Abstract
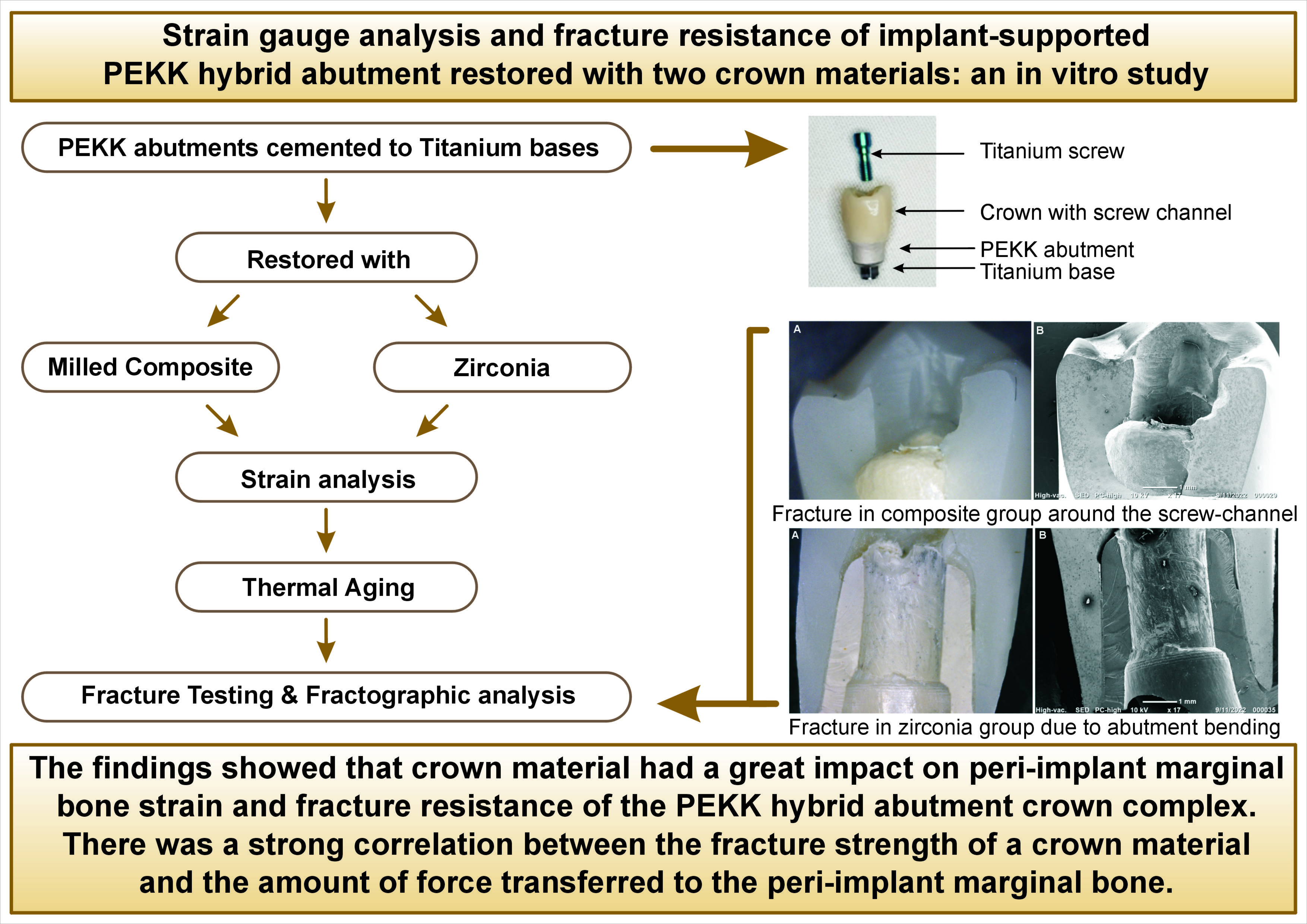
Background. Polyetherketoneketone (PEKK) was recently introduced as an alternative to titanium and ceramic implant abutments due to its apparent ability to dissipate excessive strain around dental implants. However, the biomechanical behaviors of implant abutment crown systems may change depending on the crown and abutment material combinations used.
Objectives. This study aimed to assess how the crown material affects strain generation and fracture resistance of PEKK hybrid abutment crowns.
Material and methods. Sixteen dummy implants (Ø 3.7 × 11 mm), simulating maxillary first premolars, were restored with 16 milled PEKK hybrid abutments and randomly categorized into two groups according to the crown material (n = 8): Group C, milled composite crowns cemented on PEKK hybrid abutments; and Group Z, ultra-translucent zirconia crowns cemented on PEKK hybrid abutments. Before thermocycling, a cyanoacrylate-base adhesive was used to position two strain gauges on buccal and lingual crestal bone surfaces, and a vertical load (100 N) was applied to the central fossa to record the strain generated. Then, all samples were thermocycled between 5°C and 55°C before being loaded to fracture on a universal testing machine. Modes of failure were observed under an optical microscope, and representative samples were examined using a scanning electron microscope. Independent t-tests were used for intergroup comparisons. The significance level was set at (p < 0.05) for all tests..
Results. The results showed a significant difference between both groups. The zirconia group recorded significantly higher strain and fracture resistance values than the composite group (p < 0.001). There was a positive correlation between the strain developed in peri-implant crestal bone and fracture resistance of the abutment crown complex.
Conclusions. Strains developed in both groups were within the acceptable clinical range. The crown material substantially impacted the strain and fracture of the PEKK hybrid abutment crown system.
Keywords: dental implants, zirconia, composite resins, implant abutments, polyetherketoneketone
Introduction
The high success rate of dental implants depends on good osteointegration and the overlying superstructure’s performance.1 However, dental implants may encounter biomechanical complications as they lack the dampening behavior of periodontal ligaments in natural teeth; thus, implants and natural teeth respond differently to typical masticatory forces.2, 3 Therefore, loading on dental implants should be controlled via the correct choice of implant, abutment, crown materials, and designs.3
Titanium abutments were the most commonly used implant abutments due to their superior biomechanical properties. However, their greyish color could be transmitted through the thin biotype gingiva and affect the final shade of ceramic restorations.4, 5 Therefore, dentists shifted to using more esthetic abutments and developed ceramic abutments. The first all-ceramic abutments used were zirconia due to their favorable esthetic and mechanical properties.6 However, they encountered a critical problem that involved fracturing of the apical part during screwing.7 Due to these problems, the concept of hybrid abutments was proposed.
Hybrid abutments consist of a non-metal part customized over a prefabricated titanium base, which provides a better esthetic restoration, and a titanium connection within the implant prevents fracture at the implant-abutment interface.8, 9 Modification of the non-metal part allows for better customization of the emergence profile and treatment of cases that require angulation correction. The presence of a cement layer between the titanium base and ceramic part acts as a weak link that decreases the possibility of screw looseness.10 These advantages demonstrate that hybrid abutments could be effective in implant rehabilitation cases.
Hybrid abutment restorations can be screw-retained, cement-retained, or screwmentable designs. Screw-retained restorations are easily retrievable for the repair of fractures and have insignificant biological complications as no excess cement remains in the sulcus.11, 12, 13 However, they carry a risk of screw loosening or ceramic fracture.14, 15 Cement-retained restorations can compensate for implant position discrepancies and have improved esthetics and better control of occlusion. The cement layer acts as a shock absorber that uniformly transfers loads to the implant prostheses bone complex.12, 13 Nevertheless, there is a risk of peri-implantitis due to excess cement not being adequately removed from the soft tissue.15, 16 The screwmentable design combines the benefits of both designs (screw-retained and cement-retained) by allowing intraoral adjustments of the crown and contact area during restoration delivery without multiple removal and replacement of the screw, and the crown can be extraorally cemented on the abutment, allowing excess cement to be easily removed.13, 17, 18
Different materials are available for use in hybrid abutments. Conventional ceramics, such as oxides (alumina, zirconia) and glass (lithium disilicate), can produce highly esthetic hybrid abutments; however, they have a high incidence of failure when used over implants, possibly caused by their rigidity.19 While searching for a restorative material with a lower elastic modulus, high-performance polymers called polyaryletherketone (PEKK) have been developed.5, 20
Compared to titanium, high-performance polymers showed a decreased marginal bone loss and soft tissue recession during the initial healing phase by reducing the occlusal loads reaching the bone.21, 22 Moreover, a previous study revealed that unpolished polymers had a lower surface roughness than zirconia abutments, which will provide less biofilm accumulation and better soft tissue attachment; however, they found that the flexibility of these materials may cause a higher strain in the implant and peri-implant bone.23
PEKK is a high-performance polymer claimed to have good shock absorption properties and high compressive strength due to the additional ketone group in its structure.24 Nevertheless, PEKK has a monochromatic opaque appearance and is usually combined with an overlying esthetic crown. The manufacturer recommends restoring PEKK abutments with either composite or ceramic crowns.25 Composite resin has a low elastic modulus that could be beneficial over implant restorations. Milled composite crowns showed no polymerization shrinkage and enhanced mechanical and wear properties over direct composite layering.26, 27 On the other hand, some authors claim that using a rigid crown material like zirconia would decrease the forces transmitted to the abutment and bone.28
Several tools were used in the literature to record the strain around dental implants, such as finite element analysis,29, 30 photoelasticity,31 and strain gauges.32, 33 Strain gauges are electric resistors that alter the resistance created in their current under slight deformation. They can be used to assess strain developed in prostheses, implants, and teeth in vivo and in vitro.32 Moreover, using a strain gauge to evaluate the strains induced in the implants is clinically reliabile.34
Due to the multilayer nature of the implant superstructure, the biomechanics of the implant system can vary depending on the crown and abutment material combinations, so the current study aimed to investigate the peri-implant crestal bone strain and fracture resistance of composite and zirconia crown materials when combined with PEKK hybrid abutments and fabricated as screwmentable restorations.
The null hypothesis of the present study stated that neither peri-implant marginal bone strain nor fracture resistance of the PEKK hybrid abutment crown complex would be affected by the crown material.
Material and methods
A power analysis was designed based on the results of a previous study.35 By adopting an alpha (α) level of 0.05 (5%), a beta (β) level of 0.2 (20%) (i.e., power = 80%), and effect size (d) of (1.65), the minimum required sample size (n) was seven per group. The sample size calculation was performed using G*Power version 3.1.9.4.
Sixteen dummy implants, Ø 3.7 x 11 mm (JDentalCare s.r.l, Modena, Italy) resembling the average implant dimensions in the premolar region,36, 37 were placed perpendicularly in self-cured resin (Technovit 4000, Heraeus Kulzer, Hanau, Germany), with an elastic modulus (12 GPa) that approximates that of trabecular bone (18 GPa). A paralleling device (Dremel® Moto-Tool Model 395, WI, USA) was used to maintain the implant in place until the resin was completely set.
A titanium base (JDentalCare s.r.l, Italy) with platform switching, 0.5 mm shoulder finish line, and 3 mm height was hand screwed to the dummy implant. The screw access channel was sealed with wax, and the titanium base was then sprayed with light-reflecting powder (Occlutec spray, Renfert, Hilzingen, Germany) to facilitate the scanning procedure. Scanning employed a desktop scanner (Medit T710, Medit Corp, Seoul, Korea). Computer-aided design (CAD) software (Exocad GmbH, Version 3.0, Darmstadt, Germany) was used to design the abutments and crowns. The abutment dimensions were adjusted following Taha et al.38 The crowns were designed with a screw channel within the occlusal surface and adjusted according to the average dimensions of a maxillary first premolar, with a crown height of 11.5 mm and buccolingual width of 6.5 mm.39 Then STL files of the design were sent from the CAD software to computer-aided manufacturing (CAM) software. A five-axis milling machine (Glidewell Dental Labs, VHF Camfacture AG, Ammerbuch, Germany) was used to mill the abutments and the crowns.
The abutments were divided into two groups (n=8) according to the crown material: milled composite (Group C) and zirconia (Group Z). PEKK blanks (Pekkton® ivory, Cendres+Métaux, Milano, Italia) were used to fabricate the PEKK abutments for both groups. Composite blocks (Brilliant Crios, Coltène AG; Altstätten, Switzerland) were used to fabricate the composite crowns in Group C. Zirconia blanks (UTML, Kuraray Noritake, Japan) were used to fabricate zirconia crowns in Group Z.
After milling, the PEKK abutments were finished and polished using a specific kit (BioHPP polishing kit, Bredent, Germany), while zirconia crowns were sintered and glazed using a zirconia sintering furnace (inFire HTC speed, Sirona Dentsply, Bensheim, Germany) at 1550°C for two hours. For the composite crowns, finishing and polishing were done using a two-stage polishing system (Diatech polishing kit, Coltène AG; Altstätten, Switzerland). The titanium bases, milled abutments, and crowns were cleaned in an ultrasonic bath, degreased with ethanol, and then treated according to the manufacturer’s recommendations, as shown in Table 1.
The screw channel was sealed with Teflon tape, and Multilink Hybrid Abutment self-cured resin cement (Ivoclar Vivadent; Schaan, Liechtenstein) was applied to the titanium bases. The pretreated abutments were cemented to their corresponding titanium bases. The abutments were first seated with finger pressure and then left to set under a 5 Kg load.
The intaglio surfaces of the crowns were sandblasted and treated with universal primer (Monobond Plus primer, Ivoclar Vivadent; Schaan, Liechtenstein), as mentioned in Table 1. An adhesive resin cement (Breeze™, Pentron Clinical, CA, USA) was used to cement the crowns to the abutments. A static load was applied over the cemented crowns for five minutes. The prostheses were tightened to the implants using a screwdriver and torque wrench under 30 Ncm to avoid preload screw loosening then they were retightened after ten minutes. Teflon tape was placed to seal the screw channels, and then a light-cured composite (Filtek™ Z250) was applied.
Two strain gauges (Kyowa Kirin, Koyowa, Japan) (Ø1 mm) were positioned on the buccal and lingual crestal surfaces of the bone analog with a delicate layer of cyanoacrylate-base adhesive cement (Super glue, China).
Before thermocycling, a universal testing machine (LLOYD Universal Testing Machine, UK) applied a vertical load (100 N) onto the central fossa to record the strain generated in the peri-implant crestal bone. Tin foil was fixed between the loading piston and the specimen to ensure equal strain distribution.
All samples were artificially aged in a thermocycler (Thermocycler, SD Mechatronik, Feldkirchen-Westerham, Germany) to a total of 5000 thermal cycles between 5°C and 55°C with a dwell time of 30 seconds and a transfer time of five seconds, which is equivalent to six months in the oral environment.37
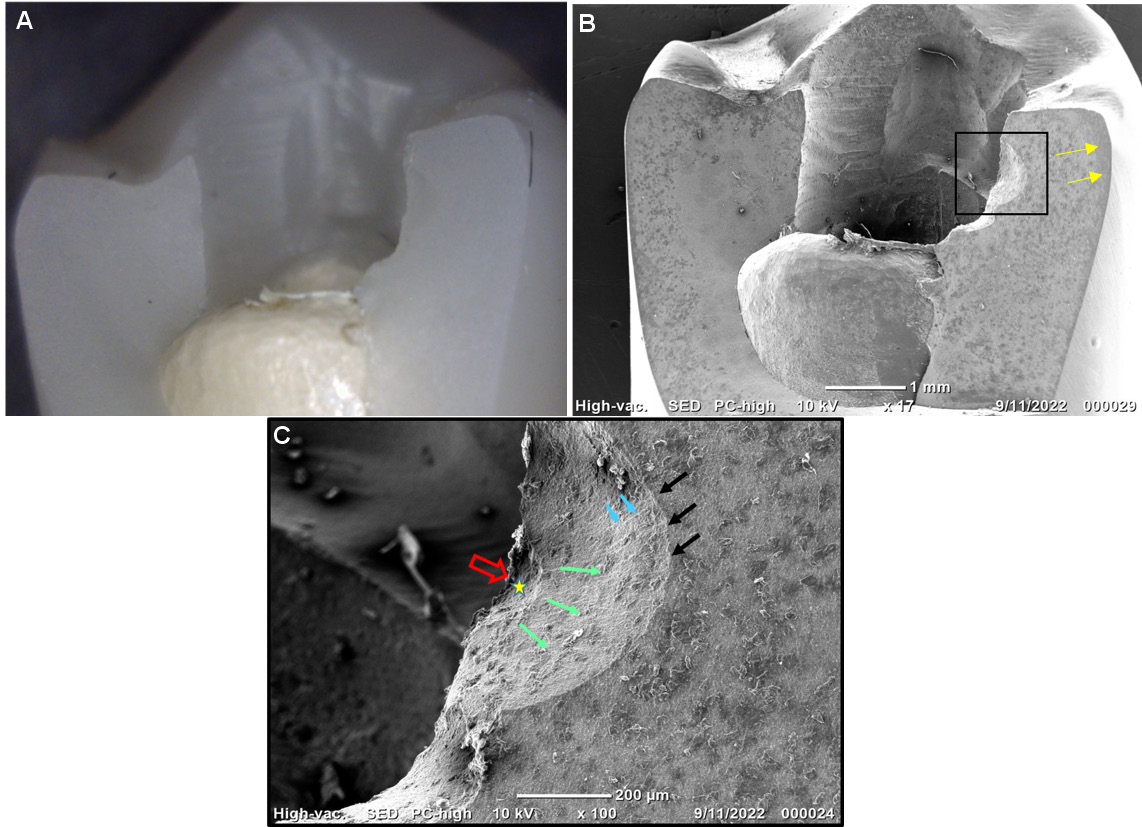
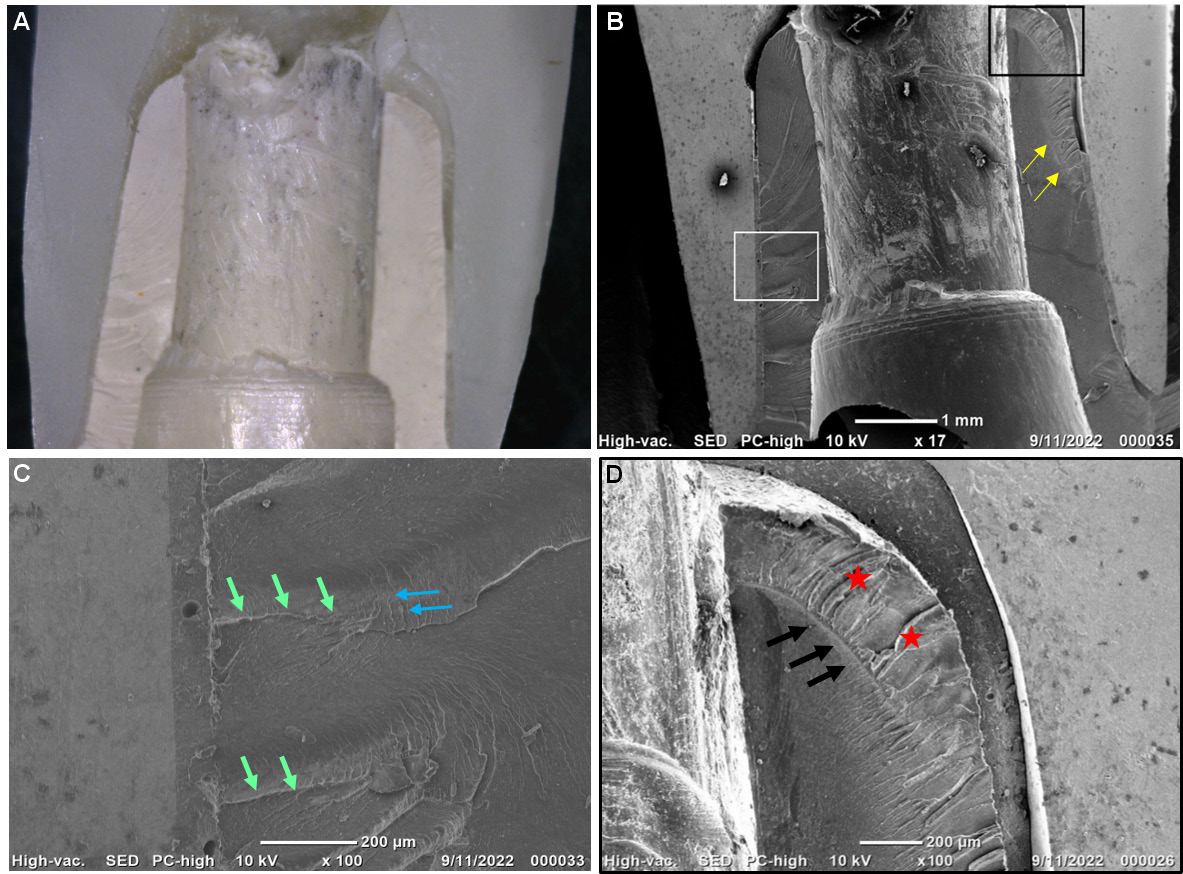
The specimens were loaded with vertical loads (1 mm/min) onto the central fossa until fracture.40 The fractured specimens were examined with an optical microscope (Dino-Lite Electronic Corp., Taiwan) at 35× magnification to analyze the mode of failure. Representative specimens were sputtered with gold for five minutes and observed with a scanning electron microscope (SEM) (Neoscope (JCM-6000 Plus), JEOL, Japan) at 17× magnification and then at 100× magnification to detect the cause of fracture.
Statistical analysis
Numerical data were explored for normality by assessing the data distribution using a Shapiro-Wilk test. The data were normally distributed and were represented as mean and standard deviation (M ±SD). Independent t tests were used for intergroup comparisons. Pearson’s correlation coefficient was used to study the correlation between fracture resistance and strain. The significance level was set at p < 0.05 for all tests. Statistical analysis was performed with R statistical analysis software version 4.1.3 for Windows (R Core Team, 2022).
Results
The results revealed that the zirconia group had significantly higher strain and fracture resistance values than the composite group (p < 0.001) (Table 2).
There was a strong positive correlation between strain falling on the implant surrounding marginal bone and the fracture resistance of the implant superstructure. The relationship was statistically significant (r = 0.970; p < 0.001).
Failure modes were classified as Class I: a fracture in the crown only, Class II: a fracture in the abutment only, Class III: a fracture in the crown and abutment, and Class IV: screw fracture and implant deformation.41 In Group C, Class I failure was observed in all specimens without fractures or deformations within the abutments (Figure 1). For Group Z, failures were more catastrophic and were within the abutments and crowns (Class III). The failure exhibited bending and deformation of the abutment and vertical fracture of the abutment and crown (Figure 2).
Fractographic analysis for Group C under SEM showed that the fracture originated from the screw channel and propagated as small cracks within the crowns without any cracks or plastic deformation in the PEKK abutments (Figure 1B,C). In Group Z, multiple cracks and signs of bending were observed within the PEKK abutments (Figure 2B,C,D).
Discussion
There has been much debate on whether rigid or soft implant crown material will transfer lower strains to the implant-bone surrounding,26, 27, 28, 38 so this study was based on biomechanical evaluation of peri-implant cervical bone strain and fracture resistance of implant-supported prostheses, fabricated as screwmentable restorations, using two crown materials with substantial differences in their mechanical properties.
The null hypothesis of the study was rejected since strain analysis results revealed that Group C had significantly lower microstrain values than Group Z. The statistical difference could be attributed to the difference in elastic modulus between the crown materials (about 10 GPa for composite and 200 GPa for zirconia). The high elastic modulus of zirconia (200 GPa) lowered its damping behavior, which transmitted high forces to the substructure and bone. This agrees with Datte et al.,42 who stated that increasing crown material stiffness increases the generated strain in the implant surrounding bone while decreasing the developed strain in the restoration itself.
Despite the strain analysis results, the two groups had a similar clinical effect on the peri-implant bone strain, as all values were within the clinically accepted range for microstrain (50-3000 µm) that enhances bone formation and prevents its overload or disuse.43 The resin-based crown material acts as a shock absorber for the occlusal loads, making the strains developed in the bone more bearable.38 For the zirconia group, combining a ceramic crown with a high elastic modulus in contact with the applied load and a material with a lower elastic modulus below the crown mimics the enamel and dentine behavior in natural teeth.44 As such, even with the high elastic modulus of zirconia crowns, the zirconia-PEKK combination generated strains within the generally accepted limits. Another explanation suggests that the intermediate resilient cement layer improves the dampening behavior of the rigid crown materials, leading to better dissipation of the occlusal forces.38
Fracture resistance results support the first finding in the present study, as the material with high elastic and flexure modulus could not be easily deformed under loads. However, it would transfer high strains to the underlying structure, which was supported by the SEM findings showing cracks in the underlying PEKK abutments in Group Z (Figure 2).
On the other hand, the material with low flexure and elastic modulus (composite) deformed under the applied load, preventing it from reaching the underlying abutment and implant-bone surroundings, so no deformations were observed in the composite group (Figure 1). This was in line with Bijjargi and Chowdhary,45 who concluded that using crown material with a low elastic modulus reduces the strains transferred to the underlying structure by absorbing more energy from the applied load while transmitting less energy to the implant, abutment, and bone.
Another explanation for the lower fracture values in Group C was the presence of the screw access channel within the crown. The screw access channel disrupted the structural integrity of the crown material, affecting its fracture resistance, particularly when the crown was formed of a material with a weak microstructure like composite. This agrees with a previous finding in a study by Preis et al.,35 who found that screw channels might affect the continuity of resin-based occlusal material and lead to fracture. Our interpretation was also confirmed by the SEM findings, as the fracture origin for Group C was found to be along the screw channel, with needle-like cracks, called hackle lines, extended downward, which indicated the direction of crack propagation (Figure 1). Therefore, the fracture originated and propagated from the screw channel.
On the other hand, in Group Z, stiff zirconia crowns (200 GPa) transferred higher strains to PEKK abutments with an elastic modulus of 5 GPa, which led to bending and deformation of the abutments and so concentrated high tensile strains on the overlaying brittle zirconia crowns and caused crown fracture. This was confirmed by the SEM findings (Figure 2), which revealed signs of plastic deformation and bending in the PEKK abutment with the tension surface towards the zirconia superstructure and the compression surface inside.
The plastic deformations and bending occurred despite the PEKK microstructure containing an extra ketone group. However, this might be due to the fact that PEKK does not contain reinforcing elements to increase its stiffness (modulus of elasticity) and resistance to bending. The titanium oxides included in PEKK only increase their wear resistance,46 which explains why when zirconia crowns transferred high strains to the PEKK abutments, they showed multiple signs of bending and plastic deformation. This finding was consistent with a previous study designed by Türksayar and Atsü,47 showing that unmodified PEKK implant abutments had fracture load values less than those made of modified PEKK; however, they only tested one crown material.
Ghodsi et al.,48 classified the fracture modes into favorable and unfavorable failures. A favorable failure occurs within the crown material while the abutment remains intact. An unfavorable failure is a fracture within the abutment that necessitates restoration or replacement. In the present study, despite Group Z having higher fracture values than the indirect composite, it showed more unfavorable catastrophic fractures than the composite group. However, having a customized abutment made from a material with a low elastic modulus protected the implant and titanium bases from being deformed or fractured in both groups. The indirect composite fracture was in the form of cracks or chipping of the composite crown without any fracture in the abutment, resulting in a more favorable mode of failure with an easy repair advantage. Nevertheless, composite resins are more prone to material wear, color instability, and loss of surface gloss than zirconia.19, 49
Statistical analysis of the results clarified a strong positive correlation between the fracture resistance of the implant crown material and the microstrain produced in the implant surrounding the marginal bone. This might be due to the fact that both the fracture resistance of a material and its damping behavior are strongly related to Young’s modulus.
Concerning the above, it could be hypothesized that stiff crown materials have high fracture resistance, increasing their ability to withstand high occlusal forces. However, these high loads could be transmitted from the crown to the underlying PEKK abutment and cervical peri-implant bone, although, in the current study, the loads were within the acceptable physiological range. Moreover, using a hybrid abutment with a low elastic modulus (PEKK) under rigid crown material could be beneficial as it would protect the underlying titanium bases, implant fixture, and peri-implant bone from being overloaded.
A limitation of the current study was that the tested specimens did not undergo cyclic loading, so further studies are required after mechanical aging.
Conclusions
Based on the findings of the present study, strains generated in both zirconia-PEKK hybrid abutment crowns and milled composite-PEKK hybrid abutment crowns were within the acceptable clinical range. Also, zirconia-PEKK hybrid abutment crowns can be used safely in the upper premolar region; however, milled composite-PEKK hybrid abutment crowns may cautiously serve in this region. Crown material had a statistically significant impact on the peri-implant marginal bone strain and fracture resistance of the PEKK hybrid abutment crown complex. Furthermore, there was a strong correlation between the fracture strength of crown material and the amount of force transferred to the peri-implant marginal bone.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.