Abstract
Background. Although the microplate system is commonly used for the treatment of maxillofacial fractures, its use in the fixation of mandibular fractures is not widely accepted.
Objectives. The study aimed to evaluate and compare the efficacy of microplates and miniplates in osteosynthesis for the internal fixation of undisplaced and minimally displaced anterior mandibular fractures.
Material and methods. A total of 40 patients diagnosed with undisplaced or minimally displaced symphyseal and parasymphyseal fractures were randomly assigned to 2 study groups (group A and group B). Patients in group A (microplate group) were treated with two 0.8-mm microplates, whereas patients in group B (miniplate group) received two 2.0-mm miniplates. Bite force values were recorded in 30 healthy individuals (control group) to establish baseline values. Postoperative bite force values were recorded at various intervals and compared between the study groups and the control group.
Results. Both groups demonstrated a progressive improvement in the bite force. However, the bite force values recorded at the 2nd, 4th and 6th postoperative weeks were comparatively lower in the microplate group. At the six-week follow-up, the bite force values were lower in both study groups in comparison to the control group. There were no differences in the incidence of postoperative complications between the study groups.
Conclusions. The use of microplates in the management of undisplaced or minimally displaced anterior mandibular fractures results in a reduction in the recovery of biting force in comparison to the conventional miniplate system.
Keywords: traumatology, maxillofacial, trauma, fracture fixation
Introduction
The etiology of facial bone fractures can be attributed to a number of factors, including road traffic accidents, interpersonal violence, falls, and sport-related injuries.1 Maxillofacial and mandibular injuries can cause facial disfigurement and functional impairment.2 The fundamental principles of treating mandibular fractures include proper anatomical reduction, restoration of the premorbid occlusion, and appropriate fixation until stable osseointegration. Open reduction and internal fixation are the main treatment modalities for managing mandibular fractures. Semi-rigid fixation techniques include methods such as intraosseous wiring, which allows intersegmental movement across the fracture line. However, this often results in delayed union, malunion, or non-union. Rigid fixation helps overcome these drawbacks by preventing intersegmental movement under active load and includes the use of reconstruction plates, miniplates, lag screws, and compression plates.
Luhr developed the microplate fixation system, revolutionizing the operative management of maxillofacial fractures.3 The system was designed to reduce the size of bone plates and limit the hardware, with the intention of encouraging close adjustment at the fracture site and minimizing periosteal stripping. In comparison to miniplates, microplates are thinner and more commonly used in the fixation of midface fractures. Microplates have been considered in the treatment of mandibular fractures because their use is less traumatic to soft tissue, requires less periosteal tissue reflection, minimum tissue interference, and easier contouring that provides three-dimensional (3D) geometric stability. Furthermore, reduced palpation and thermal conduction due to the thin cutaneous cover improve patient comfort.4
Objectives
The present prospective clinical study aimed to evaluate the efficacy of microplates for managing undisplaced or minimally displaced anterior mandibular fractures, and to compare them with miniplate osteosynthesis in terms of occlusal stability, fracture fixation and biting efficiency using a bite force measurement device.
Material and methods
This prospective randomized clinical study was conducted in patients aged 18–35 years who required open reduction and internal fixation for undisplaced or minimally displaced symphyseal or parasymphyseal fractures. A total of 70 patients were enrolled in the study, including 30 healthy individuals as a control group and a study group of 40 patients with undisplaced or minimally displaced anterior mandibular fractures. The study was approved by the Krishna Institute of Medical Sciences Ethics Committee (approval No. KIMSDU/IEC/02/2018). Patients who expressed willingness to participate and who provided informed consent were included in the study. The patients with mandibular fractures (study group) were randomly divided into group A, treated with 2 microplates (0.8-mm thick) and 8 microscrews (1.5 mm × 8 mm and 1.5 mm × 10 mm), and group B, treated with 2 miniplates (2.0 mm) and 8 miniscrews (2 mm × 8 mm and 2 mm × 10 mm), according to an odd-even formula. Each study group consisted of 20 patients. Thirty healthy individuals whose age and gender matched the study group were recruited for the control group.
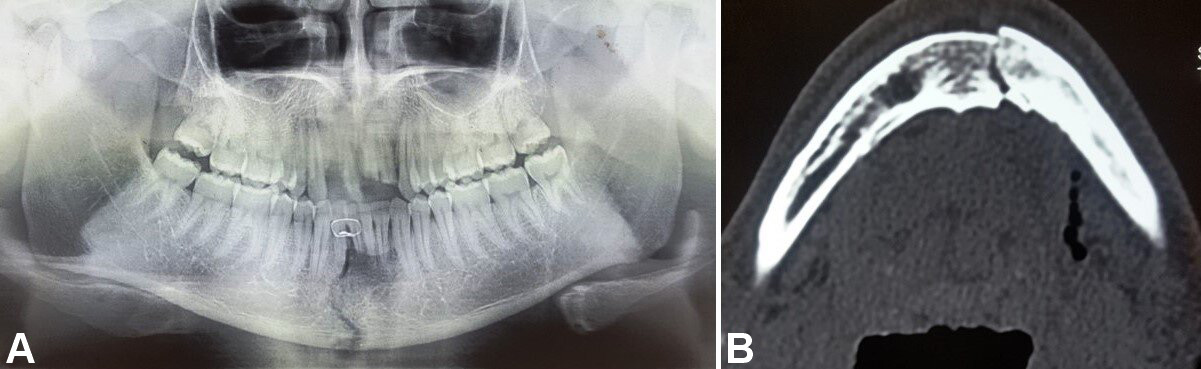
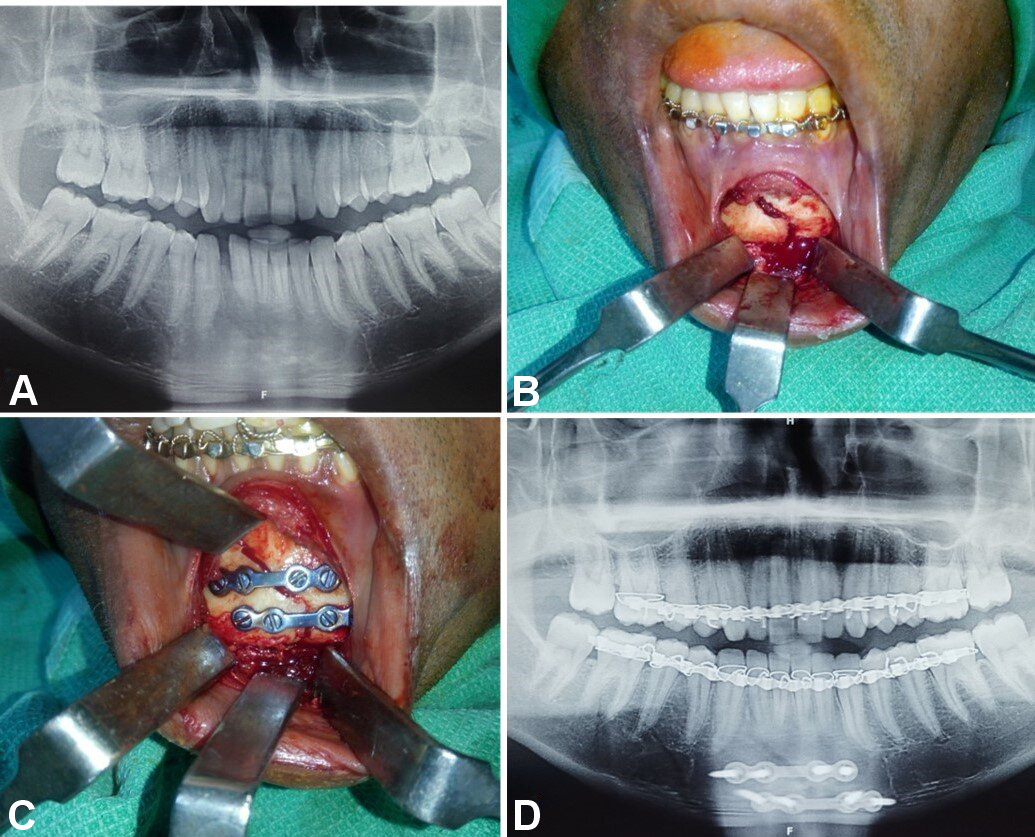
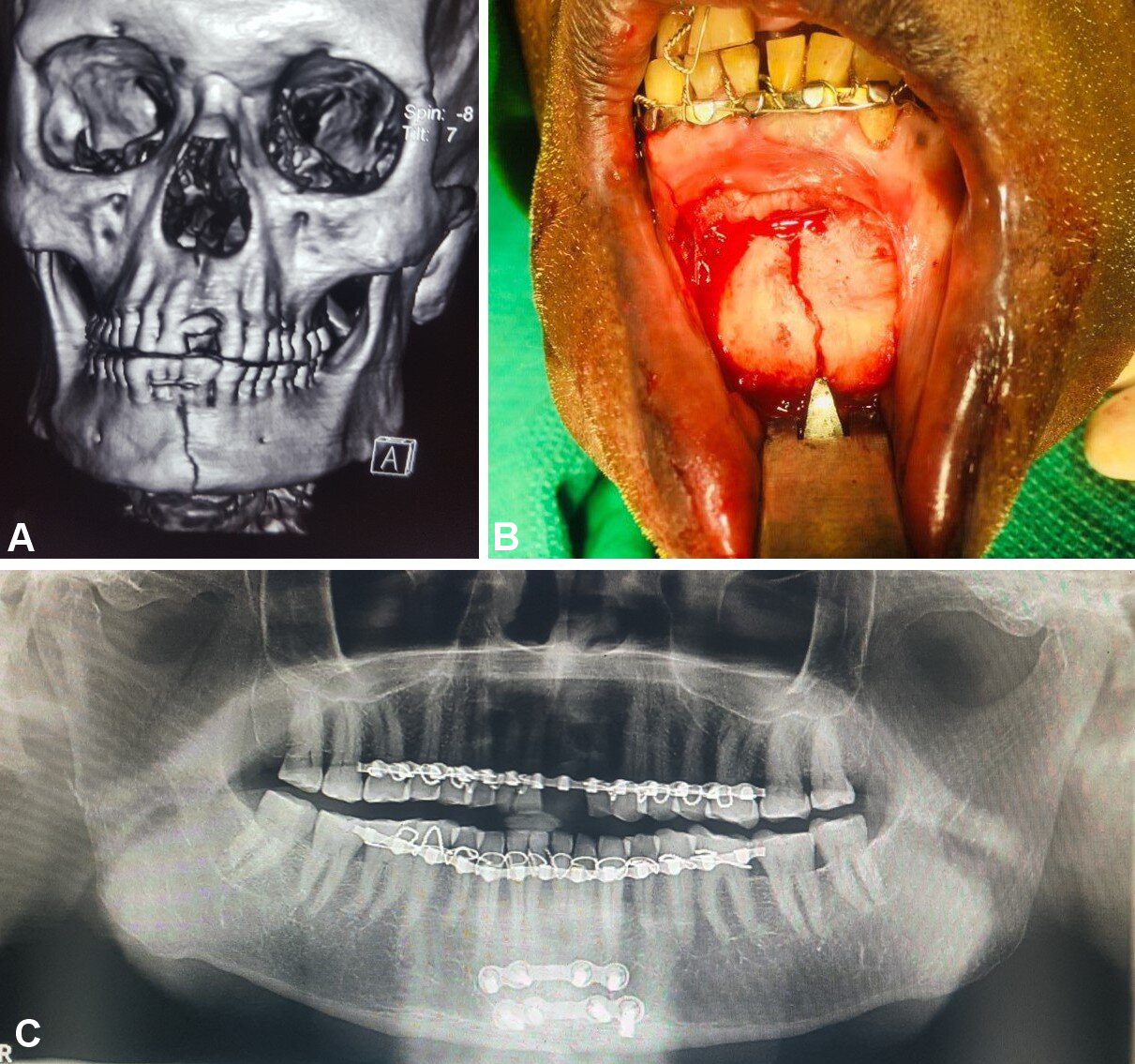
Patients with comminuted mandibular fractures, concomitant midface and dentoalveolar fractures, infected fractures, partial or complete edentulism, and systemic diseases were excluded from the study. Detailed preoperative medical and clinical examinations were conducted. The diagnosis of undisplaced or minimally displaced symphyseal or parasymphyseal fractures was based on clinical and radiographic assessments. Orthopantomograms were used to evaluate mandibular lower border displacement, with displacements of less than 5 mm included in the study (Figure 1). Advanced diagnostic techniques, including low-dose radiation and 3D assessments using computed tomography (CT), cone beam computed tomography and magnetic resonance imaging, facilitate comprehensive evaluation of head and neck disorders, including the assessment of both soft and hard tissue injuries.5, 6, 7 Therefore, CT with 3D reconstruction of the face was performed, with fractures exhibiting bucco-lingual overlap of less than 5 mm included in the study (Figure 1).
Surgical procedure
Following the pre-anesthetic check-up, each patient underwent surgery under general anesthesia with nasal intubation. The standard surgical preparation and draping were performed under strict aseptic conditions. Local anesthesia (2% lidocaine with 1:200,000 adrenaline) was injected at the fracture site. Maxillary and mandibular arch bars were placed for intermaxillary fixation. An intraoral mandibular incision was made according to the location of the fracture, and a full-thickness mucoperiosteal flap was elevated, retracting the tissues. Cautery was occasionally used during dissection to maintain a bloodless field. The fracture segments were adequately exposed, followed by anatomical reduction and intermaxillary fixation to achieve passive occlusion.
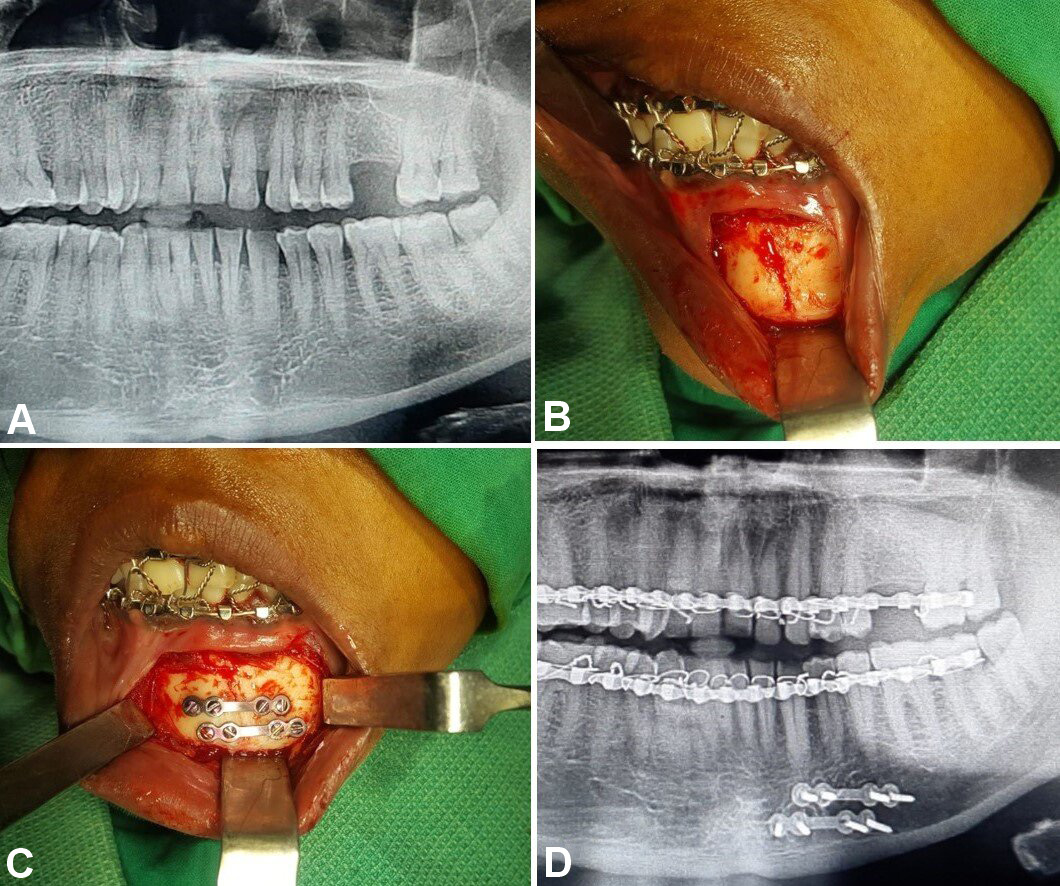
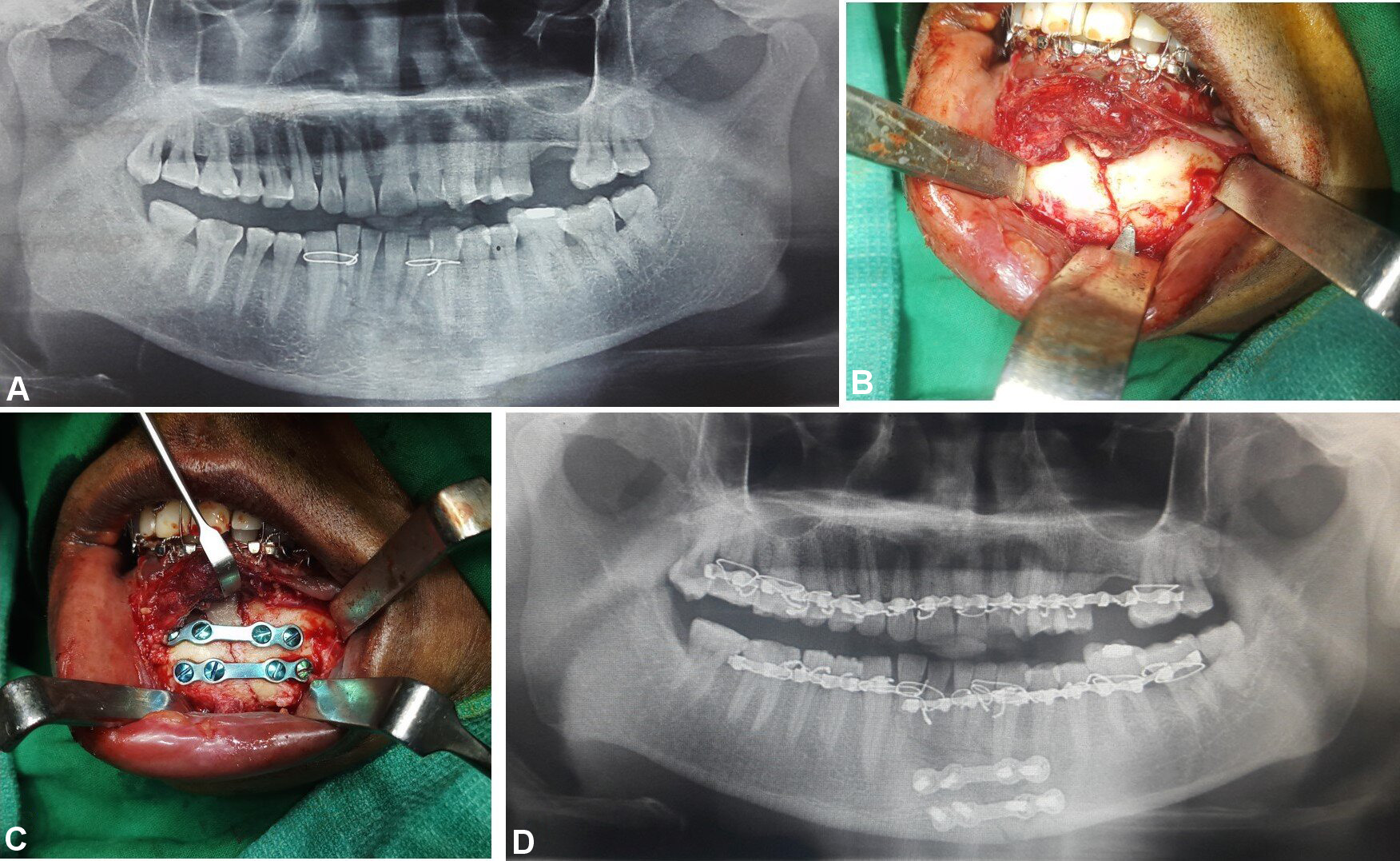
In group A, fixation was performed using 2 titanium microplates (0.8-mm, 4-hole design with a gap) and 8 microscrews (1.5 mm × 8 mm and 1.5 mm × 10 mm), which were placed subapically and at the inferior border of the mandible according to Champy’s lines of osteosynthesis (Figure 2, Figure 3, Figure 4).
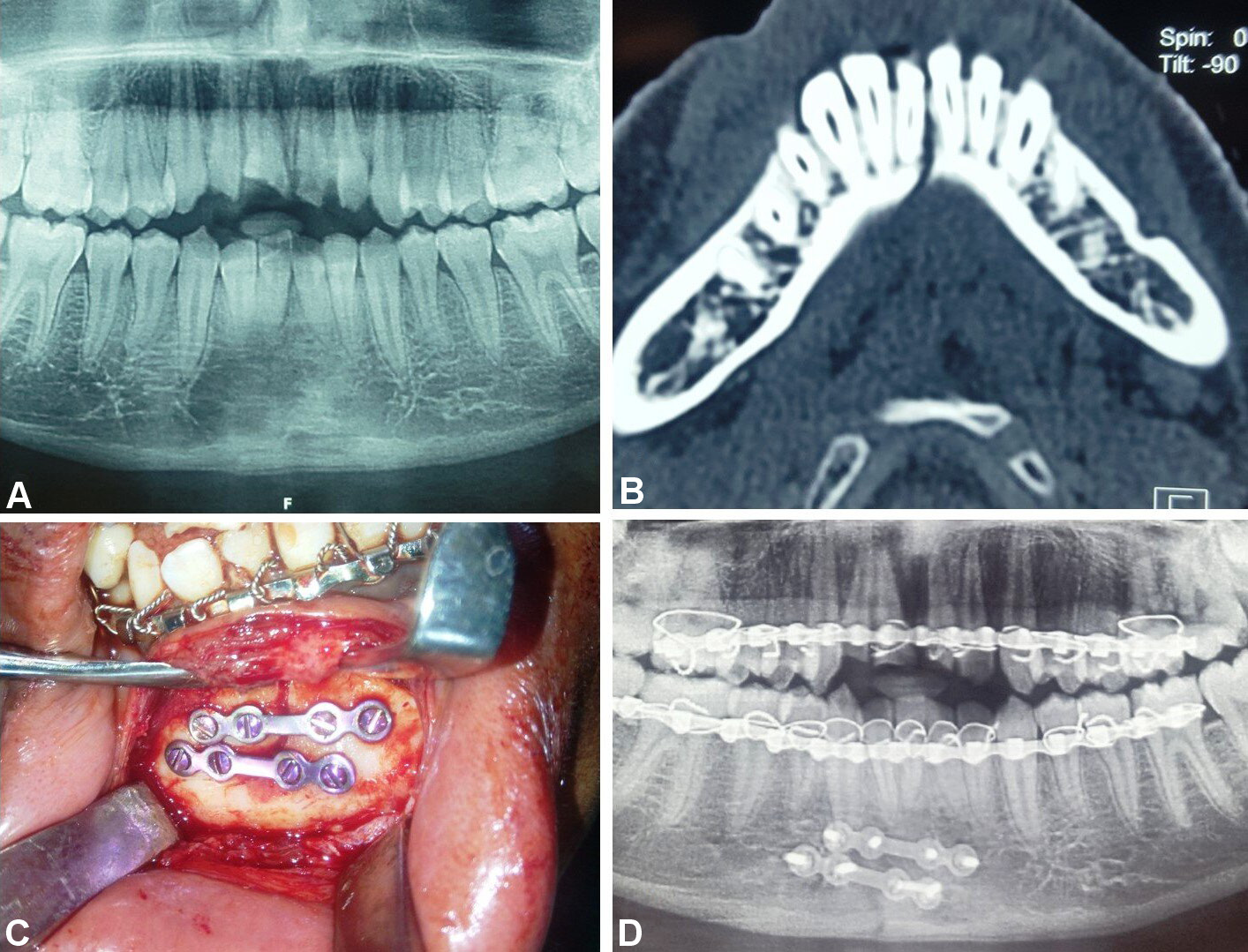
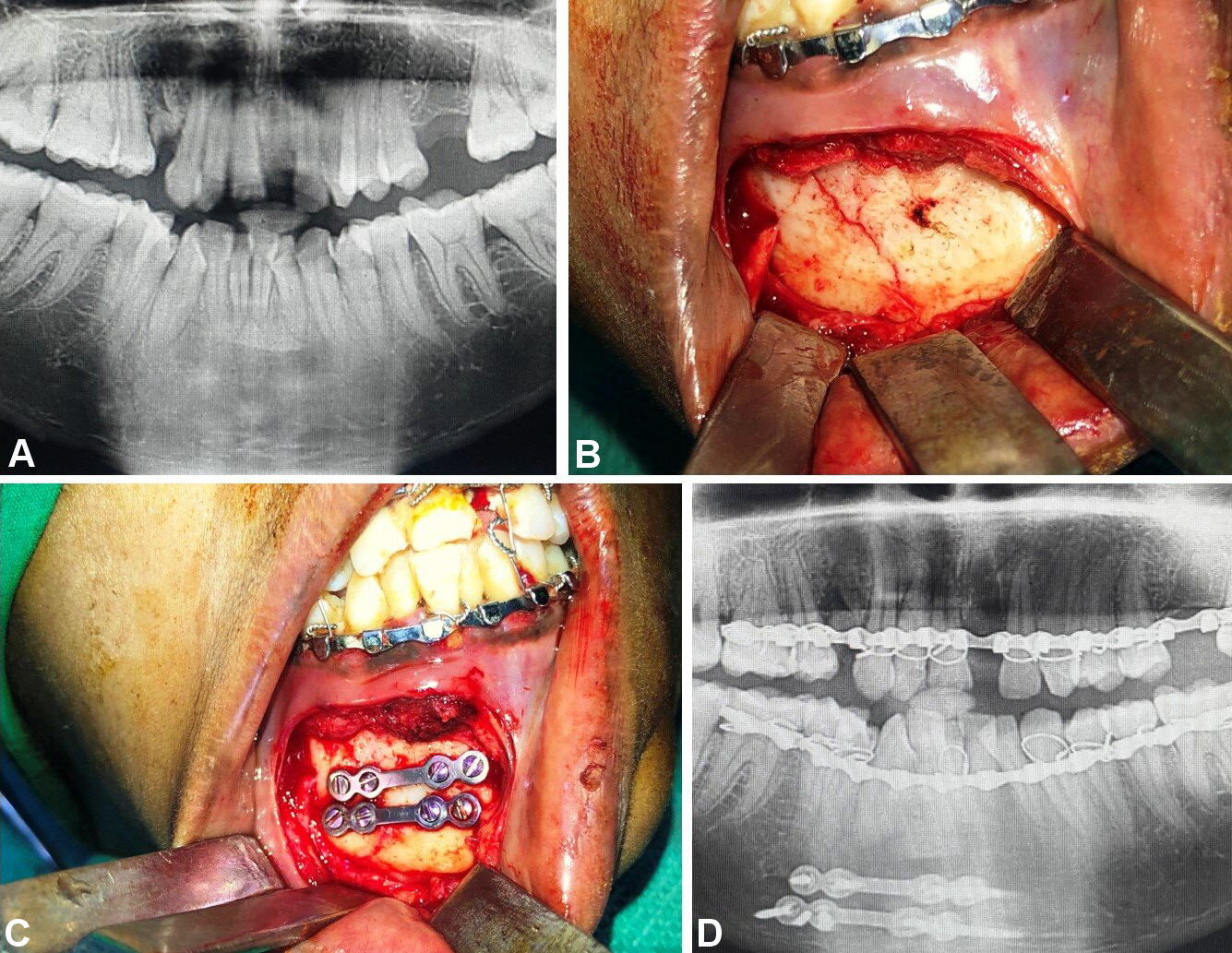
In group B, fixation was conducted using 2 titanium miniplates (2.0-mm, 4-hole design with a gap) and 8 miniscrews (2 mm × 8 mm and 2 mm × 10 mm), which were positioned subapically and at the inferior border of the mandible according to Champy’s lines of osteosynthesis (Figure 5, Figure 6, Figure 7).
Following the fixation procedure, the intermaxillary fixation was removed, and the occlusion was checked passively. The wound was closed using 3-0 absorbable Vicryl sutures in a continuous locking pattern for all patients. In accordance with the established trauma protocol, perioperative antibiotics and analgesics were administered. The surgical technique was identical for both groups and was performed by the same operating surgeon. All patients received postoperative antibiotic coverage for 5 days and were advised to consume a liquid and semisolid diet for 2 to 3 weeks. The subjects were instructed to rinse frequently with chlorhexidine mouthwash. Patients were scheduled for follow-up assessments at postoperative weeks 1, 2, 4, and 6. The parameters assessed included the bite force, occlusal discrepancy, segment mobility, plate integrity, and fracture site infection.
Bite force measurements were recorded using a digital bite force recorder (HARIOM Electronics, Vadodara, India). In the study groups, the bite force was measured at the incisors, right molars and left molars before surgery and at 1, 2, 4, and 6 weeks after surgery. A single bite force measurement was recorded for the control group at the incisors, right molars and left molars in a similar manner. The data was tabulated and analyzed statistically using unpaired t-tests and analysis of variance (ANOVA) with Tukey’s post hoc tests.
Results
A total of 70 patients were enrolled in the study, comprising 30 healthy individuals (control group) and 40 patients with undisplaced or minimally displaced anterior mandibular fractures (groups A and B). In the control group, 16 individuals were male and 14 were female. In study group A, 14 of the 20 patients were male and 6 were female, whereas in group B, 16 of the 20 patients were male and 4 were female. There was no statistically significant difference observed in sex distribution between the study and control groups (p = 0.684).
The age of the healthy individuals in the control group ranged from 19 to 35 years, with a mean of 27.17 years. In group A, the mean age was 27.50 years (range: 18–35 years), and in group B, it was 27.55 years (range: 19–35 years). No statistically significant difference was observed in age distribution among the 3 groups (p = 0.134).
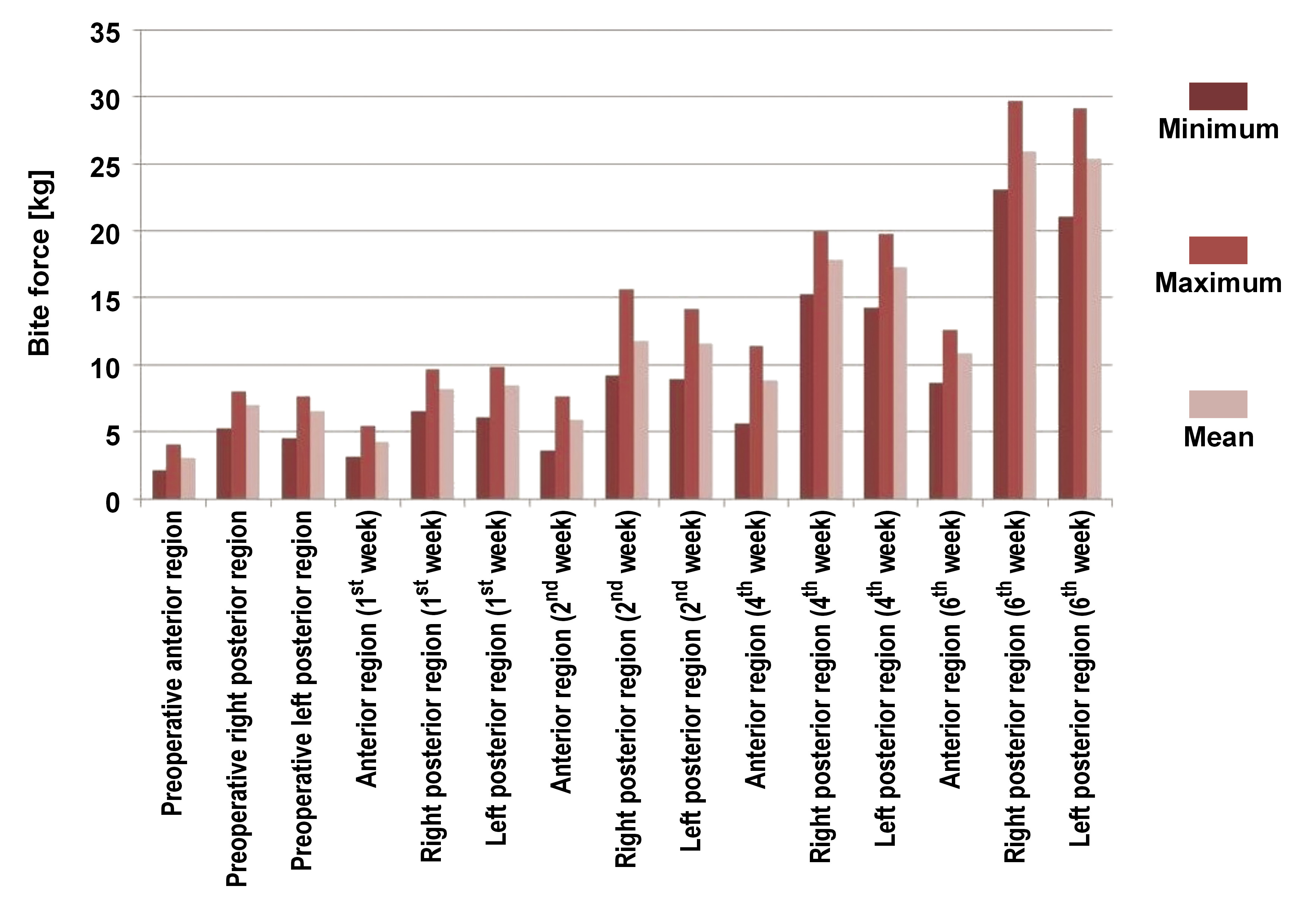
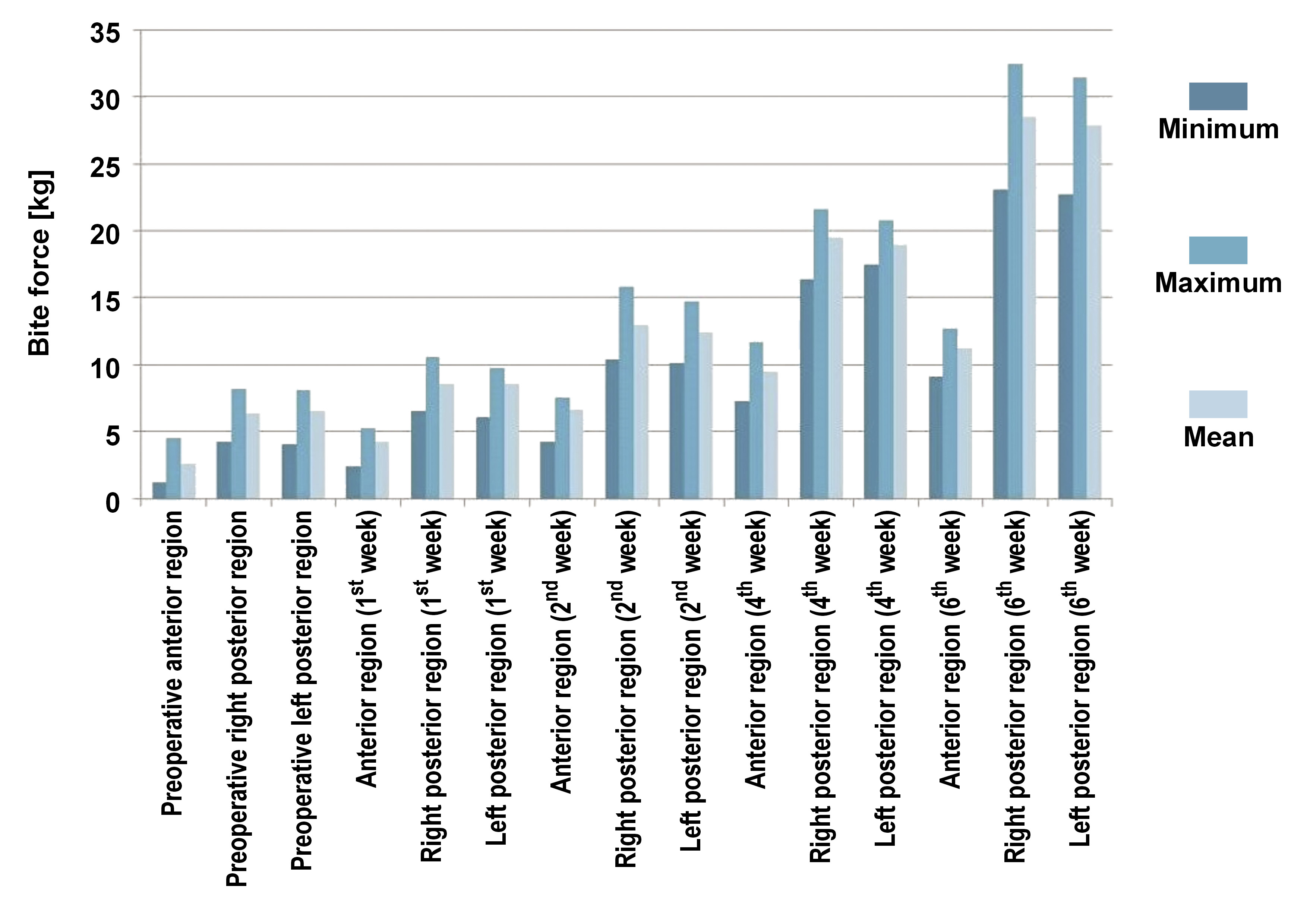
A comparison of the bite force between study groups A and B was performed using unpaired t-tests at various time intervals (Figure 8, Figure 9). Preoperatively, in group A, the mean bite forces at the anterior, right posterior and left posterior regions were 3.08 kg, 6.97 kg and 6.58 kg, respectively. In group B, the mean bite forces at the anterior, right posterior and left posterior regions were 2.55 kg, 6.35 kg and 6.50 kg, respectively. A statistically significant difference was identified in the preoperative comparison of the anterior bite force between group A and group B (p = 0.014), with a mean difference of 0.534 kg. The mean differences at the right posterior (0.621 kg) and left posterior (0.065 kg) regions were found to be insignificant (p = 0.051 and p = 0.822, respectively).
After the 1st postoperative week, the mean bite force at the anterior region for group A was 4.22 kg, while the mean bite force at the right and left posterior regions was 8.18 kg and 8.50 kg, respectively. In contrast, in group B, the mean bite force at the anterior region was 4.20 kg, and at the right and left posterior regions it was 8.56 kg and 8.56 kg, respectively. The mean differences between group A and group B for the anterior, right posterior and left posterior regions were 0.017 kg, −0.378 kg and −0.665 kg, respectively. These differences were found to be statistically insignificant (p = 0.943, p = 0.257 and p = 0.835).
After the 2nd postoperative week, the mean bite force in group A was 5.90 kg at the anterior region, 11.70 kg at the right posterior region and 11.60 kg at the left posterior region. In contrast, in group B, it was 6.61 kg at the anterior region, 13.02 kg at the right posterior region and 12.40 kg at the left posterior region. The mean difference between group A and group B for the right posterior region was −1.264 kg, which was statistically significant (p = 0.021). However, the mean differences between group A and group B for the anterior (−0.709 kg) and left posterior regions (−0.823 kg) were insignificant (p = 0.059 and p = 0.080, respectively).
After the 4th postoperative week, the mean bite forces in group A at the anterior, right posterior and left posterior regions were 8.82 kg, 17.80 kg and 17.30 kg, respectively. In contrast, in group B, the mean bite force values at the anterior, right posterior and left posterior regions were 9.45 kg, 19.46 kg and 18.90 kg, respectively. The mean difference between group A and group B at the right and left posterior regions was −1.620 kg and −1.595 kg, respectively, which was found to be statistically significant (p = 0.001 and p ≤ 0.001, respectively). However, at the anterior region, the mean difference was statistically insignificant (−0.632 kg; p = 0.134).
Lastly, after the 6th postoperative week, in group A, the mean bite forces were 10.80 kg, 25.90 kg and 25.30 kg at the anterior, right posterior and left posterior regions, respectively. In group B, the corresponding values were 11.23 kg, 28.52 kg and 27.86 kg at the anterior, right posterior and left posterior regions, respectively. The mean difference between group A and group B at the right posterior and left posterior regions was −2.560 kg and −2.530 kg, respectively, which was found to be significant (p = 0.001 for both). However, at the anterior region, the mean difference was not statistically significant (p = 0.359), with a value of −0.350 kg.
A comparison of the bite force among the control group and study groups (A and B) at the 6th postoperative week was conducted using the ANOVA Tukey’s post hoc test. The mean difference in the bite force at the anterior region between the control group and the study groups was 5.703 kg (p ≤ 0.001) and 5.353 kg (p ≤ 0.001), respectively, which was statistically significant. Similarly, the mean difference in the bite force at the right posterior region between the control group and the study groups was 18.648 kg (p ≤ 0.001) and 16.088 kg (p ≤ 0.001), respectively. At the left posterior region, the mean difference in the bite force was 17.223 kg (p < 0.001) and 14.693 kg (p ≤ 0.001), respectively. The observed difference in the bite force between the study and control groups in both the right and left molar regions was statistically significant (Table 1).
All patients in the study groups were followed up for 1 year. They were evaluated for the presence of complications, including occlusal discrepancy, mobility between segments, infection at the fracture site, and plate fracture. Two patients in group A and 2 patients in group B experienced fracture site infection at the 12th and 13th weeks and at the 11th and 16th weeks, respectively. This was effectively managed with antibiotics, and no further intervention was required. There were no complications observed in either of the study groups.
Discussion
Arbeitsgemeinschaft Osteosynthesefragen/Association for the Study of Internal Fixation (AO/ASIF) recommendations for rigid fixation are based on 4 fundamental principles: bony segment reduction; stable fixation; immobilization of fragments to maintain adequate blood supply; and early return of function.8 Advancements in techniques, biomaterials, and understanding of biophysics have significantly influenced the application of fixation in facial fractures. Internal fixation with titanium hardware is the most commonly used method for the treatment of facial skeletal injuries, with numerous systems available for this purpose.9
A miniplate is a semi-rigid fixation system designed to achieve multiple points of bone fragment fixation, thereby maintaining facial dimensions, preventing rotational movement of fragments, and providing interfragment stability. Adverse outcomes associated with miniplates that may necessitate removal include plate prominence, palpability, infection, migration, and exposure.10 In mandibular fractures, infection and exposure are the most common reasons for plate removal, whereas prominence and pain are primary concerns in midface fractures.7 A review involving 507 patients (1,112 facial fractures) demonstrated that 12% of patients required miniplate removal due to various reasons.11 To reduce the risk of postoperative complications and the need for implant removal, it is desirable to minimize the size and amount of material used.
It has been reported that metal deposits can occur in close proximity to titanium miniplates and in peripheral organs after osteosynthesis.12 Additionally, the implant used should require a minimal degree of periosteal stripping. The preservation of vital periosteum facilitates fracture healing, reduces the likelihood of postoperative wound breakdown, and lowers the incidence of hardware-related infections. Therefore, it is logical to minimize the quantity of osteosynthesis material used.
The use of microplate systems in the craniofacial region was first presented by Hans Luhr in Atlanta in November 1987.13 Clinical indications for the use of microplate systems include naso-ethmoid, infraorbital, frontal, and calvarial fractures.14, 15 These systems offer greater adaptability to the contours of the midface skeleton due to their easier malleability. Their lower profile reduces plate palpability and pain, while also lowering the risk of exposure during midface fracture treatment.16, 17, 18
The use of microplates in the treatment of mandibular fractures is limited, with only a few papers reporting on its efficacy.12, 19, 20, 21, 22, 23, 24 Recent experimental and clinical studies have shown favorable outcomes with the use of microplates in the stress-bearing areas of the mandible. An experimental study demonstrated that microplates have reduced load-bearing ability in comparison to miniplates. However, microplates possess nearly equal torsional force and sufficient stability for mandibular osteosynthesis. In a prospective study, Song et al. concluded that mandibular fractures can be effectively fixed with 2- or 3-point fixation using microplates, without the need for maxillomandibular fixation, ensuring good stability, adaptation and patient comfort.21 Similar results were published by Kumar et al. on the treatment of inter-foraminal mandibular fractures.22 The torsional strength of microplates was found to be similar to that of the miniplate system.
The primary goal of fracture management is to facilitate the early return of function. The early mobilization of the jaw and the restoration of adequate bite force for mastication should be the primary objectives in managing mandibular fractures.15 In the present study, the bite force was evaluated as the primary treatment outcome. Similar use of the bite force for evaluating the efficacy of microplates in the fixation of mandible fractures has been reported in the literature.12, 20, 22
The present study demonstrated a progressive improvement in the bite force in both study groups. However, the bite force measurements at all intervals were consistently lower in the microplate group compared to the miniplate group. This difference was statistically significant at the 2nd, 4th and 6th postoperative weeks. This finding is in agreement with the results of a previously published study by Ahmed et al.20 Contrary to our findings, Anand et al.19 reported no significant difference in bite force values between the 2 plating systems. However, their study design differed, with 2 miniplates in 1 group and a combination of 1 miniplate and 1 microplate in the other.
In comparison to the control group, patients in both study groups showed a reduction in the bite force at the last follow-up (6th week). This suggests that the bite force of patients treated with either microplates or miniplates does not return to its baseline values by the 6th week of fracture healing. Two patients from each study group experienced surgical site infections, which were managed conservatively with antibiotics. There were no reports of fracture segment mobility, plate/screw loosening, or occlusal discrepancy in either group.
Although this study used microplate fixation in adult cases of undisplaced or minimally displaced anterior mandibular fractures, its use in the pediatric population and for comminuted mandibular fractures has also been documented. The low profile and malleability of microplates facilitate better adaptation and minimize trauma to tooth buds in young patients.23 Choi et al. found that microplates are strong enough to maintain a reduction in comminuted mandibular fractures.24 Their small size and malleability allow for multiple fixations of comminuted bony segments in an accurate anatomical position with less periosteal stripping and self-occlusal adjustment. However, in the present study, the degree of periosteal stripping required for hardware fixation was not found to be similar in both study groups.
Conclusions
The application of 2 microplates resulted in a reduction in bite force values at the six-week follow-up compared to the miniplate and control groups. Based on the findings of this study, the use of microplates in the management of undisplaced or minimally displaced anterior mandibular fractures should be discouraged. However, further prospective randomized controlled studies with a large sample size and longer follow-up are essential to evaluate the suitability of this system for regular use.
Ethics approval and consent to participate
The study was approved by the Krishna Institute of Medical Sciences Ethics Committee (approval No. KIMSDU/IEC/02/2018).
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.