Abstract
Background. Dental education is taking its share of the digitalization of the world. Therefore, it is of value to assess the use of the digital dental education system, especially in the undergraduate period.
Objectives. This systematic review concisely evaluated the use of augmented and virtual reality in preclinical dental education.
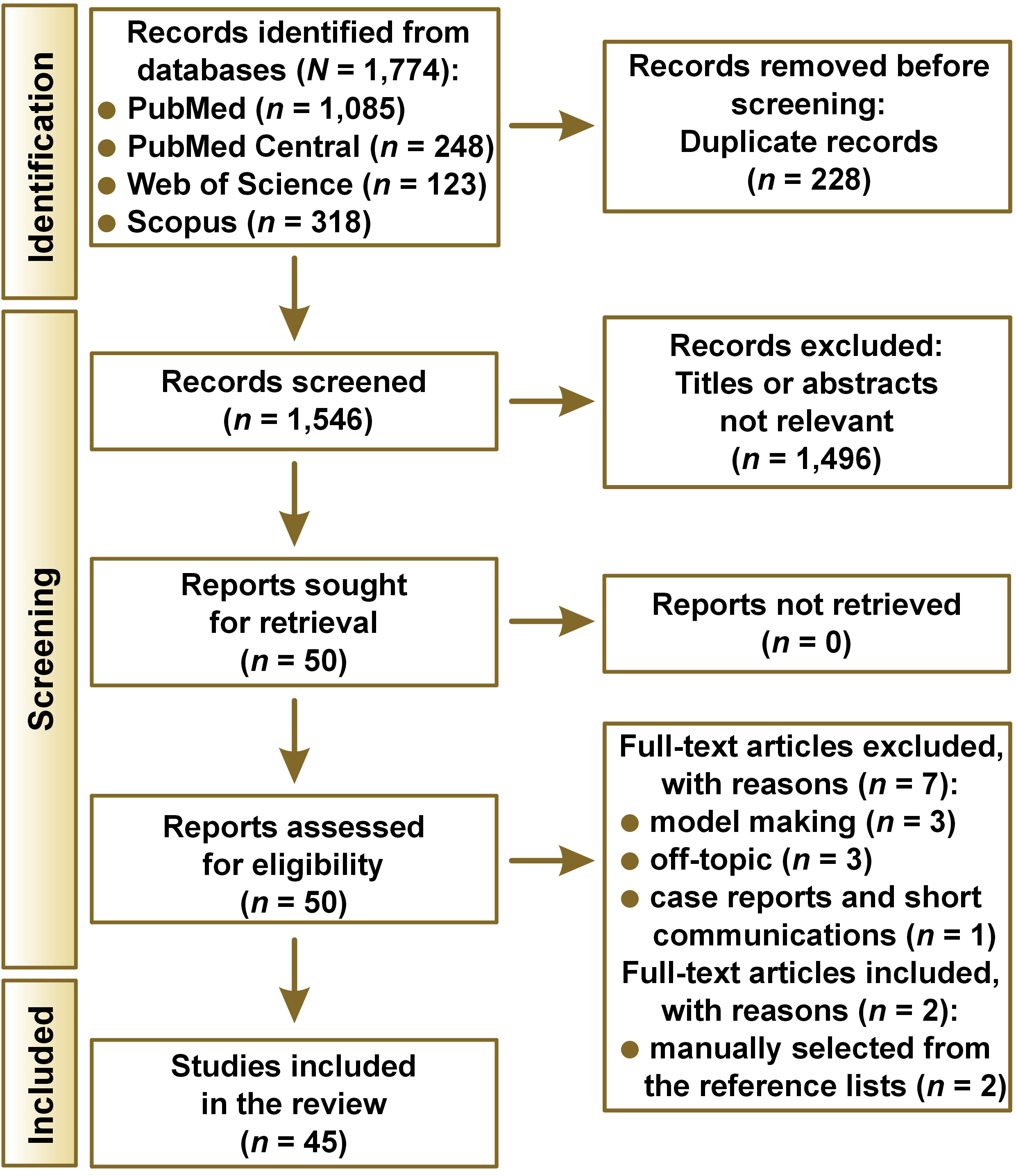
Material and methods. The PICOS (Population, Intervention, Comparison, Outcome, and Study design) search strategy was used with the keywords ‘e-learning’, ‘virtual reality’ and ‘preclinic simulation’ to search the PubMed, PubMed Central, Web of Science, and Scopus databases.
Results. A total of 1,774 articles were found, and 45 articles were reviewed. The level of bias in the studies was also calculated. The studies were divided into 3 main groups: computer-assisted learning (C-AL); augmented reality-assisted learning (AR-AL); and virtual reality-assisted learning (VR-AL). Augmented and virtual reality are steadily evolving, and are increasingly being used in education and healthcare.
Conclusions. The evaluated technological applications enable the visualization of medical information and provide clear feedback during the learning process with increased security and reliability; thus, digital simulation systems can be used to enhance students’ abilities in dentistry.
Keywords: augmented reality, virtual reality, computer-assisted learning, dental simulator, digital dentistry
Introduction
Dentistry involves many skills, among which manual dexterity is the most difficult to maintain.1, 2, 3 Dental students typically take a manual dexterity course during their first 2 years of education. As part of their preclinical practice, students often start with tasks involving simple geometric shapes rather than complex cavity or tooth preparations, and digital systems are rarely deployed. However, technological development is essential in modern dental practice. In addition, digital dental instruction shows high potential in facilitating both direct and distance learning in undergraduate and preclinical education. Indeed, applications based on three-dimensional (3D) imaging and printing, computer-aided design and computer-aided manufacturing (CAD/CAM),4, 5 augmented reality (AR), and virtual reality (VR) have been used in many fields, including dental research and practice, for over a decade.
Translational applications that use cameras in smartphones and popular face-swap applications are among the best-known AR applications encountered in everyday life. A well-known example of a VR application are the glasses used via game consoles. Applications of AR/VR are employed in various fields, such as entertainment, industry, medicine, and dentistry.6, 7, 8
Learning with digital technologies can be categorized as computer-assisted learning (C-AL), AR-assisted learning (AR-AL) or VR-assisted learning (VR-AL). Computer-assisted learning uses computer programs specially designed for education on specific topics. The AR-AL technology uses the existing reality or environments, and enriches them with a computer-generated scenario and the means of interaction. Meanwhile, the VR-AL technology uses only an artificial reality or environments, with which the user can interact.9 By deploying these technologies, users have the opportunity to see preparations from different angles and at different magnifications. Moreover, the real-time feedback provided to the user permits consistent and standardized evaluation.10
The AR/VR components must be well-integrated to achieve the desired effect on users. These components include real and virtual data sources, tracking and registration techniques, visualization processes, perception locations, and feedback mechanisms.
In addition to the growing trend of deploying new information technology applications in education, the quarantine which came with the coronavirus disease 2019 (COVID-19) pandemic also had a marked impact on the education sector, where the traditional systems were forced to be replaced by digitized education. In many countries, students had to be quarantined at home for their safety and online education became the most popular solution for continuing their education, with accessibility and flexibility being among the most important criteria. The advantages of digital education have overcome the problems associated with the traditional education systems almost everywhere.11 Online education has turned every place with access to the Internet into a classroom through personal terminals, such as computers, laptops and smartphones. Furthermore, the sudden closure of universities during the COVID-19 pandemic caused significant changes to the dentistry education system. Consequently, students began to think that they might either not succeed in graduating or graduate without having sufficient practical skills.12 Due to such worries over their preclinical and clinical training adequacy in the context of distant learning, dental students struggled with elevated stress levels.13, 14, 15, 16
If the education system is supported by the AR or VR technologies, students should receive distance education of a higher quality.17, 18 Even though it is well documented that dentistry education deploys the AR and VR technologies, education with AR or VR has never been evaluated along with C-AL systems. However, the C-AL technology should also be evaluated in the same scope as AR and VR.
The primary aim of this systematic review was to present the application areas for the C-AL, AR-AL and VR-AL technologies, and highlight their distinguishing features for dental education. Secondarily, it aimed to determine the application differences between these technologies within dental specialties. Thus, the present study was meant to establish a pathway for further research.
Methods
Ethics statement
This was not a human-subject study; therefore, neither approval by the institutional review board nor the obtainment of informed consent was required.
Protocol and registration
This systematic review followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2020 guidelines. The research protocol was registered in the Open Science Framework (OSF) (https://doi.org/10.17605/OSF.IO/VTQAC).
Eligibility criteria
Table 1 outlines the inclusion and exclusion selection criteria details, which were based on the PICOS (Population, Intervention, Comparison, Outcome, and Study design) framework.
Information sources
and the search strategy
A systematic electronic search of the PubMed, PubMed Central, Web of Science, and Scopus databases was performed. The search was limited to English-language articles published between January 1, 2000, and December 30, 2021.
The search syntax contained Medical Subject Headings (MeSH) terms, and the terms were as follows: (education, dental) AND (virtual reality OR virtual simulation) AND (e-learning OR electronic learning) AND (preclinical simulator OR phantom simulator). All abstracts were read, and duplicates and review articles were excluded. For the final stage, the full texts of all articles were read and relevant information was identified. Abstracts, short communications, letters to the editor, book chapters, and review articles were also excluded at this stage.
Selection process
Two authors (D.E. and B.G.) eliminated duplicated articles manually. They independently checked titles and abstracts to identify potentially eligible studies. If there was persistent disagreement between the 2 authors, a third reviewer (B.G.E.) made the final decision.
Data items and the data collection process
With regard to the general characteristics of the selected studies, the following data was extracted: authors; intervention design; type of digitalized learning technique; specialty; system used; participants; study design; and outcome measures. One author (D.E.) collected the data from the selected studies with the use of an extraction form prepared jointly by the authors. Another author (B.G.) verified the collected information. In instances of disagreement, a third author (B.G.E.) was consulted for the final decision.
Assessment of the risk of bias
The assessment of the risk of bias in the included studies was conducted independently by 2 authors (D.E. and B.G.), using the Medical Education Research Study Quality Instrument (MERSQI). The MERSQI is a tool for assessing the methodological quality of quantitative research articles. The scale consists of 10 items organized into 6 domains: study design; sampling; type of data; validity of the evaluation instrument; data analysis; and outcomes. The total score ranges from 5 to 18. The agreement between the 2 examiners’ results was analyzed using the kappa (κ) statistical coefficient.
Synthesis methods
The data was classified and analyzed to achieve the objectives of this review. The study properties were extracted and key items, such as the acquisition of skills, the quality of preparations and feedback, were tabulated. Data synthesis was initially conducted by 2 authors (D.E. and B.G.), and then discussed with a third author (B.G.E.). The included studies were analyzed through a narrative synthesis. The types of learning methods and the specialization types are presented as percentages.
Assessment of the reporting bias
The reporting bias in this systematic review was independently assessed by 2 authors (D.E. and B.G.) for selective outcome reporting by comparing the study results with the previously published study protocols and registrations. Any disagreement was resolved by consulting a third author (B.G.E.).
Certainty assessment
Not done.
Results
Study selection
A total of 1,774 articles were retrieved via the electronic keyword search. Among these, 228 were evaluated further after eliminating duplicates. Finally, the review included 43 articles identified electronically, and an additional 2 articles were manually chosen from the reference lists of the other articles, resulting in a total of 45 articles (Figure 1, Table 2).
Study characteristics
The studies were divided into 3 main groups: C-AL (n = 5; 11%); AR-AL (n = 16; 36%); and VR-AL (n = 24; 53%). Most articles could be categorized into more than one group, so classification was based on the primary objective of the study (Table 1).
Risk of bias in the studies
The MERSQI scale assessed the methodological quality of half of the included studies as relatively moderate, with a mean score of 10.72 ±1.52 (median (interquartile range) (Me (IQR)): 11.5 (6.0–12.5)) (Table 3). The kappa coefficient of concordance was 0.74.
Results of individual studies
Relevant data from the included studies are grouped and summarized separately in Table 4.
Synthesis results
All the programs used in the C-AL studies were produced for experimental purposes. Except for one study,49 all studies reported that C-AL improved students’ education and satisfaction (9%).38, 44, 46, 50
Many studies stated that VR-AL-based education is as effective as the traditional methods (33%).29, 31, 33, 34, 40, 43, 47, 51, 52, 53, 54, 55, 58, 62, 63 However, a few studies reported that VR education was not sufficient and needed improvement (9%).23, 36, 42, 48 One study reported that educating with the use of VR alone was not suitable for undergraduate education.19
Although few studies examined AR-AL systems, many reported that they were effective for pregraduate education (24%).22, 25, 26, 28, 32, 35, 37, 39, 41, 57, 61 Meanwhile, only one study reported no difference in success between the traditional and AR-AL-based education.24
AR-AL systems were mainly used for restorative dentistry training (29%),21, 22, 24, 25, 26, 27, 28, 30, 32, 35, 37, 39, 57 more so than VR-AL systems (27%),19, 20, 40, 43, 45, 47, 48, 55, 56, 59, 60, 63 and no study related to restorative dentistry teaching used a C-AL system. One study (2%) used C-AL for endodontics training,44 while 2 (4%) used VR-AL systems for this purpose.34, 47 All orthodontics training studies (4%) employed a C-AL system.49, 50 Only one study on pediatric dentistry training (2%) used a VR-AL system62 and 1 (2%) studied periodontology training with a C-AL system.38 Two AR-AL system studies (4%),41, 61 2 VR-AL system studies (4%)31, 36 and 1 C-AL system study (2%)46 were found for prosthodontics. All 3 surgery studies (6%) used VR-AL systems.23, 29, 33
All 6 studies with a geometric shape subject area that could not be attributed to any dental specialty (13%) employed VR-AL systems.42, 51, 52, 53, 54, 58
Reporting bias
The search showed that none of the protocols or records of the included studies were previously registered. As such, the risk of reporting bias was unclear, as it was not possible to determine if all results were included in the published reports.
Discussion
Modern digital technologies have been used in medical specialties, such as surgery and echocardiography, for decades.64 The VR and AR systems used in neurosurgery and cranial surgery are highly advanced, although they are not as common in dentistry.65 Surgeons can access information on the patient’s medical status throughout the operation by using smart glasses.66 Such features may play a vital role in reducing surgical risks, even during routine procedures.
New technologies have recently become available for medical and dental education. While some of these technologies let the lecturer communicate with students, other digital technologies, such as cloud-based systems, allow data storage and its timely access. Therefore, using digital technologies for education enables low-cost, easy-to-use, reproducible, and equitable assessment and evaluation of students.67 Among the types of digitalized learning, Internet-based and electronic educational applications fall within the scope of e-learning.
C-AL applications are programs that proceed within the framework of specific algorithms and contain codes specially written for education, though they do not include any real or virtual practical application steps. AR-AL uses a computer to process the data collected during the dental operation, and provides instructions and feedback to the user. VR-AL allows the operator to use haptic devices for dental procedures in a completely virtual environment, with instructions and feedback received from the computer.
Computer-assisted learning, augmented reality-assisted learning and virtual reality-assisted learning
Learning has been defined functionally as changes in behavior that result from experience, or mechanistically as changes in the organism that result from experience.68 In a typical classroom setting, information generally flows in only one direction, which can be considered passive learning. However, current education requires the development of more active learning through interactive systems. This transformation in learning has already started and has become a critical factor in health education. For example, anatomy is one of the specialties that has benefited most from AR; consequently, it is now possible to learn live anatomy by visualizing internal structures.69
Many studies have assessed C-AL in dentistry, especially during undergraduate education. With the use of C-AL, the educational satisfaction level of students increases.44 Including interactive tasks in the curriculum may also prevent demotivation in students.38 Therefore, using C-AL may be an efficient way to enhance learning, especially during repetitive tasks.50 Another benefit of using C-AL is that it requires less hardware than AR-AL and VR-AL systems.
During preclinical dental education, students receive directions from instructors, who evaluate their work before they proceed. Students generally receive feedback directly from instructors at the end of the procedure. However, such delayed feedback may potentially lead to overlooking errors. With VR-AL, students learn faster and perform a higher number of exercises as compared to the traditional systems, and also receive regular internal evaluation, which reduces the time needed for the assessments made by instructors.70
Some authors have reported that VR-assisted training is not a sufficient replacement for the traditional training.62 Indeed, only 27% of the participating students found the textural or tactile sensation to be adequately close to reality.62 Generally, the traditional educational methods are used alongside supportive digital educational methods. Therefore, including standardized digital learning materials with real-time feedback would increase student performance and reduce the learning time. Such an approach would allow students to practice more repetitive procedures for the development of motor skills.
Skill acquisition using augmented
and virtual reality systems
Manual dexterity is used to execute motor skills, and is a permanently acquired ability resulting from practice and experience. The skills associated with AR and VR are continually evolving, and are becoming increasingly used in education and healthcare. These technological applications are useful, as they allow the precise visualization of medical information. Moreover, these systems provide more accurate information during the process, resulting in increased security and reliability.71 By applying the same principles to restorative dentistry, AR and VR simulations can help students improve manual dexterity during Class I and Class II cavity preparations.57
Although this systematic review included only 45 studies, many articles describe the future of digitalized dentistry applications. Both AR and VR systems play a substantial role in dental education. Moreover, AR systems could be used as an educational standardization medium. One of the studies investigated and compared the removal of carious lesions by novice students and experienced dental residents, and found that novice students removed less material, including sound and carious tooth structure, than residents; the results also demonstrated that caries removal skills could be taught by using computer simulators.45
Immediate feedback is one of the major advantages of digital systems, with many using application time data, target-based data, clinical step data, and motion and force exertion tracking data to provide feedback to the user. Digital simulators can provide information on the preparation size and the amount of removed matter, and observe the stroke magnitude and the movement speed, thereby monitoring the user’s professionalism.72 It has been suggested that just an additional 8 h of computer simulation can improve learning performance.32 A similar study also reported that increasing computer simulation instruction from 6 to 8 h improved practical exam grades among second-year dentistry students.22 With the help of this technology in dental education practical training, it is possible to simulate different scenarios and provide feedback on student performance. In particular, the haptic devices used in VR provide results comparable to a real environment.73 Therefore, learning can be enhanced more easily with VR-AL systems than AR-AL systems.
Another application of AR is a mapping scheme called ‘seeing through reality’, which can be used by operators during surgery.74 Such systems not only assist with operations, but also supply navigation and guidance in real time during surgery, specifically in implant dentistry.75 The AR technology also has diagnostic and treatment planning applications. Navident is the latest AR-assisted implant surgery system. Furthermore, AR-assisted guided surgery is more precise. Even in risky anatomic zones, the average error of the system is approx. 0.96 ±0.7 mm.76
Using digital interfaces in dental education has some limitations. Continuous feedback may cause practitioners to become overly reliant on the system and the cessation of feedback may subsequently lower their performance.77 Although feedback is essential for improvement, reducing feedback frequency facilitates the development of motor and cognitive skills.78 The cognitive load theory predicts that learning varies with feedback during practice. Reduced feedback necessitates more planning to execute the task, whereas increased feedback can cause an information overload.77, 79
Distance learning with augmented
and virtual reality systems
Although it is challenging to execute practical exercises remotely, distance learning has become a requirement in education, especially due to the concerns regarding face-to-face learning during the COVID-19 pandemic. Nevertheless, there are some disadvantages associated with distance (or online) learning, such as isolation from the community, which can cause participants’ discomfort and reduce motivation for learning.80 In particular, using webcams and microphones can reduce course participation, and cause distractions or difficulties in focusing.
AR glasses, or smart glasses (e.g., HoloLens 2, Meta Quest 2 and Google Glass), show promising effects in education and medicine, and can be an alternative tool in distance learning. AR glasses involve 3 forms of interaction: gaze; gesture; and voice. Additionally, AR glasses can use the position-tracking technology to locate and track the user in their 3D environment, and is equipped with the orientation-tracking technology to recognize what the user is looking at.
Some programs work with AR glasses in an educational context, including HoloHuman and HoloPatient.81 It has been reported that 68% of students agree that the dentistry curriculum statement must include HoloHuman as a supplementary teaching tool during anatomy lectures.82 Another program, HoloDentist, connects 2 distant dentists or students to enable communication and the exchange of information. The newly developed portable learning platform DenTeach consists of smart sensors, advanced robotics, big data handling, 3D printing, AR, and cloud-based computing. This platform is applicable to distance learning in preclinical education.83
AR and VR systems contain processors, software, sensors, and input parts that work together. One limitation of the AR and VR technologies is that development can occur only within the framework of the infrastructure, i.e., software updates can only be performed if the system hardware configuration has the necessary permit. Thus, AR systems, which use a real environment, can be more advantageous in terms of visualization quality than VR systems.
The digital technologies used in dentistry education have both advantages and disadvantages. While C-AL does not contribute adequately to the development of motor skills, it provides an advantage in distance education and reduces educational costs.38, 44, 46, 49, 50 AR systems are advantageous for developing motor skills, since the physical environment used is very close to a real environment, although they do have disadvantages as well, such as the need for consumables, which increase training costs.21, 22, 25, 26, 27, 28, 32, 37, 39, 41, 57, 61 While VR systems enhance motor skills without requiring consumables, they need to be developed to imitate a real environment.19, 20, 23, 29, 33, 34, 36, 40, 43, 47, 52, 53, 56, 58, 59, 60, 62 With a reduction in the cost of haptic parts, AR systems are a promising technology for distance education in the future. Since all digital systems provide objective criteria for evaluating the user, they should be included in dental training.
It should be emphasized that our research was limited to articles related to software developed for educational purposes only. Programs related to dentistry that may also be used for educational purposes in the future were not included. Despite the attempt to include as many accessible studies as possible, only a limited number of them were found to be relevant to this study. Furthermore, considering how rapidly technology is evolving and blended learning is becoming a modular and adaptable teaching and learning approach, it is probable that there exist publications which would either support or contradict the findings of this review. Another limitation of the study is the exclusion of non-English articles.
Future research is needed to explore the feasibility of digital technologies in these areas. Furthermore, evidence for the long-term effect of C/AR/VR-assisted training on student clinical performance and competence, as well as data regarding the cost-effectiveness of these devices, are currently lacking.
Conclusions
In the current era, with digital technologies being frequently used in all areas, it has become necessary to use them to improve students’ skills. Among these digital technologies, C-AL, AR-AL and VR-AL were the focus of this study. One of the main advantages of AR-AL and VR-AL systems is that they facilitate manual skill acquisition and provide instant feedback. When considering C-AL systems, even though they are proficient in knowledge transfer, they are inferior as compared to AR-AL and VR-AL systems in terms of manual skill acquisition. The biggest feature distinguishing AR-AL systems from VR-AL systems in education is that in the former case there is no disconnection from reality. AR-AL gives students the feeling of being close to a real environment, provides information on the current situation and guides them during dental treatment. Nevertheless, C-AL, AR-AL and VR-AL applications cannot be considered adequate replacements for the traditional preclinical instruction. While distance education is possible, we believe that the instructor and the student must be physically present in the same setting for learning to be most effective. Even though C-AL, AR-AL and VR-AL applications can be easily implemented into dental education, further studies are needed to elucidate the benefits of these emerging digital technologies to the learning processes.
Ethics approval and consent to participate
Not applicable.
Data availability
All data generated and/or analyzed during this study is included in this published article.
Consent for publication
Not applicable.