Abstract
Background. Platelet-rich fibrin (PRF) membranes are known to enhance wound healing after periodontal surgeries and dental implant procedures.
Objectives. The aim of the present study was to examine the effect of PRF on soft tissue healing and the crestal bone level (CBL) around non-submerged dental implants.
Material and methods. A total of 40 patients, aged 20–60 years, with partially edentulous posterior mandibular sites were divided into 2 groups of 20 patients each: group I received non-submerged implants with a PRF membrane; and group II was treated with non-submerged implants alone. The examined parameters included the modified plaque index (mPI), the gingival index (GI), the width of keratinized tissue (WKT), the thickness of keratinized tissue (TKT), and CBL, assessed using digital intraoral periapical radiography (IOPA). All parameters were measured at baseline (immediately post-op), and at 3-month and 6-month follow-ups.
Results. In comparison with baseline, statistically significant increases in WKT and TKT were observed in both groups at 3 and 6 months post-op (p < 0.05). Also, significant gains were noted in group I vs. group II (p < 0.05). The CBL increased significantly in both groups at 3 and 6 months post-op (p < 0.05), with no remarkable differences from 3 to 6 months. A decreased CBL was observed in group I vs. group II at the 3- and 6-month intervals (p < 0.05).
Conclusions. The PRF membrane enhances peri-implant tissue wound healing, with gains in soft tissue width and thickness around non-submerged implants.
Keywords: dental implants, wound healing, platelet-rich fibrin membrane
Introduction
Replacing missing teeth in edentulous sites with implants is the preferred and pragmatic alternative to fixed partial dentures and complete dentures.1 With an impressive success rate of 90–100% for implant survival and prosthetic outcomes, a single-tooth endosseous implant is the most widely used form of dental implant.2
The initial concept for implant installation was a two-stage surgical intervention, which comprised a phase of submerged healing to achieve optimal osseointegration and implant longevity.3 However, studies by Ferrigno et al. (2002) and Romeo et al. (2004) showed that satisfactory osseointegration could be achieved, with success rates being comparable to submerged implants, by using a single-stage procedure that does not require the implant to be submerged.4 The replacement procedure using a non-submerged implant involves the placement of the implant and the transmucosal abutment during the same surgery; the abutment, while uncovered in the oral cavity, heals and is gradually loaded to ensure osseointegration.5 Non-submerged implants allow early implant loading, avoiding a second surgery and simplified prosthetic handling, with no subgingival micro-gaps between the implant and the abutment.5, 6
Over time, autologous platelet derivatives, such as platelet-rich fibrin (PRF) have been used to augment soft tissue healing and rapid osseous regeneration by enhancing the chemotaxis, angiogenesis, mitosis, and proliferation of potent stem cells.7, 8 The physiological architecture of PRF, a second-generation platelet derivative, comprises a fibrin matrix, and platelets, leukocytes, cytokines, and growth factors. Therefore, PRF is used as an autologous barrier membrane in a variety of clinical procedures, such as extraction socket healing and sinus lifting, in implant dentistry, and for treating intraosseous periodontal defects and gingival recessions; it is also a novel treatment option for various mucogingival surgeries.9, 10
A prerequisite for the longevity of an osseointegrated implant is its mechanical stability, which, in turn, depends on the quality and quantity of the surrounding soft tissue and bone.11 The effect of PRF on the existing osseous structure and gingival architecture around non-submerged implants is not well documented.
According to our null hypothesis, there is no additional benefit with the PRF usage regarding the improvement of the soft and hard tissue parameters. Therefore, the present study aimed to examine and compare how PRF affects soft tissue healing and the crestal bone level (CBL) around a non-submerged implant.
Material and methods
Sample size calculation
For the sample size estimation, the G*Power software, v. 3.1.0 (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower), was used. When the study power was set at 80%, with an alpha error of 5% and an effect size of 0.25%, the estimated sample size was 18. A sample of 20 was used to provide more robust results. As such, 40 implants (20 in each group) were placed.
Study design
This double-blind prospective randomized controlled clinical trial was conducted between May 2018 and April 2019. Patients with partially edentulous posterior mandibular sites were selected from the outpatient clinic of the Department of Periodontology, Sibar Institute of Dental Sciences, Guntur, India. All potential participants received information about the study design, and written informed consent was obtained from those willing to participate. A total of 40 patients (23 males and 17 females) were included in the study. The institutional ethics committee approved the study (Ref. No. 111/IEC SIBAR/Lr/17), and it was registered with the Clinical Trials Registry – India (CTRI) (No. 2018/05/013713).
Randomization and allocation
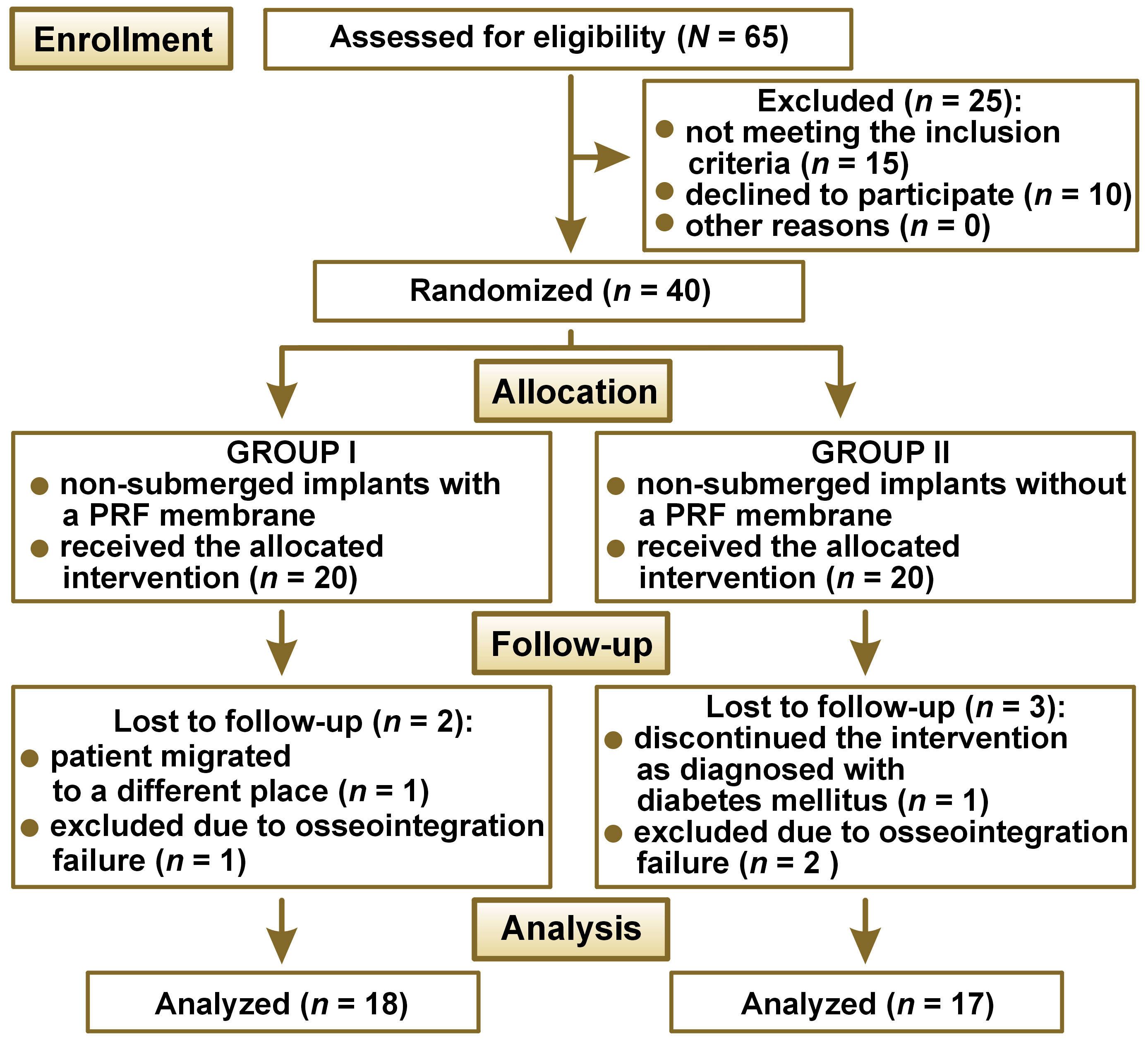
The 40 patients were randomly divided into 2 groups of 20 participants: group I received non-submerged implants (cylindrical implants with a parallel body and a core design) with a PRF membrane; and group II received non-submerged implants alone. Randomization was carried out by an independent researcher (C.A.), who was unaware of the study design, by using a computer-generated code at a 1:1 ratio. Allocation was concealed in opaque envelopes labeled with patient study numbers, which were opened before the surgical procedure. The study followed the CONSORT (Consolidated Standards of Reporting Trials) guidelines, and the CONSORT flow diagram is shown in Figure 1.
Inclusion and exclusion criteria
Patients aged 20–60 years with a partially edentulous posterior mandibular site containing sufficient bone to allow implant installation, without the need for a ridge augmentation procedure were included in the study.
Systemically compromised patients or those taking any medications/drugs that may affect the treatment outcome, patients with a history of osteoporosis, patients with a history of tobacco use, those unable to perform routine oral hygiene procedures, and those with a history of parafunctional habits, such as bruxism, were excluded from the study.
Clinical and radiographic parameters
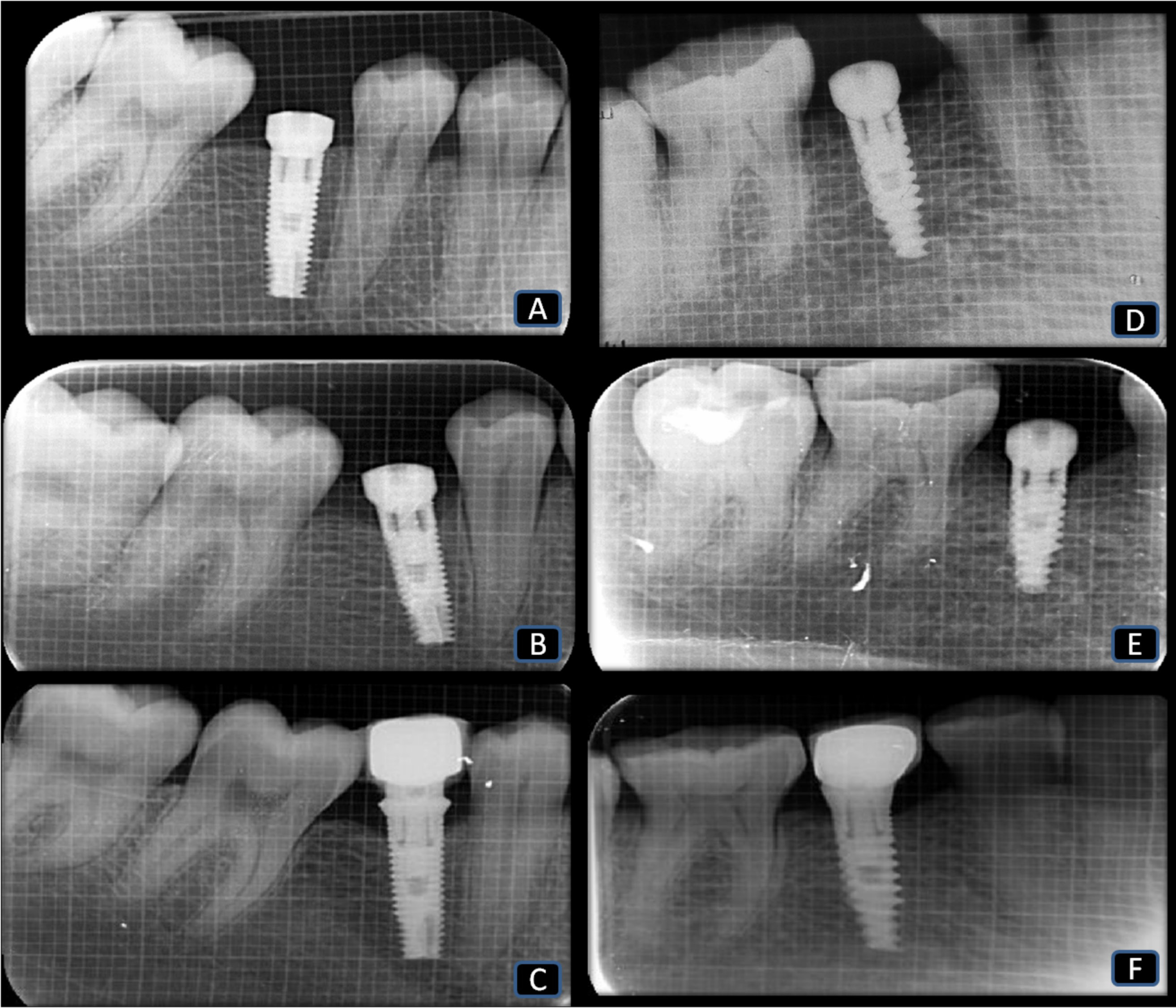
The outcome measures consisted of clinical parameters, including the modified plaque index (mPI),12 the gingival index (GI),13 the width of keratinized tissue (WKT),14 and the thickness of keratinized tissue (TKT).15 Radiographic parameters included CBL, measured using digital intraoral periapical radiography (IOPA).16 An independent examiner (R.D.), who was unaware of the study design, measured all clinical parameters. The WKT was measured using a calibrated manual periodontal probe between the gingival margin and the mucogingival junction (MGJ).14 The TKT was measured after anesthetizing the area using a 15-millimeter endodontic reamer by gently inserting it at the midpoint, 2 mm apical to the gingival margin on the facial aspect (perpendicular to the tooth surface), until the underlying hard structures were contacted, and the distance was measured with a University of North Carolina 15 (UNC 15) periodontal probe.15 Digital IOPA radiographs were taken using a 1 × 1 mm grid to measure CBL from the implant crest to the most apical point of the interproximal crestal bone on both the mesial (M) and distal (D) surfaces; an average value for these measurements was computed: (M + D)/2.16, 17
At their index visit, patients received full-mouth scaling, root planing and oral hygiene instructions, and they were recalled after 2 weeks for implant placement.
Preparation of platelet-rich fibrin
Before the surgical procedure, a 10-cc blood sample was collected from the patient’s antecubital vein, transferred to a test tube without an anticoagulant, and instantly centrifuged at 2,700 rpm for 12 min.18 We removed the fibrin clot that developed in the mid-portion of the tube and compressed it in the PRF box to obtain a PRF membrane.
Surgical procedure
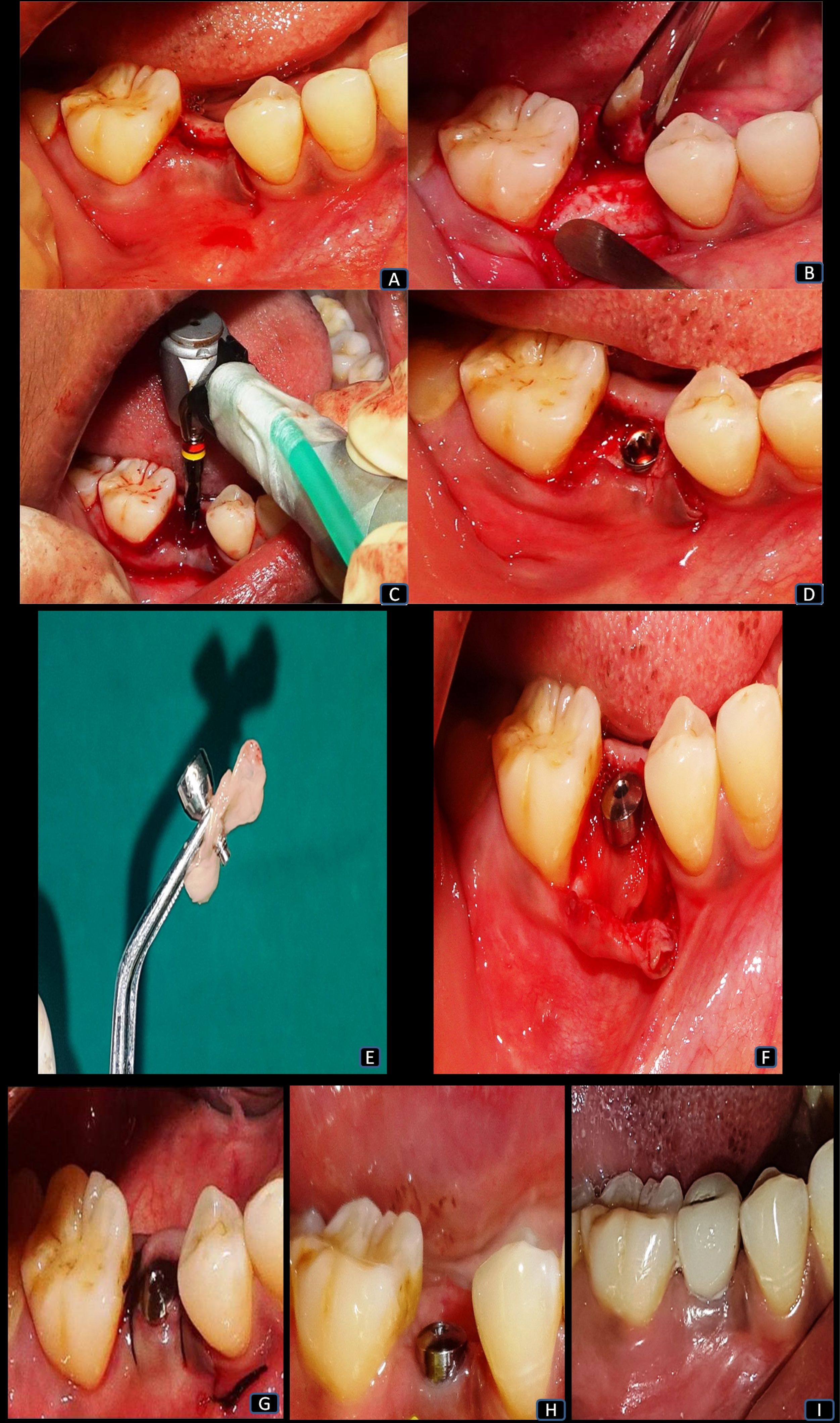
Under adequate local anesthesia, a sulcular mid-crestal incision was made extending to the adjacent tooth (Figure 2), and a full-thickness mucoperiosteal flap was reflected on both the buccal and lingual sides (Figure 2). The initial bone marking used a surgical template. For placing a tapered cylindrical endosseous implant, the osteotomy site was prepared using a series of drills, starting with a 2-millimeter pilot drill, with a speed ranging from 500 to 1,200 rpm under copious irrigation until the desired length was established (Figure 2). Afterward, the implant was installed, and primary stability was assessed using the resonance frequency analysis (RFA) device (Osstell, Gothenburg, Sweden) (Figure 2). Next, we placed the healing abutment on the implant with the use of a torque control device.
In group I, the PRF membrane was placed along with the healing abutment, using the poncho technique to cover the implant (Figure 2).19 The healing abutment was tightened to the PRF membrane so that the PRF membrane covered the implant and the alveolar crestal interface (Figure 2). Subsequently, the flap margins were approximated and sutured in both groups, using non-absorbable 3-0 black silk sutures (Figure 2).
Postoperatively, amoxicillin (500 mg thrice daily) and analgesics (100 mg aceclofenac, 500 mg paracetamol and 15 mg serratiopeptidase twice daily) were prescribed for 5 days, along with 0.2% chlorhexidine gluconate twice daily for 15 days. Postoperative instructions were given to all patients, and they were recalled after 1 week for suture removal. All surgical procedures and postoperative care were carried out by the primary investigator (R.N.S.C.).
At 3 months post-op, the healing cap was replaced with a prosthetic abutment (Figure 2). The restoration was provided with a cement-retained porcelain-fused-to-metal ceramic crown (Figure 2). All outcome measures were evaluated immediately post-op (baseline), and at 3 months and 6 months post-op for both groups. Figure 3 shows the digital IOPA radiographs for both groups.
Statistical analysis
Statistical analysis employed IBM SPSS Statistics for Windows, v. 22.0 (IBM Corp., Armonk, USA), and was performed by an independent statistician who was blinded to the study groups. After calculating the mean (M) and standard deviation (SD) values, the 2 groups were compared with regard to mPI, GI, WKT, TKT, and CBL at baseline, 3 months and 6 months, using the Mann–Whitney U test. Within-group analysis used the Wilcoxon matched-pairs test. A p-value <0.05 indicated statistical significance.
Results
Out of the 40 implants, 3 (1 in group I and 2 in group II) failed to osseointegrate, and 2 patients (1 in each group) did not attend the follow-up examination. Therefore, the analysis was carried out for 35 patients: group I (n = 18; 10 males and 8 females; mean age: 37.11 ±10.43 years); and group II (n = 17; 8 males and 9 females; mean age: 35.88 ±10.76 years) (Table 1, Table 2).
Clinical parameters
The mean mPI and GI scores were statistically similar for both groups at the 3- and 6-month time points, and between 3 months and 6 months (p > 0.05). Within the groups, the mean mPI and GI values did not show any significant differences when compared between 3 months and 6 months (group I: p = 0.081, p = 0.592; group II: p = 0.063, p = 0.463, respectively) (Table 3).
The mean WKT values for groups I and II showed statistically significant changes between baseline and 3 months (p = 0.003 and p = 0.027, respectively), between baseline and 6 months (p = 0.000 and p = 0.001, respectively), and between 3 months and 6 months (p = 0.002 and p = 0.003, respectively). Besides the statistically significant difference from baseline, a gain in WKT was also observed in group I vs. group II at 6 months post-op (p < 0.05) (Table 3).
Statistically significant increases in TKT were achieved for groups I and II between baseline and 3 months (p = 0.001 and p = 0.016, respectively), and between baseline and 6 months (p = 0.000 and p = 0.007, respectively). Meanwhile, a significant difference was observed in group I between 3 months and 6 months (p = 0.018), unlike in group II (p = 0.970). When comparing the mean TKT scores between the 2 groups, significant gains were observed in group I vs. group II at 3 and 6 months post-op (p < 0.05) (Table 3).
Radiographic parameters
The CBL showed a statistically significant increase in both groups independently at 3 and 6 months post-op (p < 0.05), while the difference was not significant for the time interval 3 to 6 months. The mean difference in CBL from 3 to 6 months within group I was 0.43 ±0.53 mm, while it was 0.54 ±0.48 mm for group II. A statistically significant decrease in CBL was observed in group I vs. group II at the 3- and 6-month time points (p < 0.05) (Table 4, Table 5).
Discussion
To the best of our knowledge, none of the available studies on the use of PRF in various surgical procedures have considered its potential significance in early soft tissue healing or evaluated CBL around non-submerged implants. The current comparative study examined the clinical and radiological effects of PRF on the soft and hard tissues surrounding non-submerged implants. We placed 40 implants in posterior mandibular edentulous sites based on the quality and quantity of the available bone, initially evaluated using cone-beam computed tomography (CBCT) for diagnostic purposes.20 Of these implants, 3 failed to osseointegrate, and 2 patients were lost to follow-up. As such, results from 35 non-submerged implants were analyzed, and functional soft tissue integration and patient satisfaction were obtained.
He et al. described advancing age to be associated with decreased bone density, which further affects implant osseointegration.21 Therefore, we included patients aged between 20 and 60 years (mean age: approx. 36 years).
Numerous growth and differentiation factors, such as bone morphogenic proteins and lactoferrin, enhance bone regeneration. Also, vitamin D plays a vital role in osseointegration by maintaining calcium and phosphorus homeostasis during bone metabolism. Optimal levels of 25-hydroxycholecalciferol significantly increase the bone level at the implant site during osseointegration, according to Kwiatek et al.22 Therefore, evaluating vitamin D levels in the current study could have improved the treatment outcomes.
Plaque development around non-submerged implants is an important etiological factor for peri-implant disease and gingival tissue inflammation. The present study found no significant increase in the mPI and GI scores around the implants in either group. These findings can be attributed to the repeated reinforcement of oral hygiene measures given to the patient, as well as the patient’s compliance with maintaining good oral hygiene.23 On comparing the within-group change in scores, group I showed reduced mPI and GI scores, indicating that the PRF membrane, when placed around implants, enhances angiogenesis and maintains tissue integrity.
We observed a considerable rise in the WKT and TKT values in both groups, which may be due to the functional soft tissue integration and adaptation achieved from the immediate placement of the healing abutment, unlike in the case of the two-stage implant procedure, where it is often sacrificed for the reopening surgery to gain access to the implant fixture and place the abutment.24, 25 These findings concur with previous studies by Temmerman et al.26 and Linkevicius et al.,27 who reported better gains in WKT and TKT with the placement of a PRF membrane around the implant. Furthermore, the increases in WKT and TKT may have also contributed to the lower mPI and GI scores, since an adequate zone of keratinized mucosa is crucial for preventing the development of plaque and the subsequent peri-implantitis, and for preserving the health of the surrounding tissues.26, 27, 28
A statistically significant, although minimal, decrease in CBL was observed in group I at 3 and 6 months post-op as compared to group II, which may be explained by the concept of ‘natural bone regeneration’ given by Simonpieri et al.29 They suggested that the bone volume and gingival tissues regenerated through the PRF membrane due to the presence of multiple growth factors in its structure, such as platelet-derived growth factors and transforming growth factors.29 The factors are engaged in the osteoblastic activity and tissue regeneration by stimulating the osteoblastic response, with stable effects that improve bone formation.30, 31
We preferred using digital IOPA radiographs over CBCT following implant insertion due to the possibility of obtaining radiographic image artifacts, especially through metal restorations, like implants.32 It is accepted that employing CBCT after implant placement should be limited to complex surgical procedures for postoperative complications, like iatrogenic neurovascular trauma or implant recovery.33
The current study demonstrated that, when applied locally during a dental replacement procedure, PRF membranes facilitate the healing of the soft tissue surrounding the implant and reduce crestal bone resorption.
Limitations
The study was limited by a small sample size, a short follow-up period, and the evaluation of CBL in only the mesial and distal sides, using two-dimensional (2D) radiographs. Also, the radiographic projections were not standardized, and vitamin D levels were not measured before implant installation. However, there is a need for more meticulously designed longitudinal studies with larger samples that would account for the different biotypes and bone volumes (D1, D2, D3, and D4) to understand the influence of PRF on the adjacent tissues.
Conclusions
Our study shows that the placement of a PRF membrane with a non-submerged implant enhances peri-implant tissue wound healing, with gains in soft tissue width and thickness around the implant.
Future perspectives
The focus of the current study was to evaluate the effects of PRF membranes on the soft and hard tissue parameters around dental implants. However, the number of PRF membranes necessary to obtain soft and hard tissue benefits is yet to be determined. Even though it is possible to use PRF in almost every procedure in implant dentistry, its potential long-term clinical benefits have not been established. Nonetheless, the ease of manipulation, its autologous nature and the release of growth factors support PRF utilization in implant dentistry. Thus, the present study is a stepping stone for future randomized controlled trials.
Ethics approval and consent
to participate
The study was approved by the institutional ethics committee at the Sibar Institute of Dental Sciences, Guntur, India (Ref. No. 111/IEC SIBAR/Lr/17), and it was registered with the Clinical Trials Registry – India (CTRI) (No. 2018/05/013713). All participants provided written informed consent.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.