Abstract
Background. The success of implant therapy depends on the proper evaluation of soft and hard tissues around implants, and the careful selection of biomaterials to manage the associated defects. To attain healthy peri-implant tissues, knowledge about evaluating and managing soft and hard tissues around dental implants is essential.
Objectives. The aim of the present study was to assess the knowledge, awareness and attitudes regarding soft and hard tissue considerations for single implant sites among the registered dental implant practitioners.
Material and methods. The current survey was carried out among dental implant practitioners registered with the Indian Dental Association (IDA). A total of 49 specialists practicing implant dentistry for at least 1 year were included in the study. The survey was conducted using a census approach. A validated questionnaire was circulated digitally among the participants, with 3 rounds of follow-up. To fill in the questionnaire, the participants’ consent was required.
Results. The study involved 14 general practitioners (GPs), 7 periodontists, 10 oral and maxillofacial surgeons (OMFSs), 13 prosthodontists, and 5 certified implantologists. The majority of the participants (93.9%) felt that the soft tissue biotype would influence the treatment outcome (p < 0.05). Most of them (91.8%) evaluated the width of hard tissue at the implant site before surgery (p > 0.05), but only 77.6% of the population evaluated the bone width while considering the future prosthesis (p > 0.05). Although all participants placed implants, only 46.9% performed soft tissue augmentation by themselves (p < 0.001), whereas in the case of hard tissue augmentation, the percentage was 65.3% (p < 0.001).
Conclusions. The study identified various knowledge gaps among different practitioners with different educational background. The educational background seemed to have played a significant role in their attitude toward the evaluation and management of soft and hard tissues around dental implants.
Keywords: CDE programs, dental surgeons, dental association, dental professionals, general practitioners
Introduction
Dental implants have become a predictable alternative for the replacement of missing natural teeth.1 In the early 1980s, implants were mainly placed and managed by oral surgeons and periodontists, but today, implant dentistry is considered an interdisciplinary branch that requires sound knowledge of both surgical and prosthetic aspects.2 However, various organizations and research institutes have introduced certified programs for general practicing dentists willing to start their careers in implant dentistry over some time. With the introduction of such programs, implant placement is practiced by various dental practitioners, including prosthodontists, certified implantologists and general practitioners (GPs).
The success of implants, placed with the use of various protocols, has increased, with predictable techniques and a better understanding of soft and hard tissue biology around implants.3 However, the number of complications has also increased significantly with the increasing number of implants being placed. Therefore, determining implant success has changed significantly from earlier concepts, which focused only on peri-implant tissues,4 to the latest approaches, which include patient-related outcomes, such as esthetics.5, 6 As such, there have been many factors discussed in the literature that can affect peri-implant health and long-term clinical outcomes.7 They include the type of implant–abutment connection,8 the type of retention (cemented or screw-retained),9 soft tissue considerations, such as the tissue biotype, the width of keratinized gingiva (WKG),10 and hard tissue considerations, such as the buccal bone thickness and/or the width of the available bone.11
The majority of those factors are directly related to the proper evaluation of soft and hard tissues around implants, and the careful selection of biomaterials to manage deficiencies. The challenge lies in successfully manipulating soft and hard tissues around the implant for positive long-term results. To achieve optimal clinical and sub-clinical peri-implant health,12, 13 it is indispensable to have knowledge about the evaluation of soft and hard tissues around dental implants. However, studies assessing such knowledge in implant practitioners are scant. Hence, the present study evaluated the knowledge, awareness and opinions of the registered dental practitioners regarding soft and hard tissue considerations around single dental implant sites based on the available evidence.
Material and methods
The present study was a questionnaire-based cross-sectional survey carried out among implant practitioners registered with the Indian Dental Association Dakshina Kannada (IDA-DK). Implant practitioner data was collected from the IDA-DK branch. After obtaining the approval of the institutional ethics committee (Ref. No. ETHICS/ABSMIDS/135/2021), an online questionnaire was sent to the dental practitioners between August and October 2021.
The survey was carried out anonymously, using a census approach, wherein all willing participants were included, and those unwilling were excluded. The selection criterion was dental practitioners with at least 1 year of practice in implant dentistry. Data from a total of 106 practitioners was collected, out of which 58 were identified as implant dentistry practitioners. Seven of the 58 were not interested in participating, 1 acted as an expert for survey validation and 1 was a part of the study (S.B.S.), leaving 49 respondents.
A self-administered questionnaire was sent to the participants digitally, with three rounds of follow-up. The purpose of the study was explained in detail, and confidentiality regarding their participation was assured.
The objective of the study was to:
– assess the knowledge regarding soft and hard tissue evaluation at single implant sites;
– assess the awareness regarding soft and hard tissue augmentation techniques at single implant sites;
– understand the clinicians’ attitudes regarding the selection of soft and hard tissue augmentation techniques at single implant sites.
The questionnaire was written in English for easy perception and response, and contained precise questions on the topic. However, no question on the source of the participants’ knowledge was covered.
The questionnaire was divided into 3 sections: general information; soft tissue considerations; and hard tissue considerations.
Statistical analysis
All data was obtained from Google Forms, entered into a Microsoft Excel file, verified, validated, and then analyzed using IBM SPSS Statistics for Windows, v. 23 (IBM Corp., Armonk, USA). The hypothesis was tested using qualitative variables represented by percentages and with the χ2 test. A p-value <0.05 was considered statistically significant when the data was analyzed at the 95% confidence interval (CI) level.
Results
A total of 49 participants were involved in the study: 14 GPs; 7 periodontists; 10 oral and maxillofacial surgeons (OMFSs); 13 prosthodontists; and 5 certified implantologists (Table 1). The study results indicate that 63.3% of the participants had fewer than 5 years of experience, and 10.2% had more than 15 years of experience in implant dentistry. However, there was no statistical significance between the groups. Most of the study population had a private practice (73.5%), while 22.4% worked in private and public sectors. More than half of the participants (53.1%) had undertaken research or training, while 77.6% had attended continuing professional development (CPD)/continuing dental education (CDE) courses on implants in the last 2 years. None of the certified implantologists had attended any CPD/CDE courses. In addition, 75.5% of the participants deemed implants to be a better treatment option than a fixed partial denture (FPD), and 38.5% of the prosthodontists deemed FPD superior to implants. The quality and quantity of the available bone determined implant selection among 59.2% of the participants, followed by the patient’s economic status or the implant cost (20.4%). Around 67% of the participants favored the switched platform type, while the remaining preferred a platform matched to the type of implant placed. All periodontists and 76.9% of the prosthodontists preferred platform-switched implants, while 57.14% of GPs preferred platform matching (Table 1).
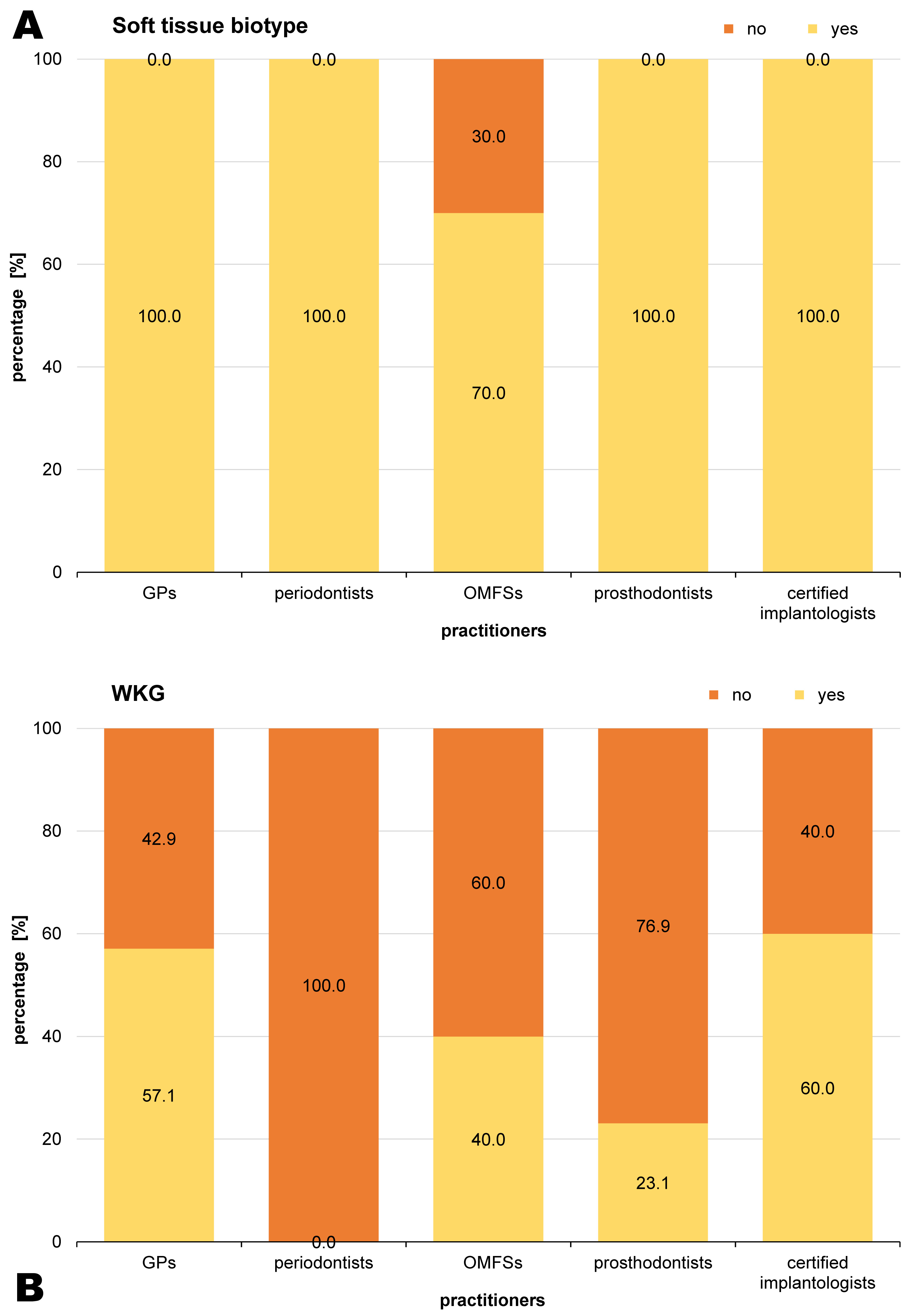
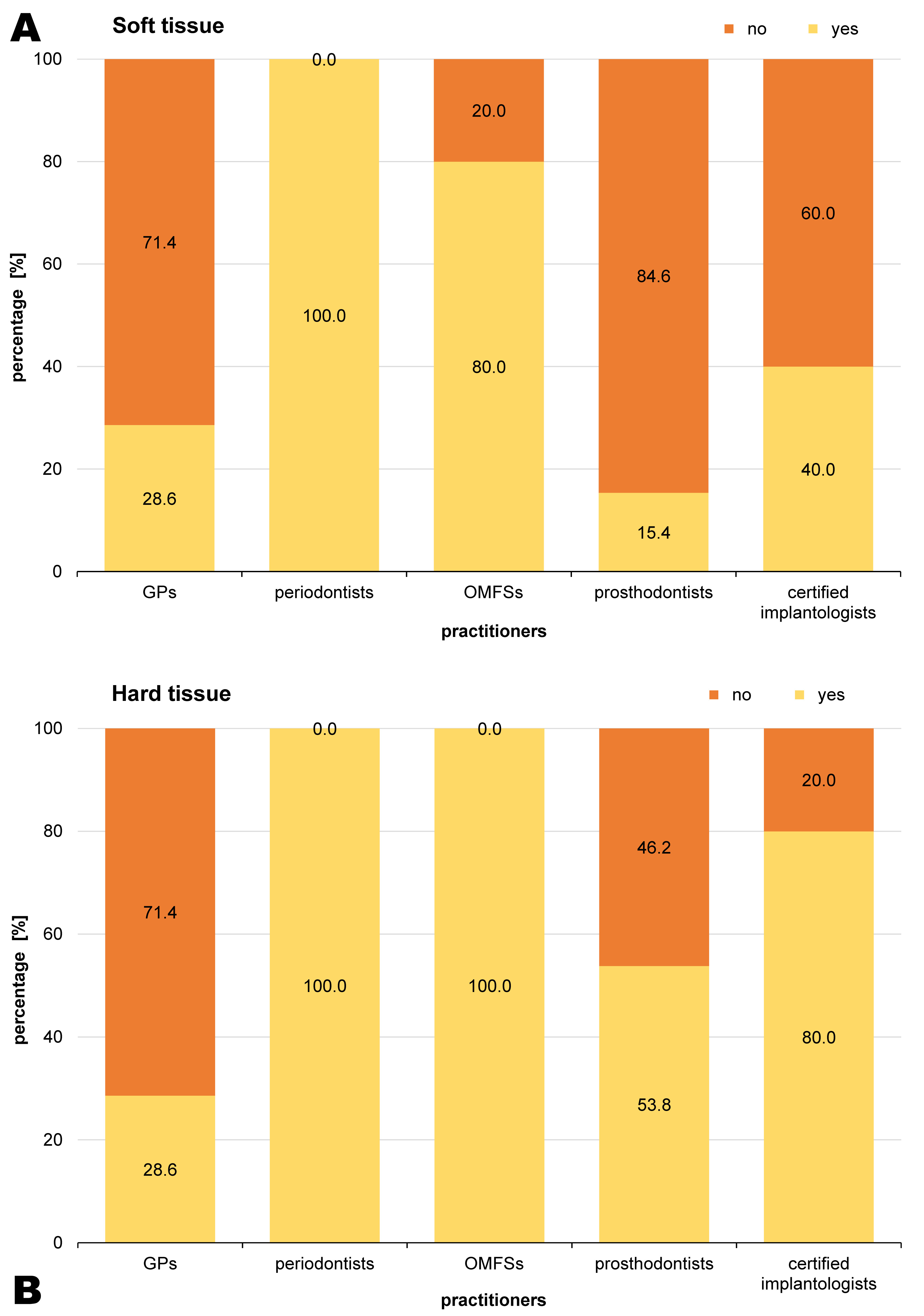
Most of the study population (93.9%) deemed the soft tissue biotype to influence the treatment outcome (p < 0.05), of which only 67.4% considered it in all cases. Meanwhile, 30% of the OMFSs thought that the soft tissue biotype had no influence on the treatment outcome. The majority of the population evaluated the soft tissue biotypes by using probe penetration at the edentulous site (37.0%) or the probe transparency method on the adjacent tooth (34.8%). Most of the participants (67.3%) and all periodontists considered WKG before implant placement. The keratinized gingiva was measured from the mucogingival junction to the gingival margin by 81.8% of the participants, including all OMFSs and prosthodontists. All periodontists and most of the OMFSs (80.0%) performed soft tissue augmentation by themselves, while the majority of the GPs (71.4%) and prosthodontists (84.6%) called for consultants (p < 0.001). All periodontists indicated the sub-epithelial connective tissue graft (SCTG) to be the best material for enhancing the soft tissue biotype. The SCTG was perceived to increase WKG the most among the participants (30.6%), followed by free gingival graft (FGG) (26.5%) (p < 0.05) (Table 2 and Figure 1).
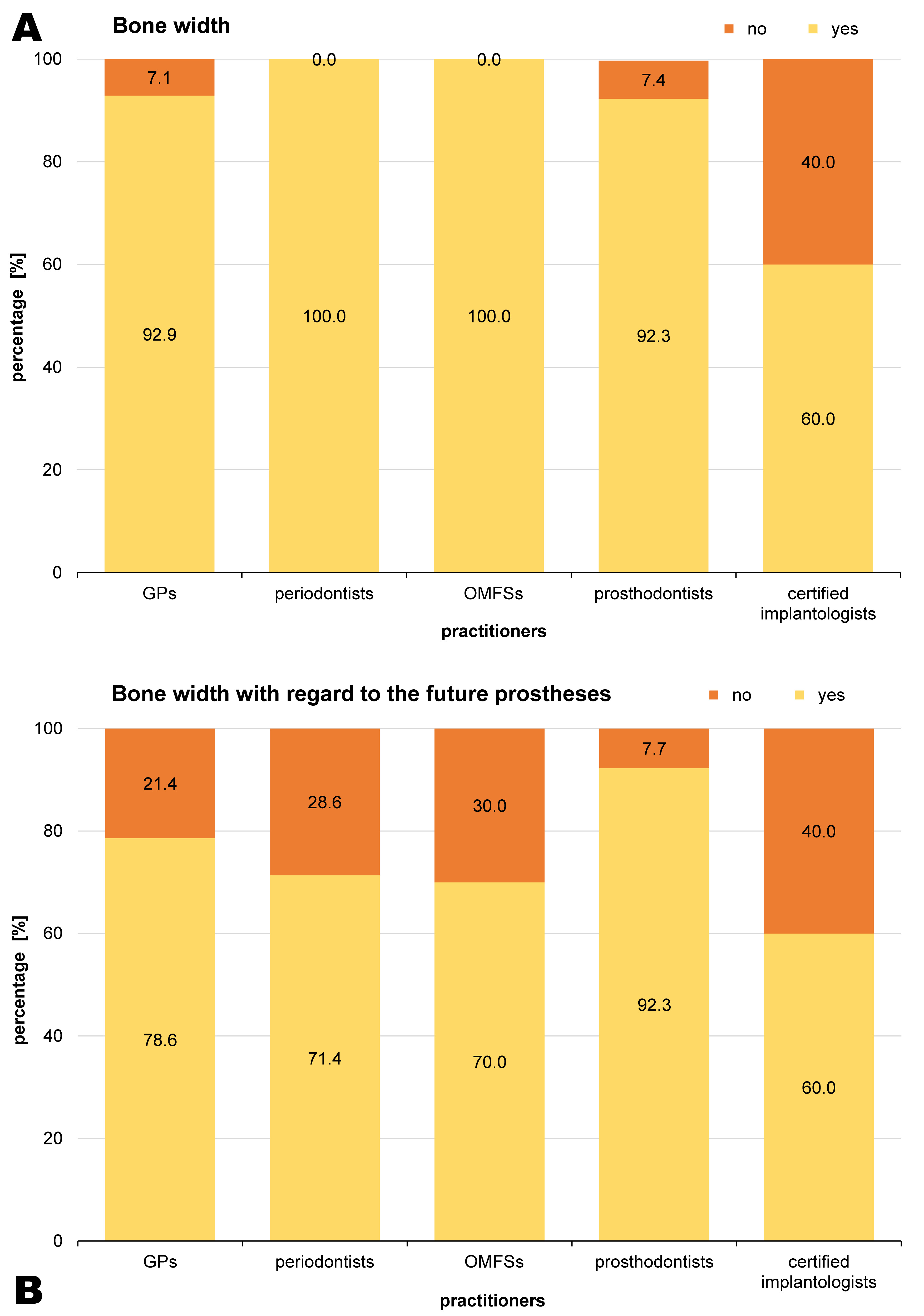
Most participants (91.8%), including all periodontists and OMFSs, evaluated the hard tissue width at the implant site before surgery, while 77.6% of the population evaluated the bone width while considering the future prosthesis, most being prosthodontists. The bone width was evaluated using cone-beam computed tomography (CBCT) by the majority of the participants (66.7%). Similarly, most of the practitioners (81.3%) used CBCT to evaluate the bone length, particularly the OMFSs (90.0%) and all prosthodontists (p < 0.05). The facial bone thickness was evaluated before implant placement by 83.7% of the population. Most of the participants (65.3%) considered contour augmentation during implant placement, while 18.4% performed it in all cases. Almost all participants (91.8%) considered augmenting the bone when the available amount of bone was less than in the case of regular platforms, while the remaining 8.7% chose narrow-platform or short implants in cases of deficiency. The majority of the participants performed hard tissue augmentation by themselves, including all periodontists and OMFSs (p < 0.001). Guided bone regeneration (GBR) was performed by 62.5% of the participants, while only 6.3% were familiar with all types of hard tissue augmentation techniques (Table 3 and Figure 2).
Figure 3 presents the percentages of practitioners performing soft and hard tissue augmentation by themselves.
Discussion
Today, implant-supported prostheses have become a better treatment option for replacing missing natural teeth than FPD.14 The knowledge regarding the anatomy, evaluation and management of soft and hard tissues is a prerequisite before implant placement, as it plays a vital role in the long-term success of implants.15 In the current study, the quality and quantity of the bone at the implant site were a significant consideration for selecting the type of implant. However, the patient’s financial capability was also a determining factor for 20.4% of the study participants.
Implants are classified as bone-level and tissue-level. Bone-level implants, in turn, can be classified into platform-switched (internal hex or conical connections) and platform-matched based on the type of implant–abutment connection.8, 16 A series of studies have demonstrated that platform-switched implants produce better crestal remodeling than platform-matched implants (0.5 mm vs. 2 mm of bone loss around the crest).17, 18, 19 The majority of the study participants (67.3%) used platform-switched implants, while 57.1% of the GPs preferred platform-matched implants. Platform-switched implants have been introduced more recently than platform-matched implants.20 Specialists, such as periodontists and prosthodontists, are well aware of the benefits of platform-switched implants, which was reflected in their selection of the implant system based on the quality and quantity of the available bone. The GPs lacked the knowledge about the latest innovations, as many of them had not attended any CDE programs in the last 2 years. In addition, platform-matched implants are comparatively cheaper than platform-switched implants, which could have influenced their choice in clinical practice (Table 1).
The soft tissue biotype has a vital role in preventing long-term peri-implant complications.10 Most participants (93.9%) deemed the soft tissue biotype to influence the long-term treatment outcome, but only 67.4% considered it in all scenarios. Currently, various methods are available for evaluating the soft tissue biotype, such as probe visibility through the sulcus,21 penetration with an endodontic file, ultrasonography (USG), and CBCT.22 However, penetration with an endodontic file at the site gives a better estimation of the biotype, while probe transparency is also considered to give better results due to its minimal invasiveness.23 Nevertheless, in the current study, most participants used either penetration with a probe at the implant site or the probe transparency method on the adjacent tooth to determine the soft tissue biotype.
The WKG has a critical role in the long-term maintenance of implants, especially if the patient is not compliant with oral hygiene.10 In the current study, 67.3% of the respondents, including all periodontists, considered WKG before implant placement. There are various methods available to measure WKG, including the visual method, the histochemical method and using a probe to measure the keratinized gingiva from the mucogingival junction to the gingival margin,24 with 81.8% of the study participants using the latter. All OMFSs and prosthodontists, and the majority of the periodontists utilized this method for evaluating the keratinized gingiva. However, less than half of the participants (46.9%) performed soft tissue augmentation. Periodontists and most OMFSs performed such procedures by themselves, while most GPs and prosthodontists called for consultants. Generally, tissue with a thick biotype has more connective tissue components than epithelial components as compared to a thinner biotype.25 Hence, connective tissue is the gold standard in terms of biotype-switching.26 Of all study participants, 42.9% preferred connective tissue as a biotype-switching material, while others preferred FGG and soft tissue substitutes. Meanwhile, 30.6% perceived SCTG to be the best material for increasing WKG, and 26.5% perceived FGG to be optimal, including as many as 71.4 of the periodontists. Nevertheless, current evidence suggests that autogenous grafts (SCTG and FGG) increase WKG,26 though they have disadvantages, such as limited availability, postoperative pain and second-site morbidity. Hence, soft tissue substitutes, like xenogenic collagen matrices and acellular dermal matrices, have been used to replace autogenous grafts.27 Also, pre-hydrated membranes that simulate the natural environment perform better than non-hydrated membranes.28 However, the latest evidence indicates similar patient-reported outcomes (the endpoint of soft tissue grafting) with autografts and soft tissue substitutes.29
The bone width and length should be appropriately assessed before implant placement. Adequate bone width should be present to place regular platform implants in the restorative-driven position.11 In the current study, 91.8% of the participants evaluated the bone width before implant placement, but only 77.6% evaluated it while considering the future prostheses, i.e., restoration-driven implant placement, among them 92.3% of the prosthodontists. The bone width and length can be evaluated using many invasive and non-invasive methods. Though direct evaluation following flap opening is the gold standard, it is not feasible to plan surgery in the prosthodontic-driven implant position with the use of this method. Hence, CBCT is a better non-invasive method for estimating the bone width and length. Two out of 3 participants in the study utilized CBCT to evaluate the bone width, while 4 out of 5 used CBCT to evaluate the bone length. One striking finding in this aspect is that all of the prosthodontists employed CBCT, with or without other methods. In cases of inadequate width and length, bone narrow-platform implants or short implants are generally used to compensate. However, narrow-platform implants underperform as compared to regular-platform implants due to the reduced bone-to-implant contact surface,30 and the evidence regarding short implants is still debatable.31
Another critical aspect for the long-term success of implants is the thickness of the buccal bone, with data showing that a minimum of 1.5–2 mm is required.11 The buccal bone thickness of the anterior maxilla is usually less than 2 mm.32, 33, 34 Hence, contour augmentation is generally indicated in most cases with the buccal bone thickness of less than 1.5 mm.35 The facial bone thickness was evaluated by 83.7% of the study population, while contour augmentation with simultaneous implant placement was considered by 65.3% of the participants, but only 18.4% of the practitioners performed it in all cases. All periodontists and OMFSs performed hard tissue augmentation, which is likely due to the surgical training they seek during their postgraduate residency. Meanwhile, 62.5% of the study participants were familiar with GBR. The current study results suggest that implant practitioners give more attention to hard tissue than soft tissue. However, soft tissue has a decisive role in long-term maintenance. Since all study participants place implants, but not all perform augmentation, it is essential for everyone to have sound knowledge about the influence of soft tissue on diagnosis and management.
Our findings could be used to identify knowledge gaps in dental practitioners with different educational backgrounds. Most of the study participants had good knowledge regarding soft and hard tissues around implants. However, they lack awareness and opinions with regard to the abovementioned treatment, except for periodontists and oral surgeons. Specialist-specific CDE or CME programs should be conducted more often, and frequent reviews of knowledge and awareness should be performed. Implant dentistry is an interdisciplinary and rapidly developing science: it is the duty of every dental practitioner placing implants to learn about the latest advances and evidence, and learning should be considered a continuous process.
Limitations
As far as the authors are aware, this is the first study to assess implant practitioners’ knowledge, awareness and opinions regarding soft and hard tissue considerations at a single implant site. However, the study has inherent limitations, such as a small sample size in a localized area, comparatively inexperienced practitioners, and questions limited to the clinical aspects of soft and hard tissue considerations at the implant site. Future studies in different regions, with a broader range of questions would help to understand the discrepancies between the evidence provided in the literature and applications in clinical practice.
Conclusions
The current study identified various knowledge gaps related to the different backgrounds of implant practitioners. Our findings suggest that education and knowledge play a key role in determining the attitude toward treatment planning and the subsequent material selection. Comprehensive knowledge of soft and hard tissues is essential, as all study participants practice implant dentistry.
Ethics approval and consent to participate
The research was approved by the institutional ethics committee at the Indian Dental Association Dakshina Kannada (IDA-DK) (Ref. No. ETHICS/ABSMIDS/135/2021). All participants provided written informed consent.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.