, the OD technique presented ISQ values greater than 68 kHz, which is the minimum value to achieve successful osseointegration, as compared to the CD technique with an average ISQ value of 58.49 kHz.7, 11, 15, 17, 22, 23, 24 Five articles showed p < 0.001 in this respect7, 15, 17, 22, 24 and in 2 articles, the p-value was >0.001.11, 23 In addition, it must be taken into account that OD is a technique that uses almost the same protocol with regard to the drilling speed as CD, the difference being that the direction is counterclockwise. All this shows predictable parameters for successful osseointegration in comparison with CD. It should also be mentioned that in most of the included studies, the patients were between 50 and 60 years of age (Table 2).
Risk of bias for individual studies
Among the 7 studies included in the systematic review, 4 were assessed to have a low risk of bias, while 3 had a moderate risk of bias. None of the articles was found to have a high risk of bias. The moderate risk of bias was attributed to the randomization process and the selection of the reported outcomes (Table 3 and Table 4).
Discussion
The primary or initial stability of dental implants results from the mechanical union with the peri-implant bone, and is considered a primordial factor in achieving secondary stability with subsequent osseointegration.23 It is a priority to employ an adequate surgical technique to improve the primary stability of the implant and to adapt to the existing protocols to achieve successful osseointegration, even more so in cases where bone quality is not optimal.25, 26
Therefore, the purpose of this study was to conduct a systematic review addressing the research question: Does the use of OD increase the primary stability of dental implants placed in the posterior maxilla region in humans as compared to CD?
An alternative to CD has been proposed, since this conventional technique eliminates bone particles in the surgical act, whereas OD keeps bone particles compact in the osteotomy wall.14 This offers mechanical and biological advantages in terms of intimate contact between the implant and the bone because of residual bone fragments on the implant surface and improved bone healing due to the nucleation of osteoblasts in the instrumented bone.27, 28, 29
Furthermore, a major advantage of the OD approach is the ability, in numerous scenarios, to circumvent the need for bone and membrane grafts. This not only reduces surgical invasiveness and significantly shortens the healing time, but also helps in minimizing peri-implant inflammation, which is often greater in implants placed in the native bone. From this point of view, it is necessary to underline the importance of keeping the level of peri-implant bone inflammation as limited as possible, as emphasized by Guarnieri et al.30, 31
Numerous surgical procedures have been suggested to avoid or decrease bone loss during implant placement in low-density bone, and to improve the primary stability of the implant and bone quality. However, few investigators recommended decreasing the osteotomy site with regard to the implant diameter by approx. 10% to decrease bone stress and improve primary implant stability. The osteotomy site decreased by more than 10% does not provide any mechanical benefit. However, the OD approach increases the primary stability of the implant.7, 8, 9, 10
Human studies can be extrapolated to daily clinical practice; therefore, it should be clarified that this review is the first to focus on primary stability in low-density bone. Several authors have demonstrated favorable and predictable results with OD as compared to CD, i.a., Abdelwahab et al.22 and Kothayer et al.,24 who mentioned superior primary stability with statistically significant values (p < 0.001).
Furthermore, the advantages of OD over CD were mentioned by Mello-Machado et al., who did not need to increase the drilling diameter for osteotomy, allowing the placement of a 3.8-millimeter implant in an ideal space for an implant with a 3.5-millimeter diameter.15 Similarly, Al Ahmari evidenced an increase in peri-implant bone density when using OD as compared to CD.11 These results are associated with the elastic compression of the bone tissue toward the implant due to the recovery effect of the implant as a consequence of OD drilling. In this way, the implant compresses the bone and, at the same time, the bone compresses the implant inversely.14
The dimensions of implants vary in each technique. Ibrahim et al. showed the superiority of OD in terms of primary stability as compared to CD with p < 0.001, but the implants used for CD were 3.8 mm and for OD 5.0 mm in diameter.17 Conversely, Bergamo et al. evaluated the primary stability of 150 implants with a statistically superior ISQ in OD at p < 0.001; however, they did not achieve the same results with short implants.7
The results of the present systematic review demonstrated an average ISQ value of 73 kHz for the OD technique, which is higher than the minimum value to achieve successful osseointegration (68 kHz). The CD technique obtained an average ISQ value of 58.49 kHz. Therefore, OD, due to its non-subtractive nature, may be useful in sites with a larger trabecular bone volume, such as the maxilla, thus improving bone mineral density and potentially accelerating osseointegration due to elastic recovery.32 Yet, 2 articles in this review did not show immediate statistical significance for dental implant placement with OD, i.e., by Al Ahmari, with a mean ISQ value of 50.57 ±11.23 (p > 0.001),11 and by Sultana et al., with an ISQ value of 65.6 (p > 0.05).23
Future prospective research on the use of the OD technique for immediate loading is recommended to achieve faster rehabilitation of stomatognathic system functions without compromising dental implant success, as mentioned by Krawiec et al.33 Similarly, changes at the peri-implant bone level may occur during healing, as noted by Abarno et al.,34 where dental implants bear tension and stress upon prosthetic loading. Therefore, the results obtained with regard to primary stability can lead to studies on the predictability of OD in relation to the abovementioned events.
Limitations
As a limitation of the present study, it should be noted that there were few studies involving human subjects, primarily due to bioethical concerns and the fact that OD is a relatively new technique developed in the last decade. Therefore, only limited data could be obtained regarding the primary stability of implants placed in the posterior maxilla region.
Conclusions
The obtained data showed significantly higher ISQ values for primary stability in the posterior maxilla region, favoring OD over CD. However, these results should be interpreted cautiously due to the limited evidence available on the use of this technique in humans.
Registration
The study protocol was registered at https://inplasy.com under the number 202290066.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets supporting the findings of the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.