Abstract
Background. As polyether ether ketone (PEEK) is a relatively new material in dentistry, its bonding properties with regard to dental acrylic base materials are not fully known. To ensure the long-term success of removable dentures with a PEEK framework, the base materials must be well bonded to each other.
Objectives. The study aimed to investigate the effects of different kinds of surface roughening treatment on PEEK and acrylic resin bonding.
Material and methods. Eighty PEEK specimens (N = 80) were randomly divided into 5 groups (n = 16 per group) and subjected to various surface roughening treatment (control, grinding, sandblasting, tribochemical silica coating (CoJet), and sulfuric acid etching). Heat-polymerized acrylic resin was applied to the treated surfaces of the PEEK specimens. The shear bond strength (SBS) test, environmental scanning electron microscopy (ESEM) analysis and three-dimensional (3D) surface topography analysis were performed. The statistical analysis of the data was conducted using the analysis of variance (ANOVA) and Tukey’s multiple comparison test.
Results. The one-way ANOVA showed significant differences in the SBS values between the groups (p = 0.001). Sandblasting, tribochemical silica coating and sulfuric acid etching resulted in high SBS values (p = 0.001). The highest SBS values were observed in the sulfuric acid etching group (8.83 ±3.63 MPa), while the lowest SBS values were observed in the control group (3.33 ±2.50 MPa).
Conclusions. The additional roughening treatment applied to the PEEK surface increases the bond strength with heat-polymerized acrylic resin.
Keywords: surface morphology, sulfuric acid, CoJet, polyether ether ketone, sandblasting
Introduction
Polyether ether ketone (PEEK) is a high-performance semicrystalline thermoplastic that belongs to the polyaryl ether ketone (PAEK) family. It consists of a triple aromatic ring unit bonded with 2 ether groups and a carbonyl group.1 Polyether ether ketone is stable against almost all organic and inorganic chemicals, has a high melting point, high hardness, and good dimensional stability. It is also easy to process.2 In addition to these properties, the polymer shows superior properties, such as high fracture strength and low water absorption.3 Due to its mechanical characteristics, such as excellent electrical insulation, it has been used in many sectors, including aviation, automotive industry, electronics, and medical equipment production.4, 5 Its application in the medical field has increased since the 1990s with the use of high-performance thermoplastic polymers for implants and metal components, particularly in orthopedic and trauma cases.6, 7, 8 Polyether ether ketone is compatible with all imaging modalities, such as computed tomography (CT) and magnetic resonance imaging (MRI),9 and its radiolucency enables the examination, diagnosis and treatment of clinical conditions without the need for dismantling or changing the framework.10 In dental treatment, PEEK has been used as an implant material due to its near-bone modulus of elasticity.11 Additionally, it has been used in the production of temporary abutments, bars for implant-supported prostheses, as a framework material in fixed dentures, and for major connectors and clasps in removable dentures.12, 13, 14 Polyether ether ketone can be also used as a denture base material in complete dentures15 and implant-supported overdentures.16 With a wide range of applications in terms of prosthetics, PEEK is a promising material for the future due to its advantages, including lightness, low probability of corrosion, low fatigue, low plaque affinity, and high biocompatibility. It is also an alternative to metal-supported systems.12 Since PEEK-related allergy and hypersensitivity cases have not been observed,17 the material can be used as an alternative to titanium (Ti) and cobalt-chromium (Co-Cr). It may be preferred as a major connector and base material in the production of removable dentures, especially for patients with metal allergies.
Notwithstanding the abovementioned advantages, it is recommended to coat the material with an esthetic layer due to its grayish-brown or opaque color. If used as a base or major connector material in removable dentures, it should form a strong bond with acrylic resin. The chemical aromatic structure of PEEK, along with ketone and other components, provides low bond strength. Therefore, surface treatment, including acidification with acids such as sulfuric acid,18 piranha solution (a mixture of hydrogen peroxide and sulfuric acid)19 and hydrofluoric acid,10 and processes such as plasma or laser application and sandblasting may be required to achieve a better bond.20, 21
However, the bonding mechanisms are changing and are still not fully understood. Data on the bonding of PEEK to dental materials is insufficient. Although the conducted research investigates PEEK and composite bonding, there are not enough studies on PEEK–acrylic resin bonding. Acrylic resin is used as a repair and dental base material in removable dentures.22 It can be polymerized in different ways, using heat, autopolymerization, light, and microwave.23 When PEEK is used as a component of a dental prosthesis, it must be firmly fixed to acrylic resin. A strong bond between PEEK and acrylic resin significantly reduces the possibility of denture fractures.24 The shear bond strength (SBS) test is a commonly used mechanical test for evaluating the performance and bonding properties of adhesive systems in a laboratory environment.25 In addition to mechanical tests, scanning electron microscopes (SEMs) and three-dimensional (3D) optical profilometers are used to examine changes on the surface of the material and the surface topography. Environmental scanning electron microscopy (ESEM) analysis is a method used to examine the natural states and microscopic properties of materials without the need for any coating on the surface of the material.26
Polyether ether ketone is also used as a framework material, so its compatibility with prosthetic materials is of great importance. Improving bonding between PEEK and acrylic resin positively affects the long-term use of PEEK framework prostheses.
The present study aims to evaluate the effects of different kinds of surface roughening treatment on bonding between PEEK and acrylic resin. The null hypothesis of the study is that all kinds of surface treatment applied to the material will increase the PEEK–acrylic resin bond. The other hypothesis is that 98% sulfuric acid etching will result in the highest SBS values.
Material and methods
Specimen preparation
The power analysis was carried out to obtain the highest power level with the smallest sample size, using the G*Power software program (v. 3.0.10; https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower). The analysis revealed that at least 16 specimens were required to achieve the highest power level (power = 80, α = 0.05). A total of 80 specimens (N = 80) were used in this study. The specimens were milled using a computer-aided design/computer-aided manufacturing (CAD/CAM) unit from PEEK blocks (CopraPEEK; Whitepeaks Dental Solutions, Essen, Germany), provided by the manufacturer in the form of cylinders measuring 10 mm in diameter and 2 mm in height. After verifying the compatibility of the obtained specimens with the initial dimensions, the surfaces of the specimens were ground with P600 and P800 grit silicon carbide paper (English Abrasives & Chemicals Ltd., London, UK) for 60 s, and polished with a fine pumice stone (Ernst Hinrichs Dental, Goslar, Germany) and Jiffy™ goat hair brushes (Ultradent Products, Inc., South Jordan, USA) for 60 s in an automatic polishing machine (PM Super, series 2300; Reco Dental, Wiesbaden, Germany) with a vertical force of 25 N to produce a standard surface. Then, the specimens were cleaned in an ultrasonic machine (CD-4800; Jeken, Dongguan, China) for 10 min. After the polishing process, they were stored in distilled water at 4°C until used in the surface roughening procedures.
Surface treatment and imagining
The obtained specimens were randomly divided into 5 groups (n = 16 per group), and each specimen was numbered. The groups were as follows:
Control group: no surface treatment was applied to the specimens;
Grinding group: grinding was performed under water cooling with cylindrical diamond burs (837LF.FG.014, 27–76 µm; Hager & Meisinger, Neuss, Germany) and a multiplier handpiece (a contra-angle handpiece up to 160,000 rpm, Synea Vision TK-100L; W&H, Bürmoss, Austria), using an average finger pressure of approx. 1 N for 10 s. A new bur was used for each specimen to ensure standardization;
Sandblasting group: the surfaces of the specimens were sandblasted with 50-micrometer Al2O3 particles in various directions, at a distance of 10 mm, for 15 s, under a pressure of 4 bars, using the Airsonic® Mini Sandblaster (Hager & Werken, Duisburg, Germany). After sandblasting, the surfaces were washed for 60 s and dried;
Tribochemical silica coating (CoJet) group: the surfaces of the specimens were sandblasted with 30-micrometer silanized Al2O3 particles (CoJet™ Sand; 3M Deutschland, Neuss, Germany) in various directions, at a distance of 10 mm, for 15 s, under a pressure of 2.8 bars, using a pencil-point intraoral sandblasting device (CoJet Prep; 3M Deutschland, Seefeld, Germany). No washing was applied to the surfaces of the specimens to not disrupt the silanization formed after the applied process;
Sulfuric acid etching group: the surfaces of the specimens were treated with 98% sulfuric acid (Fluka buffer solution; Honeywell Deutschland Holding, Offenbach, Germany) for 60 s at room temperature. After the treatment, the surfaces were washed for 60 s and dried.
After the surface roughening procedures were completed, the ESEM and 3D optical profilometry images of randomly selected specimens were taken for each group. The surface imaging was performed using an ESEM (Quanta™ 250 FEG; FEI Company, Hillsboro, USA) without any coating applied to the surfaces of the specimens. The images were recorded at ×3,000 magnification. After the ESEM analysis, the surface topography of the specimens was analyzed using a 3D optical profilometer device (Contour GT-K 3D; Bruker, Mannheim, Germany).
Shear bond strength test
After the surface imaging procedures, the preparation of the specimen surfaces for the SBS test was initiated. All specimens were embedded in cylindrical, transparent, auto-polymerized acrylic resin blocks (Integra; BG Dental, Ankara, Turkey), 25 mm × 20 mm in size, with the treated surfaces exposed for placement in the test device. Afterward, metal molds (thickness: 2 mm; diameter: 6 mm) were placed in the center of the exposed surfaces, and acrylic resin (Meliodent HC; Heraeus Kulzer, Newbury, UK) was inserted through these spaces and heat-polymerized according to the manufacturer’s instructions. The polymerized specimens were placed in a special SBS mold. Force was then applied to the PEEK–acrylic resin junction point at a crosshead speed of 0.5 mm/min in the shear mode of the universal testing machine (2519-106; Instron, Norwood, USA). The SBS values obtained in newtons were converted to megapascals.
Statistical analysis
Statistical analysis was performed using the IBM SPSS Statistics for Windows software, v. 20.0 (IBM Corp., Armonk, USA). The Kolmogorov–Smirnov test for data distribution normality and the analysis of variance (ANOVA) were conducted. Tukey’s multiple comparison test was used for intergroup comparisons.
Results
SBS test results
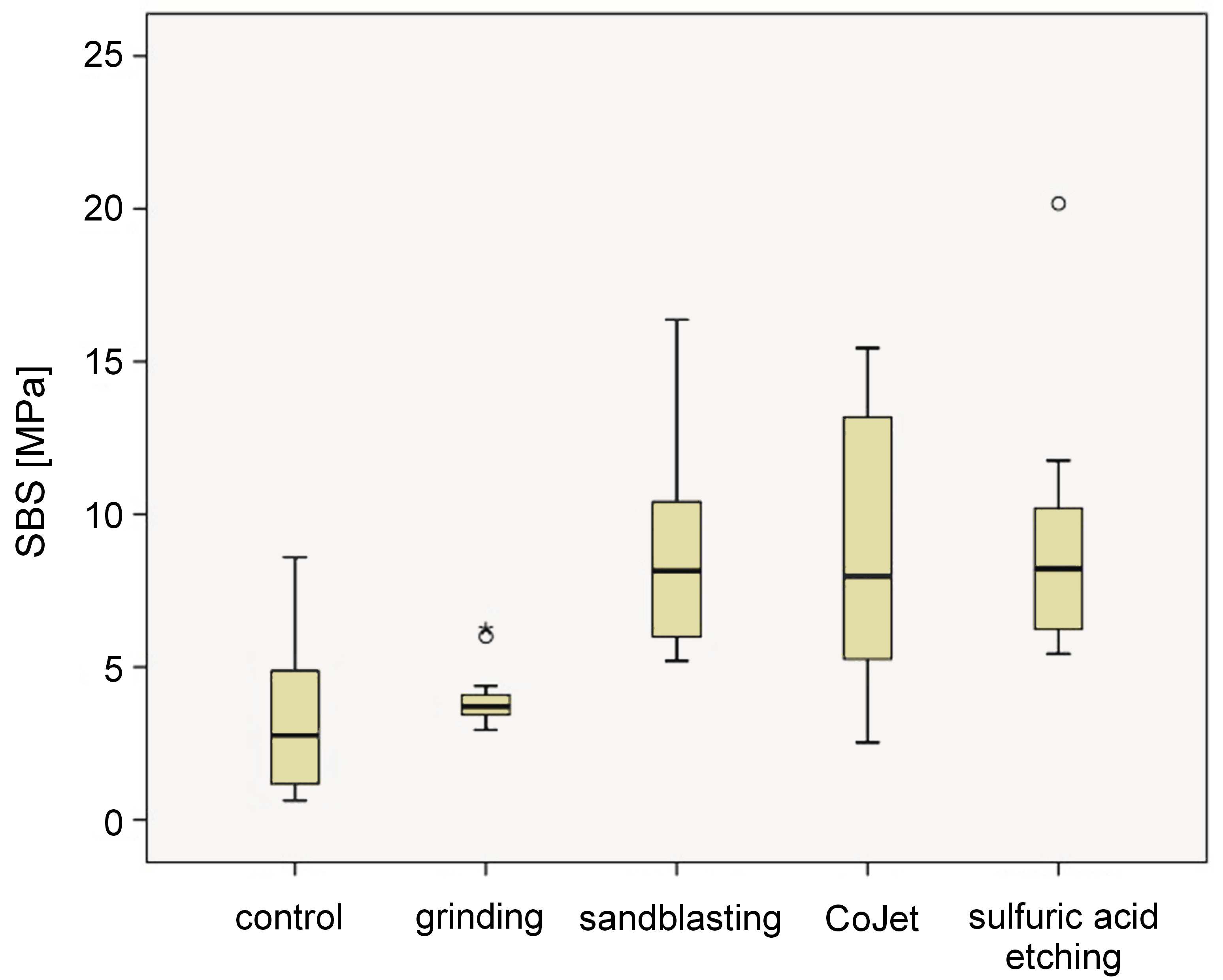
The ANOVA revealed that different surface treatment applied to the PEEK specimens significantly affected the bond strength of PEEK with acrylic resin (p = 0.001). The highest SBS values were observed in the sulfuric acid etching group (8.83 ±3.63 MPa), while the lowest SBS values were observed in the control group (3.33 ±2.50 MPa). Based on the results of Tukey’s multiple comparison test, there were no statistically significant differences between the sandblasting, CoJet and sulfuric acid etching groups (p > 0.05). However, these groups showed a statistically significant difference when compared to the control and grinding groups (p < 0.05). The SBS values for each group are shown in Table 1and Figure 1.
ESEM results
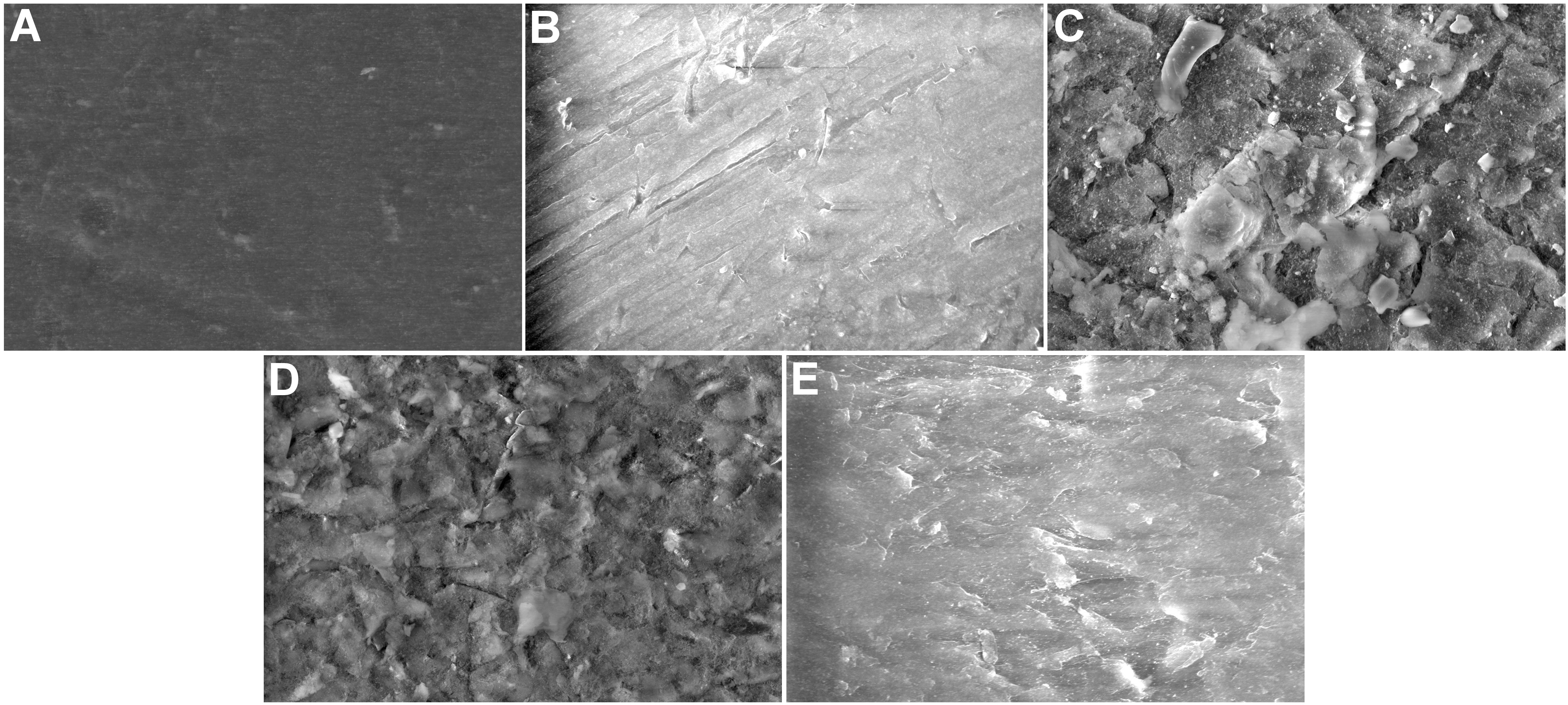
Based on the ESEM examination of the specimens at ×3,000 magnification, it was observed that even though the surface of the specimens in the control group was smooth, it had hollows and micro gaps in some areas. The specimens in the grinding group showed a similar image to the control group despite significant traces of burs on the entire surface. The images of the sandblasting and CoJet group specimens were similar, and the surface structure varied with regard to the specimens in the control group. The applied sands covered the entire surface and created an intense and complex texture. In contrast, the sulfuric acid-treated specimens had a smoother surface covered with a thin layer of scarce micro gaps as compared to the control group ().
3D profilometry results
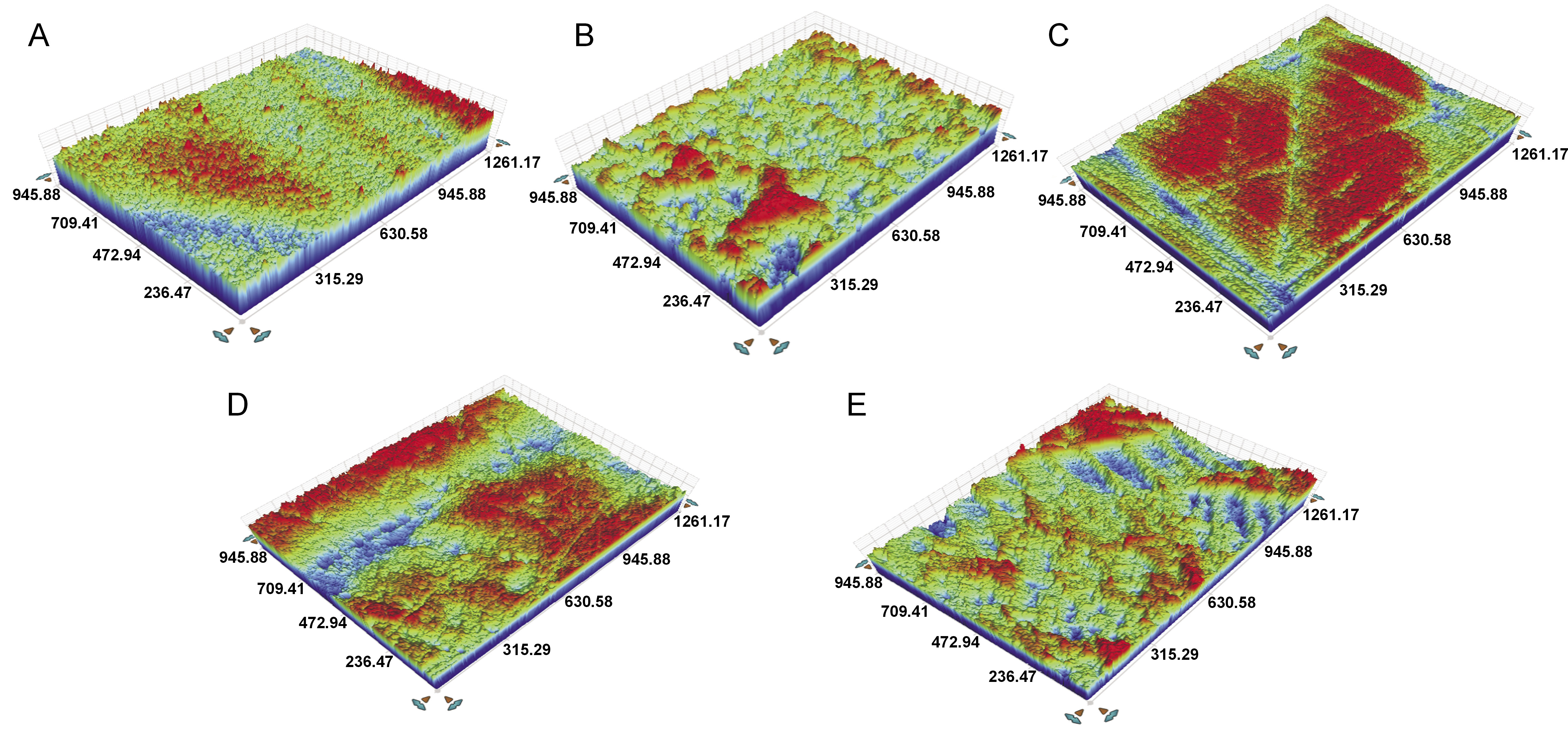
Upon the examination of the 3D profilometry images, rough areas were observed on the entire surfaces of the control and grinding group specimens. These areas were peripheral rather than central in the sulfuric acid etching group. The surfaces in the sandblasting and CoJet groups were similar and had more dense areas ().
Discussion
This study aimed to investigate the effects of different surface roughening methods on PEEK–acrylic resin bonding. The results showed that while sandblasting, CoJet and sulfuric acid etching increased the SBS values of the materials as compared to the control group, the null hypothesis was rejected, since the grinding process did not show a significant effect. However, the highest SBS values were observed in the sulfuric acid etching group, supporting the second hypothesis of the study.
Although PEEK is used in many different areas of dental treatment, it can also be used as an alternative base material in removable partial dentures due to its positive properties, such as light weight, no metal content and the lack of allergic responses.27 When used as a base material or a major connector, it should form a strong bond with the acrylic resin it will be paired with. The surface roughening processes play an essential role in enhancing the bonding by creating a rough area on the material surface.28 In this study, different treatment types were used to roughen the surface of the PEEK material. Studies have reported that 98% sulfuric acid etching creates a highly porous and permeable PEEK surface, which is effective for bonding.10, 21 Some studies indicate that sandblasting is an effective and easily applicable method that enhances bonding by changing the surface morphology of PEEK–composite resin.29 In addition, the tribochemical silica coating process was reported to improve bonding between PEEK and veneer composites.19 Based on the available literature, this study used sulfuric acid etching, sandblasting and tribochemical silica coating as surface roughening procedures, as well as the grinding process, which provides micromechanical retention.30, 31, 32
Studies on the clinical properties of PEEK, a new material used in dental treatment, have recently begun. In addition to research aimed at increasing the bond strength of the material, studies have focused on PEEK–composite resin bonding.10, 18, 19, 33, 34, 35 However, there are few studies on PEEK–acrylic resin bonding. In their study, Kurahashi et al. examined PEEK and auto-polymerized acrylic resin bonding, and reported that the highest bond strength values were observed when the Rocatec treatment was applied in combination with a ceramic primer (Clearfil™ Ceramic Primer Plus; Kuraray Noritake, Tokyo, Japan).24 In the same study, it was reported that the sandblasting process with 50-micrometer Al2O3 particles increased the SBS values as compared to the control group, where no treatment was applied.24 Similarly, in the present study, the sandblasting process with 50-micrometer Al2O3 particles significantly increased the SBS values as compared to the control group (p = 0.001). The formation of a layer on the material surface as a result of sandblasting made it ideal for micromechanical retention and may be considered a reason for this situation. According to the results of the study, the CoJet application significantly increased the SBS values as compared to the control group (p = 0.001). The absence of a statistically significant difference between sandblasting and the CoJet application (p > 0.05) suggests that silica particles were not effective in bonding, and that the CoJet group bound to PEEK specimens through micromechanical retention, similar to the sandblasting group. Additionally, the application of 98% sulfuric acid significantly increased the SBS values as compared to the control group (p = 0.001). The possible reason for this situation is that 98% sulfuric acid may have penetrated into PEEK, creating fibrous micromechanical retention35 and acting as a solvent on the PEEK surface, thereby increasing the bonding.36 The ESEM and 3D profilometer images taken for the specimens also support these assumptions. It was observed that changes on the surfaces treated with sandblasting, CoJet and sulfuric acid etching made the bonding more ideal as compared to the surfaces of the control group specimens. The SBS values obtained from the grinding process carried out with burs were similar to those of the control group, suggesting that the grinding process does not significantly affect the PEEK material. Studies on the acrylic resin–metal framework have shown that mechanical pretreatments (sandblasting and laser irradiation) increase the SBS results as compared to the no-treatment groups.37, 38 It was reported that combined methods applied together with adhesive agents (the primer) further increase these values.38 The values obtained in the present study indicate that surface treatment improves PEEK–acrylic resin bonding. The values were close to those of metal–acrylic resin bonding. Thus, surface treatment is an effective method to achieve the long-term clinical success of PEEK framework dentures.
Limitations
One of the limitations of this study was the evaluation of PEEK–acrylic resin bonding without thermal cycling. Additionally, there could have been more kinds of surface treatment applied in different combinations, and thus more study groups.
Conclusions
Within the limitations of this study, it was concluded that sandblasting, tribochemical silica coating (CoJet) and the 98% sulfuric acid application significantly increased PEEK and heat-polymerized acrylic resin bonding, while the grinding process did not cause any changes. Sandblasting, CoJet and 98% sulfuric acid etching can be safely used to increase bonding between PEEK and acrylic resin, especially in the PEEK frameworks used in removable partial dentures. This will positively affect the durability and efficacy of PEEK-containing removable dentures for patient use.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.