Abstract
Background. Splenectomy is performed in β-thalassemia cases due to the destruction of red blood cells (RBCs), and the consequent splenomegaly.
Objectives. The aim of the present study was to compare oral health and the caries risk between β-thalassemia patients with or without splenectomy, using the Cariogram.
Material and methods. In a cross-sectional study carried out in both the Maternity and Children Hospital and the King Fahad Hospital, Al-Madinah al-Munawwarah, Saudi Arabia, interviews, salivary sampling and oral clinical examinations were performed on 60 children and adolescents with β-thalassemia major (mean age: 13 ±3 years; 65% with splenectomy). The Cariogram program was used to calculate the caries risk. The main outcome measures were the number of decayed, missing due to caries, and filled teeth (DMFT), plaque and gingival indices, and the caries risk.
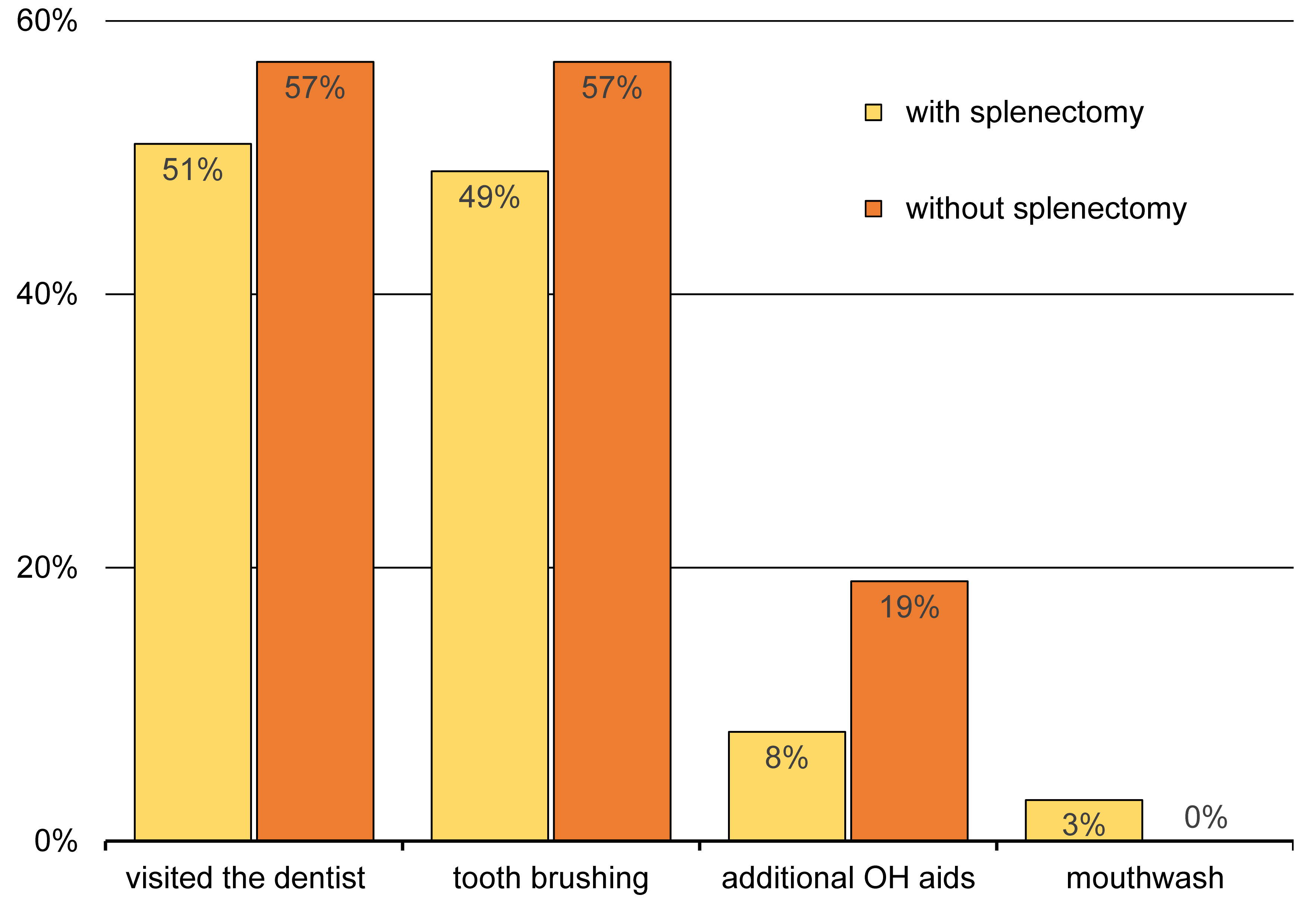
Results. Of individuals with and without splenectomy, tooth brushing was reported in 49% and 57%, respectively (p > 0.05). Individuals with splenectomy had lower plaque and gingival bleeding scores (p ≤ 0.05). Salivary secretion was identical in both groups. Caries experience and the caries risk were higher in individuals without splenectomy (p > 0.05 and p ≤ 0.05, respectively).
Conclusions. Within the study limitations, children and adolescents with β-thalassemia had high plaque and gingival bleeding scores, as well as caries experience and caries risk. Those with splenectomy demonstrated lower figures than those without. Individuals with β-thalassemia, particularly those with splenectomy, need to be educated about the oral side effects of the disease and its treatment.
Keywords: oral health, splenectomy, caries risk, beta thalassemia
Introduction
Beta-thalassemia is a common genetic disorder distinguished by the absent or decreased synthesis of globin protein chains, particularly the beta and alpha chains, resulting in a reduced production of hemoglobin and hypochromic microcytic anemia.1 Spleen enlargement, abnormal red blood cells (RBCs), iron overload, and other changes occur because of the increased rate of hemopoiesis observed in a number of conditions, including β-thalassemia.2, 3
It is well-established that individuals with β-thalassemia are at a higher risk of infection, particularly those who have undergone splenectomy.1 Regarding oral health, several studies have observed a high dental caries index in β-thalassemia patients,4 which may be attributed to several factors, including the hematologic condition itself, medications, the altered tooth morphology, and the modified salivary composition.5 Other oral manifestations related to periodontal health, occlusion and the maxillary growth have also been reported.6, 7, 8
As dental caries is known to be multifactorial in nature, different factors, such as the systemic condition of the individual, may contribute to the disease.9 Thus, the multifactorial management of dental caries has continuously been advocated and recommended in the literature.10 Moreover, assessing the individual’s caries risk plays a vital role in its prevention and management.11, 12, 13 Several methods and tools have been used for multifactorial caries risk assessment, one of which is the Cariogram,14 a computer program that calculates the relationship between dental caries and many possible protective and invading factors in an attempt to illustrate the caries risk and provide feasible explanations and recommendations for the individual patient.14
To date, no studies have investigated the association between splenectomy and the oral health and the caries risk in patients with β-thalassemia. Therefore, the present study aimed to evaluate the oral health and caries risk profiles in β-thalassemia patients, using the Cariogram, and to compare them in patients with or without splenectomy.
Material and methods
Study design and sample
This observational cross-sectional analytical investigation was approved and registered by the Taibah University College of Dentistry Research Ethics Committee (approval No. TUCDREC/20180107/Qarah) and the Institutional Review Board at the General Directorate of Health Affairs in Al-Madinah al-Munawwarah, Saudi Arabia (approval No. 120–07/02/2018). The study followed the Declaration of Helsinki guidelines with regard to involving human participants15 and the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist for reporting observational studies.16
The study population comprised children with β-thalassemia major attending the hematology/oncology center at the Maternity and Children Hospital and adolescents with β-thalassemia major attending the specialized clinic at the King Fahad Hospital in Al-Madinah al-Munawwarah, Saudi Arabia.
Study outline
All participants underwent a personal interview, had their saliva sampled and were subjected to an oral clinical examination during routine blood transfusion appointments. Those who could not be examined during the same visit were given an appointment at the Taibah University Dental College and Hospital. The interview collected general background information, including age, gender, nationality, oral hygiene practices, the type of thalassemia, the medications used, a history of splenectomy, and other health-related aspects. Child participants had their guardians answer the interview questions.
Saliva sampling
The participants washed out their mouths with distilled water before starting the procedure. Unstimulated saliva was collected by a standard spit method, with the participant in an upright sitting position and inclined to the front, spitting for 5 min into a graded plastic container.17 The samples were used to measure the salivary secretion rate of each participant. Sampling was not possible in 2 of the participants.
Oral clinical examination
Oral clinical examinations followed standard infection control precautions, were performed on a portable dental chair under an optimal light source, and utilized a graded periodontal probe (Hu Friedy, Chicago, USA), a mouth mirror and sterile cotton pads. The recorded parameters included the number of decayed, missing due to caries, and filled teeth (DMFT), the gingival index (GI),18 and the plaque control record (PCR).19 The DMFT was recorded for all teeth, and GI and PCR were registered at 4 tooth sites (mesial, distal, buccal, and lingual). Two crossed upper and lower quadrants were selected for GI and PCR by coin flip.
Caries risk assessment
The Cariogram software, v. 3.0 (Malmö University, Sweden) assessed the participants’ caries risk. The risk is calculated by entering 9 related factors into the software, including caries experience, systemic diseases, the plaque score, diet content, diet frequency, the fluoride program, salivary secretion, buffer capacity, and the salivary Streptococcus mutans counts.14 To compensate for a lack of laboratory analysis, a reduced Cariogram model was adopted, where variables that relied on the salivary analysis were excluded.20 Upon variable entry, the Cariogram produces a graphical pie chart that shows how the entered variables interact. The green sector of the pie chart, named “Actual Chance (%) to Avoid New Cavities” (Chance-AC), reflects the individual’s caries risk. The smaller the green sector, the higher the risk of developing new caries lesions in the future.14
Statistical analysis
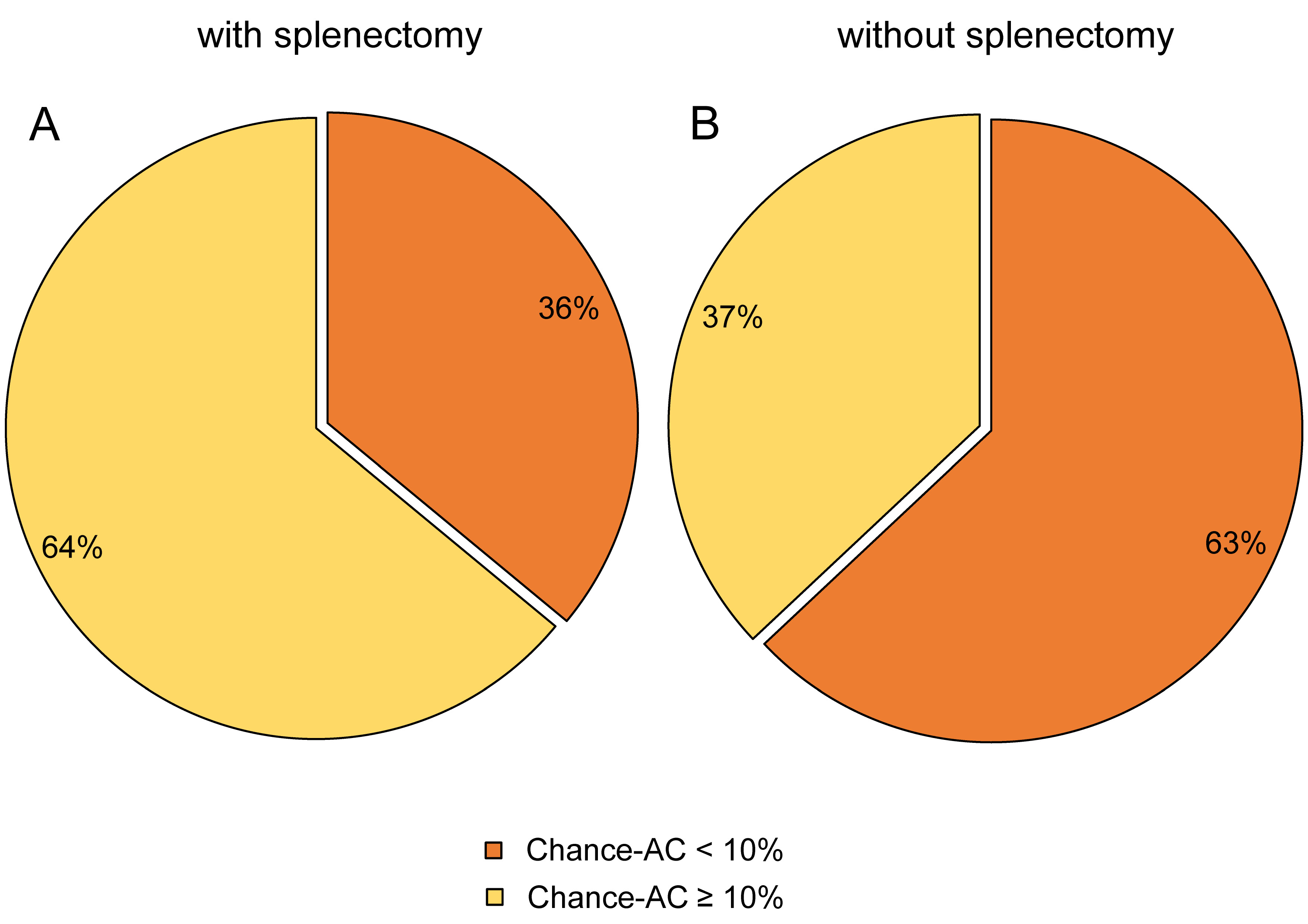
Descriptive statistics in the form of mean and standard deviation (M ±SD) were used to describe continuous variables, and frequencies represented categorical variables. Given the unequal data distribution, the Mann–Whitney U test compared differences in continuous outcome variables between individuals with or without splenectomy, while the χ2 test was used for categorical variables. As most of the study participants fell within the ‘very high’ caries risk category according to the Cariogram, i.e., Chance-AC = 0–20%,21 a decision was made to highlight those with Chance-AC <10% as the ‘highest’ caries risk among individuals with or without splenectomy. A p-value ≤0.05 was considered statistically significant. Data was analyzed using IBM SPSS Statistics for Windows, v. 20.0 (IBM Corp., Armonk, USA).
Ethical considerations
Written informed consent was obtained from the participants (or their parents) before their inclusion in the study. The purpose of the study was explained to each participant, and they were assured that participation was voluntary, with no negative repercussions in terms of the quality of health care offered due to not participating. The participants were also assured that all information would be kept confidential and would only be used for scientific purposes. They were informed of any need for treatment based on the study findings.
Results
A total of 60 individuals with β-thalassemia major were involved in this study, including all children followed up at the Maternity and Children Hospital (n = 40; 67%) and adolescents attending the clinic at the King Fahad Hospital (n = 20; 33%). The mean age was 13 ±3 years; 53% of the participants were males and 47% were females. Thirty-nine (65%) participants had undergone splenectomy (Table 1).
Of the individuals who had undergone splenectomy, only 49% reported brushing their teeth, while 57% of those without splenectomy brushed their teeth (p > 0.05) (Figure 1). High dental plaque and gingival bleeding scores were recorded in both groups, with individuals without splenectomy demonstrating significantly higher scores (p ≤ 0.05) (Table 1).
Salivary secretion was within the normal range, and identical in both groups (p > 0.05) (Table 1). Individuals without splenectomy a higher DMFT score than those who had undergone splenectomy (5.5 ±5 vs. 4.5 ±5, p > 0.05) (Table 1).
Both individuals with and without splenectomy demonstrated ‘very high’ caries risk profiles, as illustrated by the Cariogram, with a low Chance-AC of 17 ±12% and 14 ±14%, respectively (p ≤ 0.05) (Table 1). Seventy-six percent of the total sample had Chance-AC ≤ 20%, while 45% had Chance-AC < 10% (data not shown). Figure 2 presents the distribution of individuals from both groups according to Chance-AC <10% and ≥10%, with more individuals from the group who had not undergone splenectomy falling into the higher risk category (p ≤ 0.05).
Discussion
In this study, around half of the participants with β-thalassemia major visited the dentist and brushed their teeth, with no significant differences observed between those with or without splenectomy. These alarming figures may be due to the fact that patients with β-thalassemia (and their families) are often occupied with dealing with the disease and its devastating repercussions, which may lead to oral health negligence.22 Moreover, certain oral features in individuals with β-thalassemia, such as tooth malposition and malocclusion, may hinder the maintenance of good oral hygiene.7, 23
The present study demonstrated that β-thalassemia patients had high plaque and gingival bleeding indices, which is in line with the literature on oral findings in people with β-thalassemia major, and is likely related to local factors, such as malocclusion, protruded front teeth, and consequently, an anterior open bite and xerostomia.24
The salivary flow rate was generally within the normal range, with no significant differences between individuals with or without splenectomy, which was contrary to expectations, since individuals with β-thalassemia usually demonstrate iron deposits due to iron overload,25 related to a decreased salivary flow rate, pain and swelling.26 However, a histological study involving 15 adults with thalassemia failed to demonstrate a clear correlation between salivary secretion impairment and the destruction of the salivary glands by iron deposition, lymphocyte infiltration and fibrosis, warranting further research in this area.27
The current study is the first to assess the caries risk in individuals with β-thalassemia. As dental caries is a multifactorial disease, the Cariogram computer software was used to estimate the risk by illustrating how different caries-related factors interact.14 Individuals with β-thalassemia major demonstrated high caries risk, which may be attributed, in part, to the high caries experience observed. Other contributory factors include improper dietary habits, bone deformities, and lack of appropriate oral health-related knowledge.23 In addition, social status reflects significantly on oral health, and many of these families could not afford the high costs of dental treatment.28
Patients with β-thalassemia major who had undergone splenectomy had significantly lower plaque and gingival bleeding index scores, a lower DMFT score, and lower caries risk than those without splenectomy. Beta-thalassemia patients who undergo therapeutic splenectomy due to massive splenomegaly are more susceptible to bacteremia and the post-splenectomy sepsis caused by gram-negative bacteria.23 With an increased chance of infection, β-thalassemia patients who undergo splenectomy receive antibiotic therapy for life, usually in the form of oral penicillin, with some also receiving a combination of different prophylactic injections pre-operatively.29, 30 This may explain the differences in oral health findings between β-thalassemia patients with and without splenectomy. The effects of penicillin and antibiotics on dental caries in general have been reported since the 1960s.31 Similarly, periodontal disease, induced mostly by microbial plaque, has been treated by antibiotics alone or as adjuncts to mechanical plaque removal.32 However, antibiotic administration for oral diseases remains debatable due to obvious side effects and the risk of antibiotic resistance, and is limited to very specific cases.
Limitations
The small sample size may raise questions regarding the representativeness of the study findings. However, this could not be avoided, as individuals with β-thalassemia regularly visiting the clinic for follow-up represent a limited population. The intention was to include all possible patients from the database, but this was not achieved due to unprecedented circumstances. Nevertheless, findings from the current investigation may add significant value to the literature related to such a rare disease.
A reduced Cariogram model was used to assess the caries risk of the studied sample. It can be argued that each factor entered into the Cariogram software is significant for accurately determining the individual’s risk. However, using a reduced Cariogram has been reported in the literature33 and can be of practical use in cases with limited laboratory resources.
Conclusions
Within the study limitations, it can be concluded that individuals with β-thalassemia major had high plaque and gingival bleeding scores, caries experience, and risk of future caries, as shown by the Cariogram. Individuals who had undergone splenectomy presented significantly lower values than those without splenectomy.
Practical significance
All individuals with β-thalassemia, with or without splenectomy, should have regular dental visits to carry out appropriate preventive and therapeutic measures that address the causative and contributory factors of oral disease. Affected children and their parents need to be supported, educated, and made aware of the side effects of the disease and its treatment, including subclinical or masked oral health conditions.
Ethics approval and consent to participate
The study was approved and registered by the Taibah University College of Dentistry Research Ethics Committee (approval No. TUCDREC/20180107/Qarah) and the Institutional Review Board at the General Directorate of Health Affairs in Al-Madinah al-Munawwarah, Saudi Arabia (approval No. 120–07/02/2018). All participants or their parents provided written informed consent.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.