Abstract
Background. The long-term mechanical properties and stability of various resin composites in areas under stress are questionable.
Objectives. The aim of the study was to determine the effects of long-term hydrothermal aging on the mechanical properties of a microhybrid conventional resin composite and its bulk-fill counterpart.
Material and methods. We used a conventional and high-viscosity restorative bulk-fill resin-based composites (RBCs) from one company. Bar-shaped specimens of each type of resin composite were fabricated using steel molds and divided into 2 groups. The specimens were stored at 37°C for 24 h, and half of the specimens in each group were subjected to the 3-point bending flexural test and microhardness measurement. The remaining specimens were aged for 10,000 thermal cycles between 5°C and 55°C, and then subjected to flexural testing and microhardness measurement. A Vickers microhardness tester was used to estimate the surface microhardness of the specimens. Data was analyzed using an independent t test and the Mann–Whitney U test. The statistical significance level was set at p ≤ 0.05. Scanning electron microscopy (SEM) was used to investigate the surface of each material.
Results. The bulk-fill RBC showed similar flexural strength and modulus to its conventional counterpart before aging. The flexural strength of both resin composites was significantly decreased after thermocycling (p < 0.001). Hydrothermal aging had no significant effects on the flexural modulus (p = 0.84). There was a significant decrease in the surface microhardness of the bulk-fill RBC. Scanning electron microscopy photomicrographs showed several pits as a result of the exfoliation of the filler particles on the surface of the bulk-fill RBC after aging.
Conclusions. The flexural strength of both resin composites decreased significantly after aging. The flexural properties, surface changes and microhardness of the bulk-fill type were additionally affected by the aging process.
Keywords: aging, hardness, flexural strength, elastic modulus, composite resin
Introduction
Scientific advances in dental materials have led to the expanded use of resin-based composites (RBCs) for reconstructing large posterior stress-bearing areas previously reconstructed with amalgam.1, 2 However, due to the depth-of-cure problems and the possibility of incorporating voids or contaminations between the increments, restoring deep cavities using 2-mm thick resin composite increments is extremely complicated. Some manufacturers have launched new forms of resin composites, called bulk-fill materials, which are curable up to a 4–5-mm increment thickness, thus speeding up the dental treatment process.3, 4
Bulk-fill materials offer a promising solution to the challenges of technique-sensitive and time-consuming restorative treatments by employing the incremental technique, which uses low-shrinkage RBCs that allow clinicians to apply layers up to 4–5 mm of thickness. Placing resin composites in bulk results in more compact fills and prevents void contamination between composite layers.5
The increased depth of cure can be controlled by increasing the translucency of the material. Due to a linear correspondence between translucency and the amount of filler particles, reducing the filler content is an easy way to increase the depth of cure. The difference in refractive indices between the filler particles and the resin matrix, which governs how light is scattered within a material, also affects the translucency of dental materials. Translucency of experimental dental materials improved when the components of an RBC had similar refractive indices, as observed for bisphenol A-glycidyl methacrylate (BisGMA) and silica filler particles. Manufacturers have tried a number of strategies to increase the depth of cure of bulk-fill resin composites. Reducing filler content and increasing filler particle size are methods for reducing scatter at the resin–filler interface and improving light penetration.6, 7
Some bulk-fill RBCs are called nano or nanohybrid RBCs because they contain a certain amount of low-size fillers. Because their diameter is smaller than the wavelength of visible light, nanoparticles are unable to scatter or absorb it. As a result, they play a key role in light curing, increasing translucency and aesthetics.8 For example, Tetric EvoCeram Bulk Fill (Ivoclar Vivadent, Schaan, Liechtenstein), in addition to having a conventional photoinitiator system also includes an initiator booster (Ivocerin®) that can polymerize the material in-depth.9 There are a few important details about the chemical composition of some bulk-fill RBCs.
Resin-based composites are subject to temperature variations caused by nutrition in the oral cavity as well as complicated mastication forces, including a significant degree of flexural stress.10 A polymer-based material, such as composite resin, can endure deterioration when used in the mouth but its characteristics such as hardness, flexural strength and elastic modulus may suffer.11, 12 Although various laboratory tests for dental composite resins are available, mimicking clinical performance is difficult. They can, however, help us understand how changes in the composition or processes affect the material’s qualities. Flexural strength testing simulates clinical conditions in which materials must endure flexing, particularly in the posterior area. High flexural strength is required for the materials that may fail under large masticatory forces, albeit this has not been clinically proven.13
Thermal stresses are easily formed in resin composites due to various coefficients of thermal expansion and the heterogenous composition of their components, and they can be intensified by thermal cycling in the oral environment. The thermocycling test has gained widespread acceptance as a method to mimic the degradation of the material’s mechanical properties and the quality of the bond strength.14 According to Gale and Darvell, 10,000 hydrothermal cycles with water temperatures ranging from 5°C to 55°C are recommended to demonstrate the durability of the restorations and resemble 1 year of in vivo functioning.15
Changes in the formulation of bulk-fill material in terms of fillers, novel resins, stress modulators, and initiator systems have an impact on the long-term mechanical properties and stability of areas under stress. The mechanical stability of RBC fillings restored with bulk-fill material in stress-bearing areas has been the subject of some debate, presuming that the bulk-fill RBCs are adequately cured and mechanical properties within the incremental thickness remain constant.9, 16 Clinical studies on the bulk-fill class of RBCs are limited and have short follow-up periods.17 However, bulk-fill RBCs seem to be a promising alternative for posterior restorations due to their ease of use and faster restoration time.18
Some studies have explored the behavior of bulk-fill RBCs in terms of degree of conversion (DC), depth of cure and the appropriate light-curing unit.19, 20 To the best of our knowledge, there is little information in the literature on the physical and mechanical behavior of aged bulk-fill RBCs, such as flexural properties and microhardness, in the long-term aging process. Therefore, the purpose of the current study was to compare the mechanical performance of a bulk-fill and a conventional RBC before and after hydrothermal aging using 10,000 thermal cycles.
Material and methods
A conventional RBC and a restorative bulk-fill RBC (Master-Fil™ BULKFILL) from the same company (Dentonics, Monroe, USA) were selected for this study. Eighteen bar-shaped specimens of each composite resin were fabricated using a steel mold and divided into 2 groups (n = 9 for each group).
The International Organization for Standardization (ISO) recommends the use of 25 mm × 2 mm × 2 mm specimens for flexural testing.21 Producing samples of this size without any defects and flaws is very challenging and requires several overlapping irradiations due to the smaller size of the curing tips used in the light-curing units compared to the length of the specimen. Additionally, even though these ISO samples consume large amounts of material, they have no clinical relevance because the cervico-incisal length and mesio-distal width of teeth usually do not exceed 13 mm and 11 mm, respectively.2
The mini-flexural test was chosen for this investigation because of its clinical relevance, higher efficiency and a significant correlation with the ISO flexural test.2, 9 The material for RBCs was compressed between 2 glass plates with intervening mylar sheets, separated by a steel mold measuring 16 mm × 2 mm × 2 mm, to produce the specimens.9 The specimens were irradiated on the top surface, as indicated by ISO 4049 standards.21
The assembly was clamped using a small screw clamp capable of exerting pressure. The middle thirds of the specimens were cured first with a 1200 mW/cm2 multi-wave led light-curing unit (X-cure; Guilin Woodpecker Medical Instrument Co., Ltd., Guilin, China) for 20 s, and then the remaining thirds, which overlapped the middle thirds, were treated. Test specimens were separated from their molds, and the flash was removed using 600, 800 and 1000 grit silicon carbide (SiC) papers and then stored in distilled water for 24 h. The specimens of each type were randomly divided into 2 groups. Half of the specimens of each type were subjected to the 3-point bending flexural test using a universal testing machine (STM-20; SANTAM Engineering and Design Co., Tehran, Iran). The remaining specimens were placed in a basket that alternated between 5°C and 55°C water baths with a dwell time of 20 s and a rest time of 20 s for 10,000 thermal cycles (Delta Tpo2; Nemo, Mashhad, Iran).
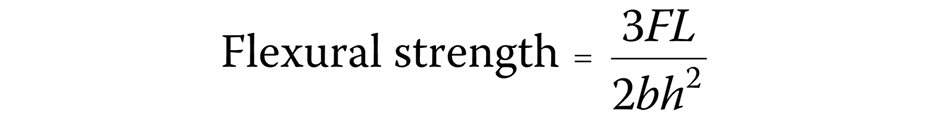
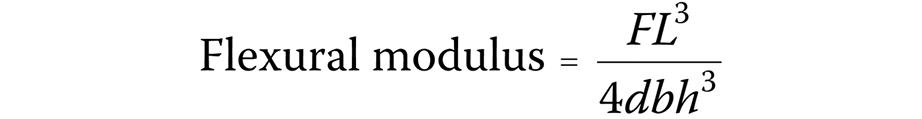
For flexural testing, the specimens were loaded until fracture using a universal testing machine (STM-20; SANTAM Engineering Design Co.) with a load cell of 6 kg (Bongshin Loadcell Co., Ltd., Seongnam, South Korea) at a crosshead speed of 0.5 mm/min and a 12-mm distance between the supports. The maximum load applied to the specimen was recorded, and the flexural strength [MPa] was calculated using the following formula (Equation 1):
where:
F – maximum load on the specimen [N];
L – distance between the supports [mm] (12 mm);
b – specimen’s width [mm]; and
h – specimen’s height [mm].
The flexural modulus [MPa] was determined using the following formula (Equation 2):
where:
d – sample’s deflection corresponding to F.
After flexural testing, fragments larger than 8 mm were used to determine the micromechanical properties of the specimens in each group.9 Measurements were taken at the top of bar-shaped specimens, approx. 4 mm away from the breaking edge, with 3 measurements per sample. The surface microhardness of the specimens was measured using a microhardness tester (Bareiss Prüfgerätebau GmbH, Oberdischingen, Germany) under a load of 300 g for 15 s for 9 specimens. The average value of the 3 indentations for each specimen was taken as the Vickers hardness number (VHN).12 An independent t test and the Mann–Whitney U test were used to analyze the data. The statistical significance level was set at p ≤ 0.05.
A scanning electron microscope (SEM) (VEGA3; TESCAN, Brno, Czech Republic) was used to investigate the surface of each material. Two specimens from each group were randomly chosen for this evaluation, sputter-coated and observed with the use of SEM.22 The SEM photomicrographs were taken at ×2,000 magnification.
Results
The flexural strength and the flexural modulus of conventional and bulk-fill RBCs are shown in Table 1. The bulk-fill RBC showed similar flexural strengths and moduli to its conventional counterpart before aging. No statistically significant differences were found between conventional and bulk-fill RBCs in terms of flexural strength and modulus at the beginning of the experiment (p = 0.34 and p = 0.28, respectively). The flexural strength of both RBCs was significantly decreased after thermocycling (p < 0.001). The lowest flexural strength (52.62 MPa) was observed for the bulk-fill RBC after aging. The flexural modulus was decreased after thermocycling, but the difference was not statistically significant (p = 0.84). Both materials met the ISO requirement for the average flexural strength (80 MPa) for sculptable RBCs before aging. However, after aging, a statistically significant decrease was observed in the flexural strength, which was more pronounced in the bulk-fill composite.
Before aging, the microhardness values of the bulk-fill RBC were similar to those of the conventional RBC (p = 0.848). However, after aging, the bulk-fill RBC showed significantly lower microhardness values when compared to the baseline. There was no statistically significant difference in the conventional RBC microhardness values before and after aging (Table 2).
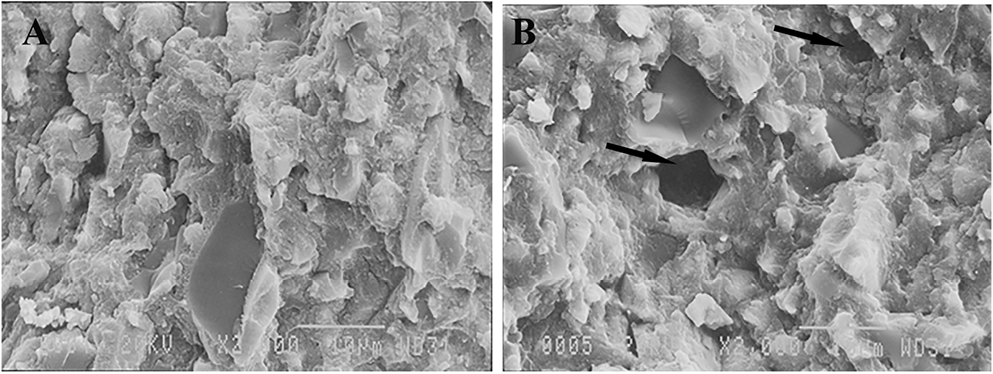
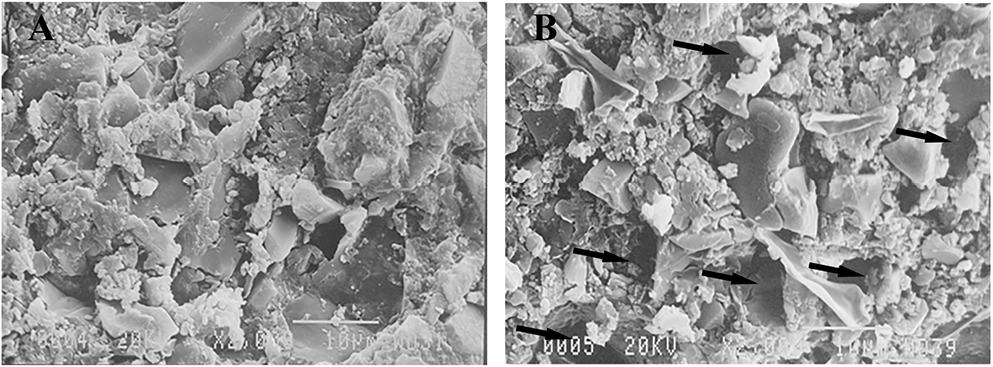
Scanning electron microscopy images of the 2 types of resin composites are shown in Figure 1 and Figure 2. Irregularly shaped filler particles were found in both resin composites. In the bulk-fill type, clusters of fillers with approximate nano dimensions can be seen. The mechanical properties of the composite resins deteriorate during the aging process, as evidenced by surface changes, resin–matrix degradation and filler debonding, all of which can be seen in the SEM images. As the composite resin aged, several pits appeared as a result of exfoliation of filler particles. These findings may explain the reported behavioral variations before and after the aging process.
Discussion
Few studies have compared the mechanical properties of bulk-fill RBCs with other types of RBCs after a short period of aging. Eweis et al. compared the flexural strength and the flexural modulus of high-viscosity and flowable bulk-fill RBCs to conventional RBCs obtained from the same company after 7 days of aging in different solutions.2 However, longer exposure to the medium is necessary to mimic the wet environment of the oral cavity and evaluate the clinical performance of the material.
In the study conducted by Benalcázar Jalkh et al.,14 the mechanical properties of different materials, including bulk-fill composites, were examined after 500 thermal cycles, but the authors used the biaxial flexural test that differs from the flexural test recommended by ISO 4049. In the studies by Haugen et al.,23 Ilie et al.9 and Rizzante et al.24 on bulk-fill materials, the aging period did not exceed 24 h. Therefore, our objective was to evaluate long-term artificial aging-induced alterations up to 10,000 hydrothermal cycles in a bulk-fill composite resin and its conventional counterpart. We examined the mechanical properties of a microhybrid RBC from Dentonics and its bulk-fill counterpart.
Composite resins with a lower modulus may not provide an adequate occlusal stress buffer, so they should be capped with conventional materials. Composites with increased stiffness are necessary in high-stress situations to prevent the deformation of the restoration, which may lead to fractures. For stress-bearing situations, various physical properties of the composites, such as strength, fracture and abrasion resistance, must be addressed in addition to the modulus. Therefore, a high-modulus material is preferred when using bulk-fill (full-body) RBCs to reconstruct large posterior stress-bearing areas.2, 23
In the present study, the bulk-fill RBC exhibited similar flexural strength to its conventional counterpart at the beginning of the experiment. The flexural strength of the bulk-fill RBC was significantly reduced after thermocycling compared to the conventional composite. Studies have reported that bulk-fill RBCs contain polymerization modulators and novel monomers in the resin matrix, which are intended to reduce the polymerization stress of these materials.9 These changes may weaken the polymer network and decrease the resistance of these materials to moisture.25 A further reduction of the flexural strength values observed in the present study after aging may be due to differences in the type, composition and properties of the resin matrix in the bulk-fill RBCs.
Conversely, in the study by Benalcázar Jalkh et al.,14 the decrease in the flexural strength of composite resins after thermocycling was lower than in our study. The disparity in the aforementioned study’s results could be attributed to the variety of the materials tested and the study method used (a biaxial flexural strength test). In addition, the authors conducted only 500 thermal cycles to age the RBCs in their investigation.
The ISO 4049 recommends a minimum flexural strength of 80 MPa for restorative materials affecting outer occlusal surfaces.21 The results of this investigation for both materials exceeded this value at baseline; however, after 10,000 hydrothermal cycles, the flexural strength values were less than 80 MPa, not meeting the ISO 4049 requirements for use as occlusal fillings. Although using bulk-fill composites for large posterior stress-bearing restorations makes the treatment easier and faster, our findings demonstrated that the flexural strength of the bulk-fill composite was further reduced after aging compared to the conventional RBC.
At the beginning of the present study, the flexural modulus of the bulk-fill composite was higher than that of the conventional type, but this difference was not statistically significant. This may be due to the fact that the bulk-fill composite was comparable in filler content to its conventional counterpart. El-Safty et al. discovered a strong relationship between modulus and filler loading.26
Although ISO 4049 does not specify the exact values for the flexural modulus of resin composite materials, according to earlier studies, the flexural modulus should be similar to that of dentin, which necessitates a highly filled composite resin. A lower flexural modulus is preferable to reduce the negative effects of polymerization stress.24, 27
The mechanical properties of composite resins depend on their composition. Resin-based composites with higher amounts of inorganic fillers have a better flexural modulus.9, 28 However, there is an exception to this rule. For example, Tetric EvoCeram Bulk Fill, despite its high filler content, shows moderate flexular modulus values due to the presence of pre-polymerized fillers in its composition, which are included in the total amount of filler.9, 23 Therefore, the content of inorganic filler, which actually increases the modulus of elasticity, is lower in this material compared to its corresponding high-viscosity counterpart.9 Based on the information provided on the Dentonics website (https://www.dentonics.com/composites-and-restoratives?page=2), there is no evidence of incorporating pre-polymerized fillers in the bulk-fill RBCs employed in this investigation. Furthermore, while barium glass filler particles, BisGMA and methacrylate monomers are mentioned, no information is given on the filler loading percentage.
Radiopaque fillers such as barium, strontium and zirconium are commonly employed in the composition of RBCs. These types of fillers, particularly barium glass, can cause a loss in flexural properties due to their weak hydrolytic stability.22, 29
In a study conducted by Rizzante et al.,24 bulk-fill RBCs presented a wide variety of elastic modulus values, but they were generally comparable to RBCs with a regular viscosity. Furthermore, when compared to conventional composites, bulk-fill RBCs generated the same amount of shrinkage stress, especially when larger increments were employed. However, Janda et al.30 found no statistically significant differences in the modulus after thermocycling that would be consistent with the results of our study.
The microhardness of resin composites is not only determined by the organic matrix and the inorganic fillers but also depends on the density and structure of the polymer as well as the DC after polymerization. The higher the number of filler particles, the higher the surface hardness of the material. Hardness is also used as an indirect method of measuring the DC; the higher the conversion rate, the higher the hardness value.31, 32
The initial results of microhardness in the conventional and bulk-fill RBCs in this study were similar, which may have been due to the loading of similar filler content in these 2 types of composites. The results of the studies by Ilie et al.9 and Puspitasari et al.31 demonstrated that some bulk-fill RBCs show less hardness than conventional RBCs with the same filler content. This difference is related to the presence of pre-polymerized organic fillers in addition to inorganic fillers in these materials. According to the information on the Dentonics website, pre-polymerized fillers were not present in the composite resins used in this study. In addition, filler loading is not mentioned.
The results of the studies by Tuncer et al.33 and Ghavami-Lahiji et al.12 showed that 10,000 cycles of thermocycling significantly reduced the hardness of the composites, which could be due to the absorption of water into the composite resins. Prolonged thermal cycling can cause water absorption and matrix swelling. Water can act as a plasticizer, weakening the polymer network and impairing the matrix–filler interface. This is due to the breakdown of chemical bonds at the silane–filler interface caused by water. Filler–matrix debonding, resin softening and even hydrolytic degradation of fillers could all be caused by the water absorbed by the polymer network,12, 22 which could impact the mechanical properties of the resin composite.
Our findings revealed a significant reduction in the microhardness of the bulk-fill RBC after thermocycling, which was not observed in the conventional RBC from the same company. The presence of a different polymer network in the bulk-fill material may be the cause of this issue. Studies have shown that polymer chains with a high crosslinking density absorb less water because of reduced free space, resulting in greater thermal stability.34, 35 The greater microhardness of the conventional RBC compared to the bulk-fill material after thermocycling may be attributed to a denser resin network in the conventional composite or a higher DC. Furthermore, microhardness values of the bulk-fill composite decreased after aging, which was consistent with the flexural strength of this material.
Scanning electron microscopy photomicrograph demonstrated several pits due to filler particle exfoliation on the surfaces of the RBCs after aging. The number of pit defects and the deterioration of the resin network were large enough to affect their characteristics, and these changes were more pronounced in the bulk-fill RBC (Figure 2).
The findings of this study show that the mechanical properties of composites deteriorate over time, especially in bulk-fill materials. According to Leprince et al., the swelling behavior of some bulk-fill RBCs can be problematic, and a capping substance is required not only for aesthetic reasons but also to decrease the destructive properties of the material.27
Limitations
It is important to note that the study investigated only one conventional and one bulk-fill RBC from one manufacturer. Furthermore, the success of composite resin restorations is complex and dependent on a number of factors. Material, clinical, patient, and professional factors can all affect the longevity of dental restorations. Despite the deteriorative alterations seen in the current investigation, such factors should be considered for RBCs, especially in the high-viscosity bulk-fill class exposed to aging in the posterior region. Further research into the functioning of RBCs in clinically relevant situations is required.
Conclusions
The bulk-fill RBC showed similar flexural strength, modulus and surface microhardness to its conventional counterpart before aging.
Hydrothermal aging decreased the flexural strength of both composite resins, and no statistically significant difference was found in the flexural modulus.
Aging had a negative effect on the surface microhardness of the bulk-fill RBC but had no significant effect on the surface microhardness of the conventional RBC.
The flexural strength, surface microhardness and surface changes of the bulk-fill type were further influenced by aging.
Ethics approval and consent to participate
Not applicable.
Data availability
All data generated and/or analyzed during this study is included in this published article.
Consent for publication
Not applicable.