Abstract
Periodontal mechanical debridement is the most common therapy for the treatment of periodontitis. However, depending on the severity of the disease, mechanical debridement has been recommended in combination with systemic antibiotics. In this study, we performed an overview of systematic reviews using the Friendly Summaries of Body of Evidence using Epistemonikos (FRISBEE) methodology on the effectiveness and safety of mechanical debridement combined with amoxicillin and metronidazole compared to mechanical debridement alone for the treatment of chronic periodontitis. We conducted a systematic search of the Epistemonikos database, extracted data from 10 systematic reviews and re-analyzed data from 23 primary studies to generate a summary of findings (SoF) table. We used RevMan 5.3 and GRADEpro for data analysis and data presentation. The following outcomes were analyzed: probing depth (mean difference (MD): 0.07 mm); clinical attachment level (MD: 0.04 mm); bleeding on probing (MD: 5.06%); and suppuration (MD: 0.31%). There was no evidence of a clinically relevant benefit of periodontal mechanical debridement therapy combined with amoxicillin and metronidazole compared to periodontal mechanical debridement therapy alone for the treatment of chronic periodontitis in the studied periodontal outcomes.
Keywords: metronidazole, amoxicillin, periodontal debridement, periodontal diseases
Introduction
Oral diseases affect many people throughout their lives, causing pain, discomfort, deformity, and even death. They constitute a significant health burden for several countries.1 The most common oral diseases are periodontal diseases, such as gingivitis and periodontitis, with a prevalence of up to 50% worldwide.2 The absence of treatment can lead to tooth mobility and subsequent tooth loss,3 which, depending on the severity of the disease, may affect a person’s ability to chew and speak, and have a major impact on their quality of life.4
Periodontal treatment involves the removal of biofilms and microbial deposits from root surfaces to reduce the host inflammatory response and tissue degradation.5 However, it is not possible to eliminate all pathogenic bacteria in the subgingival region using instrumentation alone; thus, antimicrobials are prescribed to eliminate the remaining subgingival microorganisms.6 Systemically administered antibiotics reach periodontal tissues through the blood and attack microorganisms that are inaccessible to hand instruments.7 They also help to eradicate infections by suppressing periodontal pathogens that invade subepithelial periodontal tissues and other extradental tissues, such as the deep crevices of the tongue.6 Therefore, prescribing systemic antibiotics in therapy is considered beneficial for the eradication of pathogenic bacteria.8
In recent years, there has been a growing interest in the use of endogenous molecules or natural products as adjuvant therapies for the long-term treatment or maintenance of periodontitis.9 However, antibiotic use is more common. Several combinations of systemic antibiotics are used with mechanical periodontal therapy, with amoxicillin and metronidazole being one of the most common.10 Although this is a widespread practice, it is not yet clear how beneficial it is to prescribe them compared to performing mechanical periodontal therapy alone.11 Several studies have indicated that the administration of antimicrobials in conjunction with mechanical debridement may have a beneficial effect on both the mechanical therapy and microbiological parameters.6 The benefits of adjuvant therapy have been documented in several randomized controlled trials (RCTs), as well as in systematic reviews and meta-analyses.6 Adjuvant therapies can help to reduce gingival inflammation, probing depth, attachment level loss, and the need for future periodontal surgery.12
The objective of the present study is to synthesize the available evidence regarding the practice of mechanical debridement in conjunction with amoxicillin and metronidazole compared to mechanical debridement alone for the treatment of chronic periodontitis. Additionally, we aim to report the therapeutic effectiveness of the aforementioned approaches, based on the outcomes of the studies, including the clinical attachment level, probing depth, radiographic bone loss, bleeding on probing, and suppuration.
Material and methods
An overview was conducted using the Friendly Summaries of Body of Evidence using Epistemonikos (FRISBEE) methodology13 to synthesize the best available evidence on the practice of mechanical debridement combined with the prescription of amoxicillin and metronidazole for the treatment of chronic periodontitis. Our research question was based on the Population, Intervention, Comparison and Outcomes (PICO) strategy, as follows: population – patients with chronic periodontitis; intervention – mechanical debridement combined with amoxicillin and metronidazole; comparison – mechanical debridement; outcomes – probing depth, clinical attachment level, radiographic bone loss, bleeding on probing, and suppuration. Furthermore, a systematic search of the Epistemonikos database of systematic reviews, which synthesizes data from multiple sources, including MEDLINE, Embase, Cochrane Library, and LILACS, was performed.14 No language restrictions were applied, and the search was limited to articles published until July 7, 2022.
The main search terms were “chronic periodontitis”, “periodontal disease”, “pyorrhoea”, “pyorrhea”, “amoxicillin”, “amoxicilina”, “amoxicilline”, “amoxicillinum”, “amoxycillin”, “metronidazole”, “flagyl”, “fossyol”, and “systemic antimicrobials”. Duplicate articles were removed manually using Mendeley Desktop 1.19.8 software (https://www.mendeley.com/autoupdates/installers/1.19.8). Only systematic reviews that met the following eligibility criteria were included: studies in adult patients with chronic periodontitis who had received mechanical debridement combined with amoxicillin and metronidazole as an intervention or mechanical debridement alone as a comparison.
Two authors (DZL, JMPV) independently screened systematic reviews for eligibility based on their titles and abstracts, followed by a full-text screening. Primary studies from the systematic reviews that met the inclusion criteria were selected for data extraction. Any disagreement between the 2 authors was resolved through discussion and consensus, with the arbitration of the third author (CMG) when necessary. A matrix in the XLSX format was employed as an instrument for data collection using Microsoft Excel 2022 (Microsoft Corporation, Redmond, USA), which included the search strategy, characteristics of systematic reviews and primary studies, the assessment of the risk of bias for primary studies, and relevant outcomes.
RevMan 5.3 software (Cochrane Collaboration, London, UK) was used for data analysis, and GRADEpro software (GRADE Working Group) was used to assess the certainty of the evidence. In addition, we developed a summary of findings (SoF) table according to the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) approach. The data was entered into RevMan v. 5.3 software. Regarding measures of treatment effect, we found only outcomes with continuous data. We combined the results by performing a meta-analysis for each outcome using a random-effects model with inverse-variance weighting. Results were reported as mean difference (MD), calculated with its 95% confidence interval (CI). The unit of analysis for all predefined outcomes was periodontal sites of therapeutic intervention. We assessed statistical heterogeneity in each meta-analysis using the Tau2, I2 and χ2 statistics. We considered heterogeneity to be substantial if the I2 was greater than 75% and either the Tau2 was greater than 0 or there was a low p-value (<0.05) in the χ2 test for heterogeneity.
To interpret the results and to rate the certainty of the evidence, we employed the GRADE approach and GRADEpro software. First, we analyzed the overall certainty of the evidence for each outcome individually, downgrading the evidence from “high certainty” to “moderate”, “low” or “very low”, depending on the risk of bias, indirectness of the evidence, inconsistency, and imprecision of the effect estimates. The research protocol is available from the corresponding author upon request.
Results
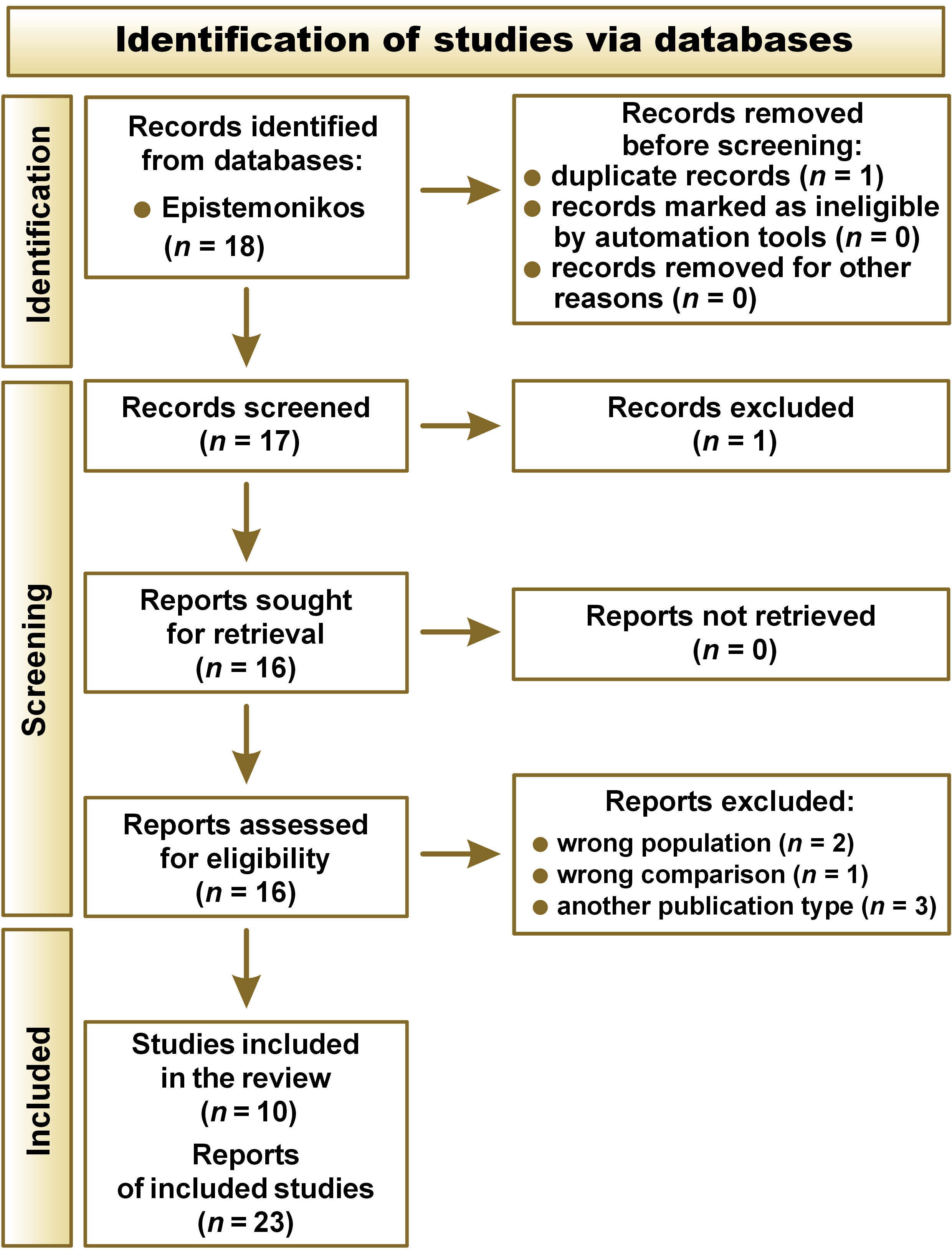
The systematic search yielded a total of 18 articles, of which 1 was a duplicate. The remaining 17 articles were screened based on their titles and abstracts, and 16 studies were included for full-text screening. Ten systematic reviews6, 11, 15, 16, 17, 18, 19, 20, 21, 22 were ultimately included in the development of this FRISBEE overview, which included 23 primary studies.10, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44 All primary studies were randomized clinical trials, reported in 27 references (Figure 1).10, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48
All studies included systemically healthy adult patients (18–70 years old) with a diagnosis of chronic periodontitis. The patients were required to have at least 4 teeth diagnosed with a probing depth greater than 4 mm, a clinical attachment level greater than or equal to 2 mm, and radiographic evidence of bone loss. Additionally, all trials compared the use of mechanical debridement combined with amoxicillin and metronidazole to mechanical debridement alone for the treatment of chronic periodontitis, with a minimum follow-up period of 3 months.
In 7 out of the 23 included studies, amoxicillin 375 mg and metronidazole 250 mg were administered.10, 23, 29, 31, 38, 43, 44 In 5 studies, amoxicillin 500 mg and metronidazole 400 mg were administered together.28, 30, 37, 41, 42 In 4 studies, amoxicillin 500 mg and metronidazole 500 mg were prescribed.24, 27, 34, 35 In 3 studies, amoxicillin 500 mg and metronidazole 250 mg were prescribed.25, 32, 36 In 2 studies, amoxicillin 375 mg and metronidazole 500 mg were administered together.26, 39 In 1 study, amoxicillin 500 mg and metronidazole 200 mg were prescribed,33 and in another study, amoxicillin 250 mg and metronidazole 200 mg were administered.40
Twenty-one trials measured probing depth (849 patients),10, 23, 24, 25, 26, 27, 28, 29, 30, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 44 18 trials assessed the clinical insertion level (758 patients),10, 23, 24, 25, 26, 27, 28, 29, 30, 32, 34, 35, 36, 37, 40, 41, 42, 44 15 trials evaluated bleeding on probing (585 patients),23, 25, 26, 27, 28, 30, 32, 33, 34, 35, 36, 37, 38, 39, 41 and 3 trials reported the percentage of patients with suppuration (142 patients).30, 37, 41 There were no clinical trials reporting radiographic bone loss as an outcome (Table 1).
Based on the analysis performed with the included studies, the main findings of this overview are as follows (Table 1):
• periodontal mechanical debridement therapy combined with amoxicillin and metronidazole could decrease probing depth (MD: 0.07 mm; 95% CI: 0.20–0.05) and increase the clinical attachment level (MD: 0.04 mm; 95% CI: 0.14–0.21) compared with periodontal mechanical debridement therapy alone (low certainty of the evidence);
• radiographic bone loss was not measured or reported in any systematic review or primary article;
• it is uncertain whether periodontal mechanical debridement therapy combined with amoxicillin and metronidazole reduces the percentage of bleeding on probing and modifies the percentage of suppuration compared with periodontal mechanical debridement therapy alone (very low certainty of the evidence).
Discussion
The results of this study are applicable to all systemically healthy adult patients over the age of 18 with mild or moderate chronic periodontitis. The objective of this study was to evaluate 5 outcomes. However, one of the proposed outcomes was not reported in the studies that met the eligibility criteria. Two of the remaining 4 outcomes were considered critical in the evaluation of periodontal parameters in periodontitis, namely probing depth and the clinical attachment level. Additionally, bleeding on probing and suppuration were evaluated as surrogate outcomes. The GRADE approach revealed that the evidence supporting the advantages of periodontal mechanical debridement therapy combined with amoxicillin and metronidazole compared to periodontal mechanical debridement therapy alone was of low or very low certainty.
The GRADE approach criteria revealed issues with the domains of risk of bias, inconsistency and imprecision. In several trials, the process of random sequence generation, allocation concealment, and blinding of participants and assessors was unclear.23, 32, 34, 36, 44 Additionally, there was missing outcome data when assessing the risk of bias,36, 38 and the reasons why data or records were lost or unavailable were not stated, which may introduce bias in the estimation of the effect of the intervention. With regard to the inconsistency domain, high heterogeneity was observed in the magnitude of the effect on bleeding outcomes, with an I2 of 94%.10, 23, 25, 26, 27, 28, 30, 32, 33, 34, 35, 36, 37, 38, 40, 41 Regarding imprecision, the effect of bleeding on probing outcomes had a wide CI, making it difficult to assess the magnitude of the effect in a single clinical trial. In addition, the limits of the CIs for probing depth and clinical insertion level outcomes led us to a different decision regarding the effectiveness of periodontal mechanical debridement therapy combined with amoxicillin and metronidazole compared to periodontal mechanical debridement therapy alone. However, a strength of this study was the achievement of an optimal sample size for the outcomes of probing depth and the clinical insertion level (849 and 758 patients, respectively).
The results of our study were consistent with 2 of the identified systematic reviews,6, 15 which found no clinically relevant effect on any of the periodontal parameters studied when comparing the effectiveness of periodontal mechanical debridement therapy combined with amoxicillin and metronidazole to mechanical periodontal therapy alone for the treatment of chronic periodontitis. In both studies, the certainty of the evidence was also very low. However, our results are in disagreement with the reviews performed by Zandbergen et al., Herrera et al. and Haffajee et al., which indicate that probing depth, the clinical insertion level and bleeding on probing improved in the antibiotic group.18, 19, 22 Despite the positive results of these studies regarding periodontal outcomes when antibiotics were administered, none of the studies established whether these results are clinically relevant. Therefore, it is not reported whether only a favorable statistical result was obtained or whether this minimal favorable difference represents a significant benefit to patients. In addition, our study partially aligns with 3 reviews that identified an additional benefit in probing depth and insertion level outcomes, but not in bleeding on probing.11, 16, 20, 21 Likewise, our results are in partial agreement with the review performed by Santos et al., who observed positive periodontal outcomes in patients who received amoxicillin and metronidazole. However, due to the limited evidence, it was not possible to determine whether the adjunctive use of antibiotics provided a greater benefit than mechanical periodontal therapy alone.17
Although the combination of amoxicillin and metronidazole with periodontal mechanical debridement therapy may improve certain periodontal clinical parameters, bacterial resistance and adverse effects of antibiotics should also be considered.18 Over the past 3 decades, antimicrobial resistance among microorganisms has increased steadily, and the susceptibility of bacteria to antimicrobial agents has become less predictable.6 For this reason, the use of antibiotics in periodontitis should be restricted to specific cases in which the condition is severe or the patient carries a high risk of disease progression and has not responded to conventional mechanical periodontal therapy.18
The European Federation of Periodontology (EFP) has indicated in a clinical practice guideline that although there is evidence that antibiotics systemically improve the clinical outcome of subgingival instrumentation, their routine use in therapy is not recommended, except in cases of generalized periodontitis stage III, which involves a deep probing depth of ≥6 mm or complex anatomical surfaces (root concavities, furcations, infra bony pockets) that may have a difficult resolution. In such cases, the endpoints of mechanic therapy may not be achieved, and further treatment might need to be implemented.49 Likewise, the UK version of the EFP S3-level clinical practice guideline recommends that the use of systemic antibiotics should not be considered a routine adjunct to subgingival instrumentation in patients with periodontitis. However, it should be considered an adjunct specifically in patients with severe generalized periodontitis.50 On the other hand, the American Dental Association’s clinical practice guideline on non-surgical treatment of chronic periodontitis indicates that in patients with moderate to severe chronic periodontitis, clinicians may consider systemic antimicrobials as an adjunct to mechanical therapy, with little expected net benefit, only after other alternatives have been considered.51
The keywords described in the methods section were used to identify 20 ongoing RCTs on this topic, from 2014 to 2022, in the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) and in ClinicalTrials.gov.52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71 Furthermore, we identified 11 ongoing systematic reviews in the National Institute for Health Research (NIHR) International Prospective Register of Systematic Reviews (PROSPERO),72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82 regarding the administration of amoxicillin and metronidazole in periodontal mechanical debridement therapy for the treatment of chronic periodontitis. In the future, these reviews could provide relevant evidence on the clinical question raised in this study.
The main strength of this study is the applied methodology, which involved an in-depth literature search and the synthesis of all available evidence from systematic reviews and primary studies on the practice of mechanical debridement combined with amoxicillin and metronidazole for the treatment of chronic periodontitis, resulting in the identification of 23 primary studies.
Limitations
A limitation of this study is the high variability in the doses of amoxicillin and metronidazole when used as adjuvant therapy. This variability ranged from amoxicillin 250 mg and metronidazole 200 mg to amoxicillin 200 mg and metronidazole 500 mg. Another drawback observed in several clinical trials was the limitations in the randomization sequence generation, concealment, and blinding of participants or personnel. It is recommended that future clinical trials on this topic address this deficiency in their protocols before the start of the study, thus improving the certainty of the currently available evidence. Additionally, the majority of studies classified periodontal diseases based on the old classification by Armitage,83 which limited comparisons between studies. Future clinical trials should classify periodontal diseases based on new classifications, such as the World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions,84 which was released by the American Academy of Periodontology and the EFP. Such an approach would facilitate the interpretation of the results. Furthermore, it is recommended that further secondary research be conducted to evaluate the effectiveness and a risk–benefit ratio of the use of other systemic antibiotics complementary to periodontal mechanical debridement therapy.
Conclusions
This study found no evidence of a clinically relevant benefit of periodontal mechanical debridement therapy combined with amoxicillin and metronidazole compared to periodontal mechanical debridement therapy alone for the treatment of chronic periodontitis when analyzing periodontal parameters such as probing depth, the clinical attachment level, bleeding on probing, and suppuration. However, the confidence in the effect is limited due to a low and very low certainty of the evidence for the included outcomes. Although none of the systematic reviews reported on bacterial resistance and the adverse effects of antibiotics, we consider these outcomes to be relevant to limiting antibiotic use in daily clinical practice.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.