Abstract
White spot lesions (WSLs) are one of the most common adverse effects following comprehensive fixed orthodontic treatment. The purpose of this review was to evaluate recent studies addressing the prevention and treatment of these lesions. Electronic databases were searched for English-written studies published between 2015 and October 2020 involving randomized clinical trials aiming at prevention or treatment of orthodontically induced WSLs using the following keywords in their title or abstracts: randomized clinical trial OR randomized controlled trial AND white spot OR caries OR demineralization OR decalcification OR remineralization. From the 23 papers which met the inclusion criteria, 11 were on preventive methods, while 12 addressed treatment protocols. However, most of the reviewed studies had a high risk of bias. The results of this review strongly support the importance of oral hygiene observation in preventing WSLs. Sodium fluoride varnish 5% was confirmed to be effective in the treatment of these lesions, as well as in the prevention of WSLs in patients with suboptimal oral hygiene. In addition, immediate CO2 laser irradiation after bonding can effectively prohibit formation of WSLs during orthodontic treatment. The literature also illustrates a promising masking effect of resin infiltration for the treatment of WSLs. However, little scientific evidence supports the effectiveness of Casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) against WSLs, although more clinical trials with long-term follow-up are needed. Oral hygiene maintenance is crucial in the prevention of WSLs, and 5% sodium fluoride varnish and CO2 laser irradiation are recommended in patients with compromised oral hygiene. In the case of WSL formation, fluoride varnish and resin infiltration are effective treatment modalities.
Keywords: dental caries, tooth remineralization, fixed orthodontic appliances, randomized controlled trial
Introduction
A common and unpleasant consequence of fixed orthodontic treatments is the development of white spot lesions (WSLs). These are characterized by white opaque lesions that are formed as a result of increased enamel subsurface porosities, which are early and reversible caries.1, 2, 3 While regular caries take at least 6 months to develop, WSLs may become visible within a month following bonding of attachments.4
Since one of the main goals of orthodontic treatment is to improve smile esthetics, WSLs can negatively affect treatment outcomes and lead to patient dissatisfaction,5 and they have a prevalence of 4.9 to 84%. This wide range of prevalence could be attributed to different study designs and the variety of methods used for detection and quantification of demineralized areas.6 Although almost every tooth can be affected, most of the studies report higher involvement rates in the lateral incisors.7, 8, 9
Improvement of WSLs appearance mostly occurs in the first 6-24 months after deboning. This is due to three major factors: oral hygiene improvement and reduction in Streptococcus mutans and Lactobacillus spp to baseline level, remineralization using fluoride-containing dentifrices and mouth rinses, and abrasion of lesions due to brushing.10, 11
Several interventions have been introduced for WSL management. Some are based on remineralization using high concentration fluoride components such as varnish, mouth rinse, and casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) (MI paste/ MI paste plus), while others focus on improvement of appearance by other methods like bleaching, micro-abrasion, and resin infiltration.12, 13
The aim of this literature review was to investigate the latest randomized clinical trials in order to clarify evidenced-based measures for prevention and treatment of WSLs during and after fixed orthodontic treatment.
Methods
Protocol and registration
The current systematic review followed the PRISMA guidelines14 and the Cochrane Handbook for the Systematic Review of Interventions (version 5.1.0).15
Eligibility criteria
According to the PICOS format (Table 1), we included randomized controlled trials on human patients comparing various preventive/therapeutic measures addressing orthodontically induced WSLs to a control/placebo group.
The eligibility criteria are summarized below.
Inclusion criteria:
– randomized clinical trial studies;
– treatment by conventional fixed orthodontic appliances;
– at least one post-orthodontic WSL (trials concerning WSL treatment)
– studies investigating different preventive and therapeutic strategies except veneers; and
– papers published in English between 2015 and October 2020.
Exclusion criteria:
– other designs of studies;
– animal studies and in vitro studies; and
– WSLs not stated to be the consequence of orthodontic treatment
Information sources and search strategy
A comprehensive electronic search was performed in PubMed, Scopus, and Embase databases from 2015 to October 2020 using the following keywords in their title or abstracts: randomized clinical trial OR randomized controlled trial AND white spot OR caries OR demineralization OR decalcification OR remineralization (Table 2). We manually added suitable articles for inclusion, and the reference lists were screened for new trials.
Study selection and data extraction
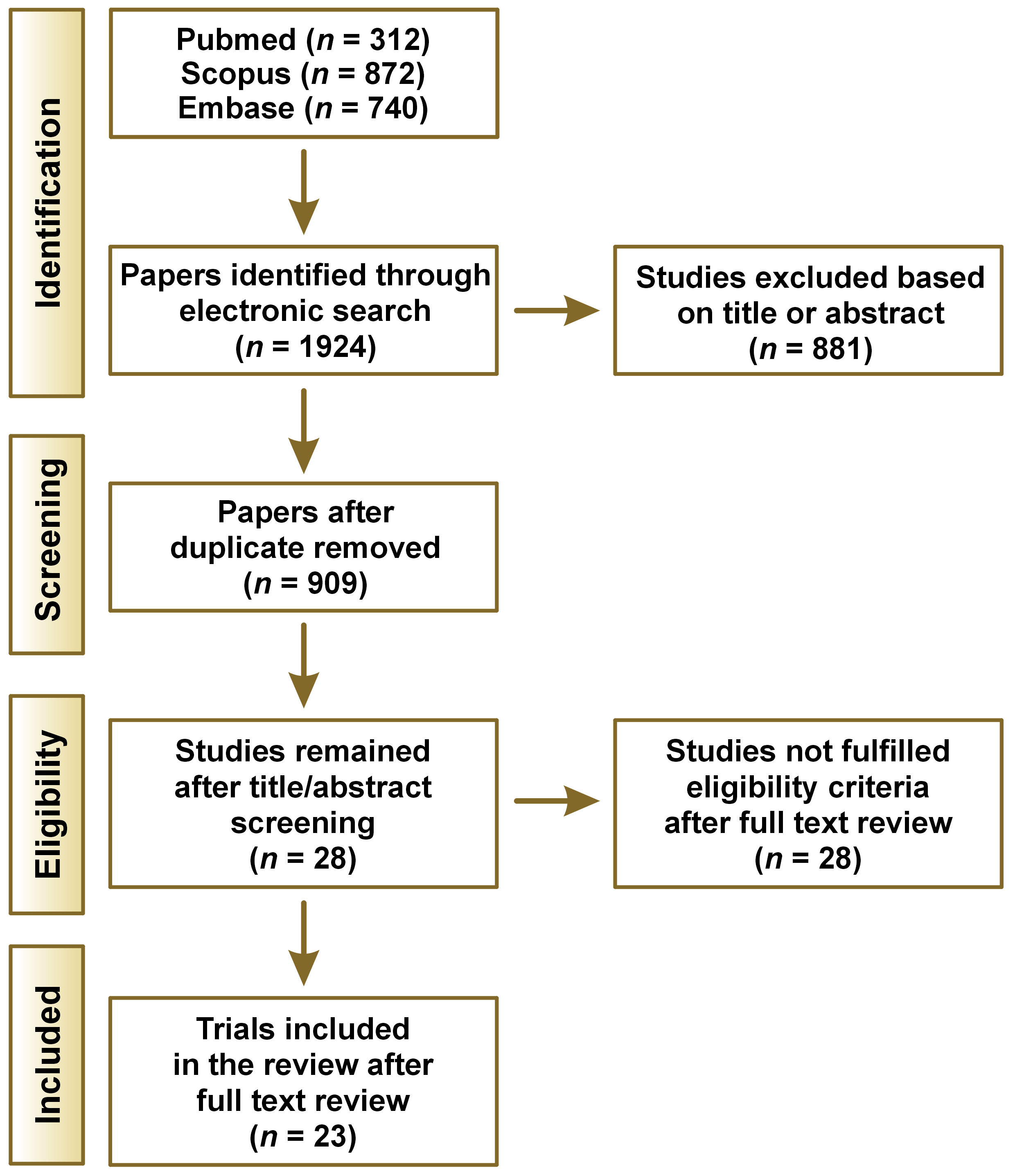
A total of 1924 papers were identified through the electronic search. After duplicate papers were removed by EndNote X9, 909 papers remained. Afterwards, two investigators independently evaluated the titles and abstracts considering the inclusion and exclusion criteria. Inconsistencies between reviewers were excluded from the study unless a consensus was reached. Full texts of 28 relevant papers were selected and reviewed thoroughly, and 23 articles met the final criteria for entering this review (Figure 1). We extracted the following data from the included studies to facilitate comparison among the articles: number of participants, type of intervention, follow-up time, diagnostic method used, and conclusions.
Assessment of the risk of bias in the included studies
Two review authors independently assessed the risk of bias for the included trials using Cochrane’s risk of bias tool.15 The study was judged as low risk if bias of all the domains were low. If at least one domain was considered high risk, the study was judged as high risk. A moderate risk of bias was considered if at least one domain was judged as unclear.
Results
Twenty-three papers met the qualifications for this systematic review. The literature involved both prevention and treatment of WSLs during and after orthodontic treatment.
Eleven papers addressed preventive strategies. One study was on bonding agents (fluoride-containing adhesive resin),16 six on fluoride/ CPP-ACP containing products (varnish, toothpaste, mouth rinse, MI Paste Plus , etc.),17, 18, 19, 20, 21, 22, 23 one study on photodynamic therapy,24 one on special sealant,25 and two studies were on CO2 laser.26, 27
Twelve papers considered therapeutic strategies. Of these, seven studies were on remineralizing agents,28, 29, 30, 31, 32, 33, 34 two studies were on resin infiltration,35, 36 one study evaluated the effectiveness of resin infiltration and microabrasion,37 one study compared fluoride varnish and chlorhexidine mouthwash, and one study compared resin infiltration with varnish.38 Table 3 demonstrates the general characteristics of the twenty-three included papers.
Risk of bias assessment
The details of the quality assessment of twenty-three eligible studies included in this systematic review were extracted and assessment of the risk of bias for included studies was performed. Two studies were assessed to be low, two studies were considered to be moderate, and nineteen studies were classified as high risk of bias (Table 4).
Discussion
WSL development is a common adverse effect following fixed orthodontic treatment which compromises the esthetic outcomes of treatment. Therefore, prevention and management of WSLs is extremely important for clinicians. In this review, we assessed recently published randomized clinical trials concerning both prevention and treatment of post-orthodontic WSLs.
Despite the breadth of literature concerning this issue, there is still no consensus on how to prevent or treat post-orthodontic WSLs. However, it is always easier and more effective to prevent rather than treat.
The current literature contains invaluable reviews concerning white spot lesions.39, 40, 41, 42, 43 However, some of these have focused on a single remineralizing agent,39, 42, 43 and the others were limited to assessing remineralizing agents without addressing contemporary approaches such as laser irradiation,40, 41, 43 and some were not focused on orthodontically induced lesions.39, 40 Another advantage of the current study was the evaluation of both preventive and treatment approaches together. In addition, the current study summarized further information such as location of the lesions and age group of the participants (Table 3). This shows that most of the included studies evaluated the labial surfaces of the teeth with brackets, which is sensible due to the prevalence and mechanism of white spot lesions. However, the studies were limited to patients under 30 years old, which reveals the need for studies on prevention and treatment of lesions in older patients. In the current study, we tried to overcome the shortages with a more comprehensive review.
The diversity in the results from clinical trials can be due to variable methods and study designs, a wide range of products claiming effectiveness on WSL treatment, various methods for the detection and quantification of WSLs, and different procedures for the application of active agents. Visual detection indices including International Caries Detection and Assessment System (ICDAS) and EDI, spectrophotometer, DIAGNOdent, and QLF are the most common methods used for detection and quantification of WSLs. Using the naked eye is not a reliable indicator, whereas magnifying loupes accompanying air drying of tooth surface is an effective method for identifying WSLs of smooth surfaces. However, there is no significant difference between DIAGNOdent and loupes.44 Since all studies using visual indices for detecting or assessing improvement of WSLs has depended on the naked eye only and did not incorporate magnifying loupes, minor improvement of lesions might have been ignored which can directly influence the studies’ results.
Prevention
Results of this review emphasize the pivotal role of routine oral hygiene maintenance in prevention of WSLs. Regular brushing with two different fluoride dentifrices (Clinpro 5000 and Clinpro Tooth Creme) twice daily for two minutes was effective in hindering WSLs, with results comparable to those of MI Paste Plus.20 The importance of routine oral hygiene procedures is also noted by Rechmann et al. who demonstrated that the combination of fluoride tooth paste and fluoride varnish and MI Paste Plus together does not provide any preventive advantage over the routine use of fluoride tooth paste and mouth rinse. In addition, it has been shown that using 5% sodium fluoride varnish is effective against WSL formation only in patients with suboptimal oral hygiene, and it is not useful in those with perfect oral hygiene.19 Similarly, a single dose of elmex® fluid (10,000 ppm) and Fluor Protector S (7700 ppm) had no benefit over the routine sufficient dental hygiene approach, and application of 1.5% ammonium fluoride every six weeks only reduced the number of severe lesions (which are more likely to be sighted in patients with poor oral hygiene).13, 17
Several interventions such as photodynamic therapy, using ultrasonic scaler and the application of sealants have been tested for their capability against WSLs. However, none of them were successful in the prevention of WSLs.24, 25 Resin Modified Glass Ionomer cement (RMGIC) has shown promising results in preventing WSL development during orthodontic treatment.22 However, one split mouth RCT revealed no preventive effect of fluoride-releasing resin composite against demineralization and development of WSLs adjacent to brackets.16
There is ample evidence that laser irradiation makes enamel more resistant to acid-induced demineralization by altering its structure.45 Various types of lasers have been introduced for this purpose, including CO2, erbium-doped yttrium aluminum garnet (Er: YAG), neodymium-doped yttrium aluminum garnet (Nd: YAG), erbium, chromium: yttrium-scandium-gallium-garnet (Er, Cr: YSGG), diode, and argon lasers. However, studies that assessed laser effectiveness in reducing enamel susceptibility were mainly in vitro and were not included in this review.46 There is supporting data for effectiveness of CO2 laser in the prevention of WSL formation. In 2019, Mahmoudzadeh et al. exposed teeth to CO2 laser (0.4 mw, 10.6 μm, 5 Hz) for 20 s following bracket attachment and uncovered that CO2 laser irradiation not only caused a reduction in WSL incidence, but it also diminished their extent and severity after 6 months.26 Raghis et al. also concluded that CO2 laser irradiation had an inhibitory effect on WSL formation during orthodontic treatment after 2 and 6 months.27 The effectiveness of laser irradiation in preventing enamel demineralization was evaluated in a systematic review in 2018; however, more RCTs are needed to verify the clinical efficacy of different available systems.45 In addition, the cost-effectiveness of using lasers should be assessed in comparison to the more economical and accessible traditional approaches, such as using fluoride varnish.
Treatment
Careful supervision and waiting for at least 3-6 months until natural remineralization occurs is the method of choice in most patients. The optimal use of fluoride-containing toothpastes, which is twice daily without excessive rinsing after brushing, must be carefully monitored during this period.13, 47, 48 However, natural remineralization is insufficient in many cases, and sometimes it doesn’t take place at all. Therefore, in many patients, adjunctive considerations should be considered.
Results of this review revealed that MI Paste Plus does not provide any long term benefits in the treatment of WSLs, while short term application of it has shown controversial results.28, 34 All reviewed clinical trials strongly support using 5% sodium fluoride varnish as an effective treatment for WSLs.29, 30, 35, 36, 37, 38
In 2018, Fernandez et.al concluded that most remineralizing agents were not more effective than conventional oral hygiene protocols, and the only effective product for remineralization of WSLs was 5% sodium fluoride varnish applied professionally once per month for 6 months.49 Although application of fluoride varnish on a monthly basis can effectively lead to reversal of WSLs after debonding, the use of high concentration fluoride immediately after debonding is under question, perhaps because surface hyper-mineralization may arrest remineralization and increase the risk of permanent brown discoloration.2, 50
Despite the positive results of fluoride varnish, the effectiveness of using 1.25% fluoride gel for treatment of WSLs is not supported by the literature.32, 33 Application of ACP-CPP alone has not shown significant improvement of WSLs, although it is effective when combined with daily use of fluoride dentifrices.29, 31
Similar to fluoride varnish, resin infiltration has also shown successful results for the treatment of WSLs. Comparison of these two methods demonstrated that resin infiltration shows greater improvement immediately after intervention, while fluoride varnish displays significantly better results over time.38 One split mouth study that compared resin infiltration with microabrasion illustrated esthetic improvement of WSLs with both techniques, but resin infiltration showed better enhancement at 12 months.37
None of the included studies compared microabrasion with a control group. Only one paper made a comparison between resin infiltration and microabrasion as discussed above.37 Microabrasion is an invasive method which is capable of masking more severe and long-standing lesions; however, care must be taken, as this is a sensitive method and should be repeated several times.51 No recent studies concerning bleaching of post-orthodontic WSLs fulfilled the inclusion criteria.
Conclusions
Observation of oral hygiene by brushing with fluoride toothpaste is the backbone of prevention of WSLs in patients undergoing orthodontic treatment. However, application of 5% fluoride varnish or using a CO2 laser after bonding are recommended in patients with compromised oral hygiene. If WSLs are formed during fixed orthodontic treatment, fluoride varnish 5% and resin infiltration are effective methods for treatment.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.