Abstract
Background. Anxiety during oral surgery can impact patient homeostasis, increase the difficulty of the procedure and create additional stress for the surgeon. Furthermore, it has been associated with more intense and prolonged pain during and after dental treatment.
Objectives. The aim of the study is to evaluate the relationship between anxiety, patient characteristics and pain outcomes in oral surgery, as well as to verify the impact of anxiety on patient’s perception of pain during and after oral surgery.
Material and methods. This is a prospective observational study. Several variables were evaluated during the course of the oral surgery. Anxiety levels were assessed using the State-Trait Anxiety Inventory (STAI), Corah’s Dental Anxiety Scale (DAS), the Interval Scale of Anxiety Response (ISAR), and Patient Self-Rated Anxiety (PAnx) during the procedure.
Results. General anxiety measures (STAI) were not associated with specific dental anxiety or external observations of anxiety. Anxiety levels varied according to gender and body mass index (BMI), and were correlated with increased heart rate (HR) (with variability among assessment tools). Odontectomy, ostectomy and an increased volume of anesthesia were associated with higher anxiety levels (with variability among the assessment tools). There was a correlation between pain and anxiety, with anxiety contributing to approx. 12% of the variability in postoperative pain.
Conclusions. Dental anxiety is a complex, multidimensional mental phenomenon characterized by high variability due to the influence of several dynamic factors.
Keywords: pain, dental anxiety, oral surgery, state-trait anxiety inventory
Introduction
The terms “fear” and “anxiety” are often used interchangeably in dentistry.1, 2, 3, 4, 5, 6, 7 Fear is a normal adaptive response to an immediate threat, whereas anxiety is a response to an anticipated or imagined future threat that can persist and interfere with daily life. However, these terms are usually used synonymously within the field.1, 2, 3, 4, 5, 8, 9 Individuals who experience fear and anxiety related to dental treatment are often referred to as “dentally anxious patients”.1 Anxiety in dental treatment is defined as an organic response characterized by apprehension and increased surveillance in situations of uncertain danger or potential threats to the organism.4 There is evidence indicating that individuals with dental anxiety are more likely to have other psychological conditions, such as depression and obsessive-compulsive disorder. Additionally, patients with anxiety and depressive symptoms tend to have poorer oral health.10, 11 Research has also shown that some individuals with dental anxiety may have a history of sexual abuse,12 highlighting the complexity of the issue.6
Oral surgery can elicit pain and a range of negative emotions,2, 3, 13, 14, 15 with fear of pain during and after oral surgery under local anesthesia being one of the greatest concerns for patients.2, 16 These emotional responses may also affect patient homeostasis3, 15, 17, 18, 19 and increase the risk of adverse situations, procedural difficulty8 and stress for the surgeon.2 In addition, dental anxiety is associated with more intense and prolonged pain during and after dental treatment and oral surgery.1, 2, 3, 4, 5, 20, 21, 22, 23, 24 Dental anxiety may also exacerbate postoperative symptoms in oral surgery, including speech impairment, altered sensation, appearance concerns, increased pain, sickness, and interference with daily activities.25 Collectively, these negative emotional experiences lead to increased patient dissatisfaction with dental treatment.5, 9, 16
Objectives
This is a prospective, exploratory, hypothesis-generating observational study designed to gather information and gain insights about the relationship between anxiety and various variables, conditions and outcomes observed in oral surgery under local anesthesia. The study aims to contribute to the understanding of anxiety by considering a number of factors, including patient characteristics, the type of surgery, procedural techniques, and pain perception during and after oral surgery. The hypothesis states that patient characteristics, the type of surgery and the surgical technique may influence or be influenced by the anxiety levels. Additionally, the study aims to verify the impact of anxiety on patient’s perception of pain during and after oral surgery. Improving our understanding of anxiety in oral surgery can lead to the development of improved measurement formats and effective management strategies, resulting in increased patient satisfaction, trust in dentists, and, ultimately, better oral health experiences and outcomes for patients.
Material and methods
The study was approved by the State University of Ponta Grossa Ethical Committee for Human Research (approval No. 21592119.3.0000.0105/4.383.359) and informed consent was obtained from all participants.
The study population consisted of patients who required oral surgery under local anesthesia. Only patients classified as ASA I or II according to the American Society of Anesthesiologists (ASA) Physical Status Classification System who consented to participate were included in the study. Patients who required premedication with anxiolytics or analgesics (preemptive), pregnant or lactating individuals, minors (under 18 years old), those with contraindications for oral surgery under local anesthesia, as well as patients who developed post-surgical infections or dry sockets were excluded from the analysis. The sample for this exploratory trial was obtained through convenience sampling, with patients included consecutively in a non-random manner. However, for t-tests and correlation analysis (point biserial model), the required sample size was calculated a priori using the following input parameters: a two-tailed test; an effect size of |ρ| = 0.5; an α error probability of 0.05; and a power (1-β err prob) of 0.95, resulting in a minimum sample size of 42 observations or patients (G*Power 3.1.9.7; https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower).
Clinical anxiety evaluation
To assess patients’ anxiety levels, they were asked to complete 2 questionnaires immediately before surgery, namely the State-Trait Anxiety Inventory (STAI) and Corah’s Dental Anxiety Scale (DAS). The surgeon and a research assistant completed the Interval Scale of Anxiety Response (ISAR) questionnaire at the end of the procedure. Additionally, patients were requested to evaluate their level of anxiety during the procedure shortly after its conclusion, while still seated in the dental chair.
STAI
The State-Trait Anxiety Inventory is a questionnaire designed to evaluate an individual’s level of anxiety. The inventory consists of 40 questions, which are divided into 2 subscales: state anxiety (STAI-S); and trait anxiety (STAI-T). The STAI-S reflects a temporary emotional state characterized by feelings of worry and increased activity of the autonomic nervous system. In contrast, STAI-T indicates a persistent tendency to perceive situations as threatening. Each category is comprised of 20 items, including both direct and reverse-worded questions. Scores range from 20 to 80, with higher scores indicating elevated levels of anxiety. In general, scores between 20 and 40 indicate low anxiety, scores between 41 and 60 indicate moderate anxiety, and scores between 61 and 80 indicate high anxiety.1, 4, 9, 26, 27 To ensure accurate results and eliminate confusion regarding reverse-worded questions, the final scores were calculated using an online calculator (STAI Scoring Tool; https://www.nsrusa.org/score.php).
DAS
The Brazilian Portuguese version of DAS (or Corah) was used for the assessment of dental anxiety. The questionnaire consists of 4 questions, with responses rated on a scale from 1 (not anxious) to 5 (extremely anxious). Higher scores indicate higher levels of anxiety. Corah’s Dental Anxiety Scale assesses the level of anxiety experienced by respondents during dental treatment.1, 23, 28 Based on the DAS scores, patients can be classified into 1 of the following categories: (a) low anxiety (4 points); (b) mild anxiety (5–10 points); (c) moderate anxiety (11–15 points); and (d) high anxiety (16–20 points).
ISAR
The perioperative evaluation of anxiety was conducted from the perspective of the surgeon/research team using the adapted ISAR1, 8, 23 immediately after surgery. The questionnaire consists of 10 questions to be rated as observed or not observed based on the following clinical signs: increased perspiration; muscle tension; elevated respiration rate; visible trembling; facial signs of fear or distress; vocal signs such as moaning; self-expression of fear or anxiety by the patient; questions from the patient about treatment necessity or pain; interruption of the procedure by the patient; and the surgeon’s assessment of patient’s anxiety (no/yes). The adapted version employed a dichotomous scoring system for the signs of anxiety (absent: score 0; present: score 1). The scores from the 10 questions were summed to form a clinical observation score for anxiety during dental surgery, with a range of 0 to 10.
Perioperative PAnx and pain
Perioperative Patient Self-Rated Anxiety (PAnx) and the pain experienced during surgery were recorded immediately after the surgery. Patients were instructed to rate their anxiety experienced during the procedure using a visual scale ranging from 0 (no anxiety) to 10 (very anxious), as well as to rate the pain experienced under anesthesia (Panes) and the pain during surgery (Psurg) using a visual scale ranging from 0 (no pain) to 10 (severe pain).23
Clinical course of the surgery
The clinical course of oral surgery was recorded, and the following details were collected: the type of surgery (categorized as non-complicated dental extraction, single third molar surgery, or other dentoalveolar/soft tissue oral surgery); the duration of surgery; the necessity for bone surgery; the need for odontectomy; and the amount of anesthesia administered, among others. Additionally, heart rate (HR) was recorded at 5 time points: measurement 1 (m1; pre-surgery in the waiting room); measurement 2 (m2; pre-surgery in the dentist chair and before the wearing of sterile surgical sheets); measurement 3 (m3; during surgery under anesthesia); measurement 4 (m4; during surgery, approximately midway through the procedure); and measurement 5 (m5; immediately after surgery and after the removal of the surgical sheets). Due to the exploratory nature of this study and ethical considerations, all patients were provided with adequate pain control medication and were allowed to discontinue it if they did not experience pain.
Postoperative pain diary
The patient received a postoperative record. The intensity of pain was self-rated using a visual analog scale (0–100) 7 times (P1 to P7) over a three-day period: at 3 h (P1), 6 h (P2) and 12 h (P3) post-surgery on day 0, and upon waking and at the end of the day (standardized between 6 pm and 8 pm) on days 1 and 2.24 The patients recorded pain based on the most severe experience between the previous annotations.
Statistical analysis
The JASP software v. 0.17.1 (https://jasp-stats.org) and/or the JAMOVI Desktop software v. 2.3 (https://www.jamovi.org/download.html) were used to analyze the data through descriptive and inferential methods. A two-tailed probability of p ≤ 0.05 was considered statistically significant. The variables were categorized as continuous, ordinal, or nominal, and appropriate statistical tests were selected based on these characteristics. The normal or non-normal distribution of the variables was also taken into account, as determined by assumption checks. Missing data was replaced with the sample mean, and outliers were addressed through winsorizing. Cases with missing sensitive data or non-returned diaries were excluded from the analysis.
Results
The sample comprised 74 surgical procedures performed under local anesthesia. Five cases were excluded due to alveolar infection or dry socket, which could significantly increase the pain reports. Additionally, 4 cases were excluded due to patients not returning the postoperative pain diary. Of the 65 patients included in the analysis, 40 were female (61%), with a mean age of 30 ±13 years. The mean body mass index (BMI) was 25.2 ±4.6, and the mean years of education was 12 ±2.6. Of the sample, 7 patients (10%) were classified as having a non-restrictive disease (ASA II), while 2 (3%) were current smokers.
Table 1 shows the descriptive statistics for anxiety and pain measurements.
Relationship between anxiety scores
The relationships between the questionnaires and scales used for the assessment of anxiety are shown in Table 2. An exploratory factor analysis, which included the 5 anxiety measurements described above, indicated a clear distinction between the STAI and the other anxiety measurements based on the factor loadings. Following the theoretical principle of differences between the questionnaires, a confirmatory factor analysis was performed, considering 3 factors: (1) generic anxiety (STAI-S and STAI-T); (2) specific dental anxiety (DAS and PAnx); and (3) external anxiety perception (ISAR). The hypothetical model was confirmed as valid (χ2 = 0.37; comparative fit index (CFI) = 0.99; Tucker–Lewis index (TLI) = 0.99; root mean square error of approximation (RMSEA) = 0.02), indicating that the generic anxiety factor did not show an association with specific dental anxiety (p = 0.52) or external anxiety perception (p = 0.49). However, a significant association was observed between specific dental anxiety and external anxiety perception (p < 0.001).
Anxiety and demographic variables
The general health status (ASA I or II) of the patient, age, education, and the smoking status did not show any associations or differences regarding the 5 anxiety measurements. A negative correlation was observed between the BMI and both ISAR (Spearman’s correlation, rs = −0.3, p = 0.01) and PAnx (Spearman’s correlation, rs = −0.26, p = 0.03). Female patients showed higher anxiety scores than males for DAS (Mann–Whitney, p = 0.001) and PAnx (Mann–Whitney, p = 0.01).
Anxiety and surgical procedures
The increase in HR during surgical procedures showed correlations with ISAR (Spearman’s correlation; HRm3 rs = 0.25, p = 0.04; HRm4 rs = 0.29, p = 0.02; HRm5 rs = 0.25, p = 0.04) and with 1 early postoperative measurement for STAI-T (Spearman’s correlation; HRm5 rs = 0.3, p = 0.01). No correlation was observed between HR and DAS, STAI-S and PAnx.
The surgical procedures were classified as follows: 14 (21.5%) were non-complicated dental extractions, 41 (63.1%) were single third molar surgeries and 10 (15.5%) were other dentoalveolar/soft tissue oral surgeries. In the preoperative analysis (DAS, STAI), anxiety levels did not vary significantly (analysis of variance (ANOVA)) according to the type of surgery. However, there were notable differences in anxiety levels during the procedure for ISAR, with third molar surgeries showing higher scores (Levene’s p-value = 0.8; ANOVA p-Tukey < 0.001). No significant differences were observed for PAnx. The surgical time was longer for third molar surgeries, although no statistically significant difference was observed in comparison to other surgical procedures (ANOVA). The reports of patients interrupting surgery due to anxiety were only associated with ISAR (Mann–Whitney, p < 0.001) and PAnx (Mann–Whitney, p < 0.001).
With regard to additional surgical factors associated with anxiety, only the intraoperative scores were relevant for subsequent analysis. The surgical time did not correlate with increased intraoperative anxiety (ISAR and PAnx). The need for osteotomy increased the reported anxiety levels (ISAR, Mann–Whitney, p = 0.01; PAnx, Mann–Whitney, p = 0.037), as did the need for odontectomy (ISAR, Mann–Whitney, p < 0.001). A positive correlation was observed between the increased anesthetic volume and increased surgical anxiety (ISAR, Spearman’s correlation, rs = 0.43, p < 0.001; PAnx, Spearman’s correlation, rs = 0.28, p = 0.02).
Anxiety and pain
Greater complaints of pain during anesthesia (Panes) were found to be correlated with PAnx (Spearman’s correlation, rs = 0.26, p = 0.03). Anxiety was associated with an increase in pain during surgery (Psurg) (STAI-S, Spearman’s correlation, rs = 0.37, p = 0.002; STAI-T, Spearman’s correlation, rs = 0.27, p = 0.02; PAnx, Spearman’s correlation, rs = 0.43, p < 0.001).
For postoperative pain, anxiety scores measured by DAS, ISAR and PAnx did not show any correlation across the 7 pain measurements. However, STAI-S demonstrated positive and significant correlations (Spearman’s correlation) from P2 to P7 (P2, rs = 0.28, p = 0.02; P3, rs = 0.31, p = 0.01; P4, rs = 0.28, p = 0.02; P5, rs = 0.33, p = 0.008; P6, rs = 0.35, p = 0.004; P7, rs = 0.36, p = 0.003). Additionally, STAI-T demonstrated positive and significant correlations (Spearman’s correlation) for P3 (rs = 0.25, p = 0.04), P4 (rs = 0.3, p = 0.01), P6 (rs = 0.37, p = 0.002), and P7 (rs = 0.33, p = 0.007). When analyzing the overall mean of pain (mean of all 7 pain measurements) (Table 1), only STAI-S maintained a significant correlation (Spearman’s correlation, rs = 0.31, p = 0.01).
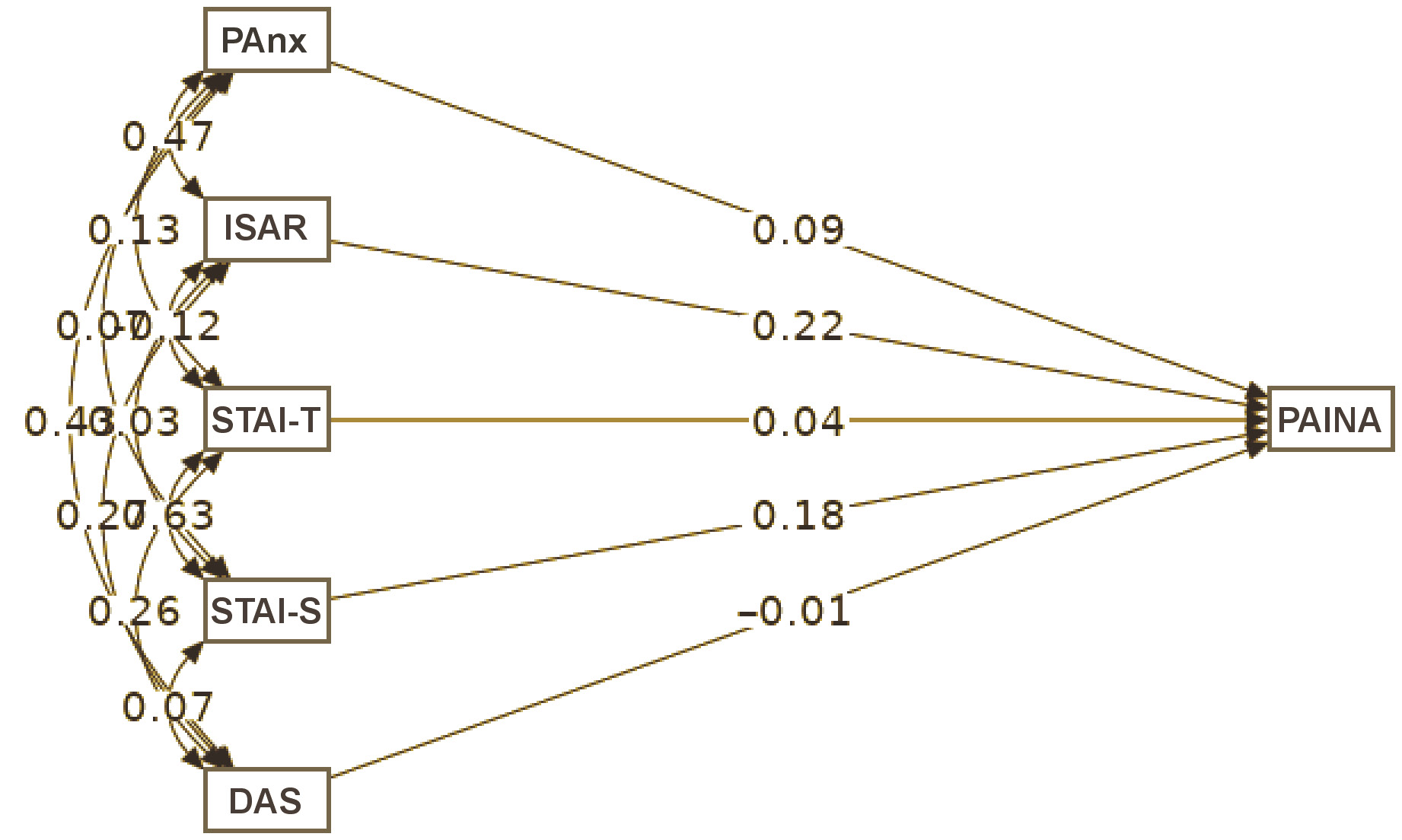
To better understand the implications of anxiety on postoperative pain, a path analysis model was created considering the set of 5 anxiety measurements (DAS, STAI-S, STAI-T, ISAR, and PAnx) as exogenous variables and the mean score of all 7 pain measurements as the endogenous variable (Figure 1). The model was overidentified, and the fit indexes were as follows: χ2 test p-value = 0.1; CFI = 1; adjusted goodness-of-fit index (adj. GFI) = 1; and RMSEA = 0.00. None of the 5 anxiety variables was significantly associated with the mean pain scores. However, the most relevant measurements with greater beta coefficients were ISAR and STAI-S. The model demonstrated that anxiety, as a set of variables, may account for approx. 12% of the variability in pain around the mean value (R2 = 0.12; confidence interval (CI) = 0.012–0.290).
Discussion
In this study, anxiety was assessed through a series of evaluations conducted during the perioperative period for dental surgical treatment. Comparisons were made between the patient’s persistent tendency to perceive situations as threatening (STAI-T), the expectations of anxiety for the surgery (DAS) and the patient’s emotional state (STAI-S), which was marked by feelings of worry about what was to come. These variables were compared with the patient’s self-reported anxiety levels (PAnx) during the procedure, as well as the observable behavior of the patient’s anxiety, as documented by the operators and the research team (ISAR). These comparisons revealed that there was a weak association between DAS and STAI-T, but no association between DAS and STAI-S. In other words, the patient’s anxiety profile (STAI-T) influenced their expectations for the procedure (DAS), but these expectations did not influence their current state of anxiety (STAI-S). However, the patient’s profile (STAI-T) strongly influenced their current state of anxiety (STAI-S).
The observed complexity may be attributed to the characteristics of the questionnaires and the timing of their administration. While STAI is a general instrument for evaluating anxiety, DAS is more specific and focused on dental treatment itself, exploring how a patient anticipates feeling during dental procedures. Lin et al.4 attempted to clarify these distinctions by separating anxiety in dental treatment into state anxiety, which refers to the present moment, and dental care-related anxiety, which refers to a more cognitively involved emotional response to stimuli or experiences associated with dental treatment. However, their meta-analytical study did not identify significant differences between these concepts.4
Dental anxiety can also be a fluctuating emotional phenomenon that varies during the course of oral surgery,23 and that is similar to the physiological responses observed during surgical stress, such as HR.3 Our findings align with those by Hollander et al.,3 who observed a correlation between an increase in HR and increased anxiety. However, these results were consistently captured only by ISAR.
It is also necessary to consider the nature of the analysis itself in order to understand dental anxiety. Initially, the statistical procedures used to describe the associations were relatively simple, and associations between DAS and STAI disappeared when gender and/or the type of surgical treatment were included or controlled for in partial correlations (although this was not reported in the main results). Furthermore, the use of more advanced methods, such as Bayesian statistics, might result in the disappearance of the association between DAS and STAI.
Regarding confirmatory factor analysis, to our knowledge, no previous study has explored this set of anxiety measures as different dimensions. The results of our analysis clearly showed that these tools capture different aspects of cognition or understanding related to dental anxiety. The proposed conceptual model suggests 3 different dimensions: general anxiety (STAI-S and STAI-T); specific dental anxiety (DAS and PAnx); and external anxiety perception (ISAR).
Our findings regarding the associations between anxiety measurements were comparable to those observed by Heaton et al.,1 except for the comparison between DAS and STAI-S. However, it is important to consider the methodological differences between both studies. The abovementioned study reported that DAS was also associated with ISAR (referred to as VAS in their study),1 similar to our observations. Interestingly, the mean STAI scores observed in the study by Heaton et al.1 were lower than those obtained in our study, which focused solely on surgical procedures. This difference may be attributed to variations in perceived threats, such as pain and associated trauma, or it may reflect cultural differences among the studied populations. Nevertheless, Heaton et al.1 also observed that subjects scheduled for surgery obtained higher STAI-S scores, but not other anxiety measures. Similarly, our study found that differences may arise even within the context of proposed surgical treatments. However, this variation was noted only by ISAR (or the team view) and was not reflected in patient perspectives (DAS, STAI and PAnx).
The results of this study indicate that there is no correlation between patient’s self-perception of anxiety (PAnx) during surgery and STAI scores. However, a moderate correlation was observed between PAnx and both DAS and ISAR. This raises several questions: Does STAI effectively capture specific dental anxiety? Is the lack of association between STAI and the patient’s self-perceived anxiety (PAnx) a problem? Could it be related to the patient’s perception of the surgery and self-soothing techniques? Could it be due to the surgeon’s (and team’s) ability to guide the patient through the surgery? To what extent does the surgical team (and researchers) influence patient responses? To what extent can anxiety and pain measurements be influenced by the Hawthorne effect, and how can this be identified, considered and controlled during data analysis? Could surgical complications or an increased perception of difficulty significantly increase negative emotions in patients? Could the experience of pain during the surgical procedure increase anxiety, or vice versa, creating a feedback loop? To what extent does the subjectivity of pain influence emotional subjectivity?
There are many questions that may not have easy answers, because the subjectivity of emotions, including future perspective threat and surgery threat, meets the real physical trauma and inflammatory responses, intertwining psychology and physiology and highlighting the complexity that may arise from these observations. The limitations of questionnaire-based assessments are apparent, given the considerable gaps in the existing paradigm for health measurements. This underscores the need for substantial updates to these instruments to match the complexity of human emotions. Emerging brain–computer interface technologies may help in a better interpretation of human emotional variability in real-time during surgical procedures, potentially rendering long and inefficient questionnaires obsolete.23
In a large systematic review of the factors associated with anxiety related to dental extractions, Astramskaitė et al. observed some similarities among studies and identified problems related to anxiety measurement.2 The review revealed discrepancies in the correlations between factors and anxiety across studies, which were attributed to the use of different measurement scales. The authors attributed some unreliable study results to measurement issues rather than to deficiencies in the instruments themselves.2 They suggested that these instruments may not capture the complex array of variables contributing to dental anxiety, including effects, interferences, circumstances, and the intricate psychological pathways of patients.
In summary, the results presented by Astramskaitė et al. showed similarities with our study, such as different anxiety correlations for the same variables depending on the scale used.2 For example, females showed higher anxiety levels (although with conflicting results), and there were varying findings regarding the association between anxiety levels and education levels and age. Similarly, conflicting results were found regarding anxiety levels and the duration of the procedure, as well as anxiety levels among patients undergoing different surgical treatments. The aforementioned authors noted no association between anxiety and the number of anesthetic injections,2 whereas our study indicated that increased anxiety was associated with a higher amount of anesthetics used (only with ISAR). Additionally, the authors reported no association between the extent of surgery and increased anxiety.2 However, we presume that more invasive, longer and challenging procedures, such as odontectomy and ostectomy, may result in higher anxiety levels, which aligns with the observations made in our study.
Aznar-Arasa et al.8 evaluated dental anxiety in a prospective cohort study focusing on the extraction of impacted lower third molars. They identified correlations between DAS, STAI and ISAR, similar to our study, except for the relationship between STAI with ISAR. The authors observed that procedures involving bone removal and tooth sectioning correlated with higher preoperative anxiety levels, which aligns with our findings.8 Additionally, they reported that anxious patients experienced significantly more difficulties during lower third molar extractions, a result analogous to our finding that patients who interrupted the surgery most frequently were significantly more anxious (ISAR and PAnx).
Few studies have focused on the relationship between dental anxiety and patient sociodemographic characteristics.2, 9, 29 Doganer et al. observed that patients with higher levels of education exhibited lower levels of dental anxiety (STAI-T).9 Additionally, they found that anxiety levels were higher among patients over 25 years of age, those who had fewer dental visits, and those with a history of dental problems. These findings are consistent with those of other studies.29, 30 Astramskaitė et al. added that marital status and social class might influence different levels of dental anxiety.2 Our study contributes to these findings by showing that general health status (ASA I and II), age, education, and smoking did not demonstrate any significant associations with the 5 anxiety measurements. However, our findings indicate that anxiety levels may vary according to sex and patients’ BMI.
Several studies have shown a correlation between pain and dental anxiety, suggesting that patients with dental anxiety may experience more intense and prolonged pain during and after oral surgery.1, 2, 3, 4, 20, 21, 22, 23, 24 Our results support previous findings, indicating an association between dental anxiety and increased patient complaints of pain during and after oral surgery, although not with all measurement models used. For example, pain during anesthesia (Panes) was found to correlate only with the patient’s self-assessment of anxiety (Panx), whereas the perception of pain during the procedure (Psurg) was associated with STAI (STAI-S and STAI-T) and PAnx. Only STAI demonstrated a correlation with postoperative pain. Despite these associations, the observed patterns suggest the existence of a missing link. If this association is consistent across many observations, it is somewhat surprising that it does not appear consistently across all anxiety measurement instruments.
Our previous study observed a weak but consistent correlation between postoperative pain and higher levels of anxiety (STAI-S), regardless of the number of third molars extracted in a single procedure or the use of pain management medication.24 In a preliminary report, de Oliveira Jabur et al. observed a significant correlation between postoperative pain and increased levels of anxiety (STAI-T and patient self-evaluation of anxiety),23 consistent with findings by Lago-Méndez et al.22 However, as noted by other authors,2, 17 the cumulative results regarding dental anxiety and various factors are inconsistent and controversial. Le et al. argue that existing surveys have significant limitations that may restrict the understanding of patient psychology.17 They suggest that many psychological assessments in dentistry lack a strong theoretical foundation and were developed for general assessment rather than for specific dental treatments, thereby oversimplifying the complexity of the issue. Lin et al.4 highlight that anxiety assessment should be a crucial step not only in managing anxiety for highly dentally anxious patients but also in optimizing pain control for all dental patients. The aim of our path analysis model was to explain postoperative pain through anxiety. However, the findings indicated that no single anxiety measurement was significantly associated with pain responses when evaluated collectively as a mean of 7 measurements. However, anxiety may explain approx. 12% of the variability in pain scores around the mean. These results suggest that dental anxiety is a complex, multidimensional mental construct that is influenced by several dynamic factors. This underscores the need for the development of new research approaches and assessment tools in order to better understand this phenomenon. In the words of physicists, we appear to be confronted with a measurement problem.
Limitations
This study was aimed at gathering information and generating new hypotheses. It had several limitations, primarily due to its exploratory and observational nature. The study sample was obtained through convenience sampling and consecutively selected in a non-random manner, potentially introducing selection bias. The representativeness of the sample might have been limited, and the findings may have limited generalizability as the study included only patients undergoing oral surgery, with data characteristics that may differ in other circumstances. Although the data analysis considered variables from different perspectives, isolated them and considered potential confounding factors, we cannot exclude the presence of residual factors that may have affected the results.
Conclusions
The findings of this prospective observational study highlight the following clinical considerations. There is an underlying dimension or latent factor in dental anxiety that cannot be fully explained by isolated measurements from the questionnaires and scales used (DAS, STAI, ISAR, and PAnx). Many correlations were inconsistent both among themselves and with the studied variables, indicating a need for improvements in the assessment tools. Generic instruments such as STAI were not associated with dental anxiety or external observations of anxiety. Female patients and those with lower BMI may exhibit higher levels of anxiety related to oral surgery, with variability across assessment tools. The invasiveness of surgery, including factors such as the volume of anesthesia, odontectomy and ostectomy, was associated with increased levels of anxiety during the procedure. Additionally, anxiety levels correlated with elevated HR (with variability across assessment tools), although the type of surgery proposed did not significantly affect anxiety levels. Pain experienced during and after surgery was found to be associated with increased anxiety levels, with variability across assessment tools. Collectively, the 5 anxiety measurements may account for approx. 12% of the variability in pain.
Ethics approval and consent to participate
The study was approved by the State University of Ponta Grossa Ethical Committee for Human Research (approval No. 21592119.3.0000.0105/4.383.359) and informed consent was obtained from all participants.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.