Abstract
Background. A retromolar canal (RMC) is an anatomical variation of the mandibular canal located in the retromandibular area. Retromolar canals and their contents may be of great clinical importance for clinicians dealing with the discussed region. The analysis of the available literature indicates that RMC is not a rare phenomenon.
Objectives. The purpose of the present study was to present the prevalence of RMC and its dependence on patient gender, as well as the location of RMC (unilateral or bilateral), by using cone-beam computed tomography (CBCT).
Material and methods. Two hundred CBCT examinations taken from the database of the Department of Dental and Maxillofacial Radiodiagnostics of the Medical University of Lublin, Poland, were analyzed by 2 independent observers (a fifth-year dentistry student and a dentist with 9 years of experience in the field of dental and maxillofacial radiodiagnostics). The research sample included 134 women and 66 men.
Results. After comparing the results obtained by the 2 independent observers, the more experienced researcher excluded 9 cases from the study; RMC was ultimately found in 21/200 subjects (10.5%). The unilateral variant was observed in all 21 cases – 13/21 (61.9%) on the right side and 8/21 (38.1%) on the left side. Seven (5.2%) RMCs were found among the 134 women, while among the 66 men there were14 (21.2%) RMCs found.
Conclusions. On the basis of the conducted research, RMCs were found in 10.5% of cases. They were more common in men than in women. Cone-beam computed tomography is an examination that allows the determination of the position and course of RMC more precisely than panoramic X-rays.
Keywords: mandible, anatomy, CBCT, retromolar canal
Introduction
A retromolar canal (RMC) and a retromolar foramen (RMF) are variations in the anatomical structure of the mandible. The canal is relatively short, deviates from the mandibular canal at different heights, and ends at the upper surface of the alveolar part of the mandible in the retromolar area as RMF.1 The contents of the canal can consist of nerve fibers from the inferior alveolar nerve, as well as blood vessels.2 According to Bilecenoglu et al., an artery of a 120–130 mm lumen is present in RMC.3 After exiting the aperture, nerve fibers branch out. They can innervate the temporalis tendon, the buccinator muscle, the mandibular third molar, the gingiva in the area of mandibular premolars and molars, and the mucosa of the retromolar area.4 The presence of RMC can be associated with complications during surgical procedures. It may also be a pathway for tumors or the spread of infections.5 There are many different classifications that describe the anatomy of the canal. In 2011, Von Arx et al. proposed a classification, differentiating 3 types of canals.6 In 2013, Patil et al. subdivided one of the types proposed by Von Arx et al. into 2 variants.7
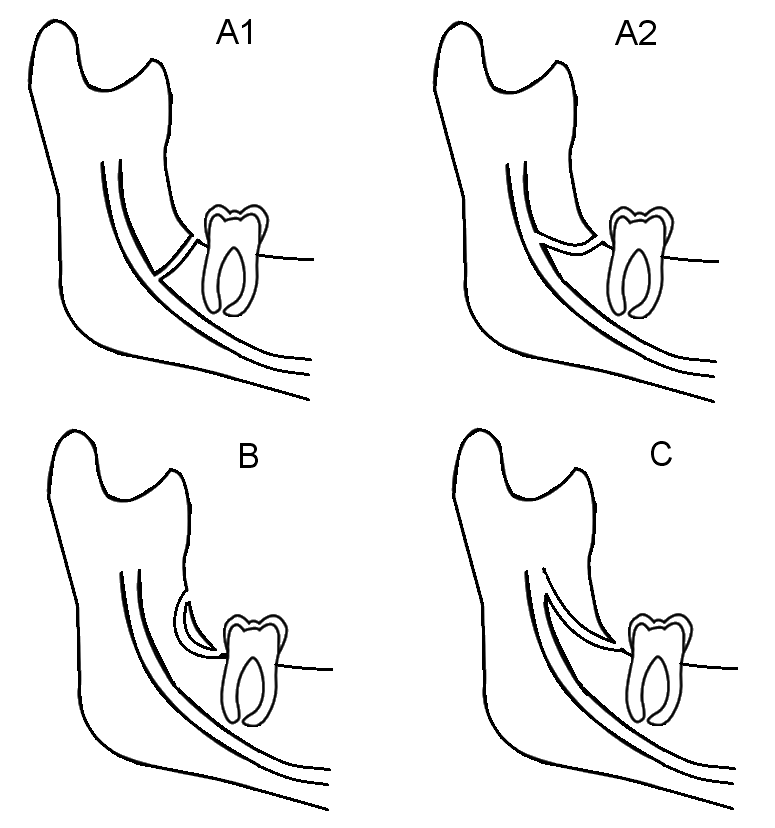
The selected classification, according to Patil et al.,7 describes 4 types of RMC alignment (self-drawn) (Figure 1):
– type A – the canal branches vertically from the mandibular canal, distally from the third molar, it runs backward and upward, and then opens within the retromolar area:
- • type A1 – the canal runs backward and upward to open into the retromolar area,
- • type A2 – the canal runs a certain distance forward, and then reverses backward and upward to open into the retromolar area;
– type B – the canal branches below the mandibular foramen, and then runs forward and upward to open into the retromolar area; and
– type C – the canal separates near the mandibular foramen, and then runs horizontally forward to open within the retromolar area.
This research was based on evaluating cone-beam computed tomography (CBCT) images. It is a relatively new but already widespread modality in dental diagnostic imaging. Most CBCT units are similar in shape to panoramic models. Some manufacturers offer units that provide both types of imaging – panoramic and CBCT. During the examination, an X-ray tube emits a cone-shaped beam during the rotation of a C-shaped arm around the patient’s head. The data on X-ray attenuation is recorded within a cylindrical volume. In the next stage, a primary reconstruction is prepared by computer software, and eventually, multiplanar reconstructions are created. Depending on the indications, the field of view (FOV) may vary from small through medium to large.
In addition to RMCs, there are other possible variations of anatomical anomalies, such as coronoid process hypertrophy (CPH), which is also defined as giant coronoid syndrome. Coronoid process hypertrophy consists of an abnormal increase in the volume of the mandibular process. One symptom of CPH that almost always occurs is decreased mouth opening (<20 mm). The etiology of CPH is still not conclusive. The treatment consists of intraoral coronoidectomy along with postoperative physiotherapy at the end of growth to obtain the correct range of jaw opening and to maintain it in the long term.8 Another example of an anatomical abnormality is the orofaciodigital (OFD) syndrome. The disease manifests itself in a group of disorders, including the malformations of the mouth, face, hands, and feet. The OFD syndrome is inherited. For dentists, the most important symptoms are changes in the oral cavity. The teeth are often affected by caries, there are teeth with abnormal structures, there is enamel hypoplasia, supernumerary teeth can appear, and tooth agenesis can be observed.9 A patient with a complex image must be treated in a multidisciplinary manner and requires prosthetic rehabilitation, in particular, in order to supplement the missing teeth in the arch.10
The aim of the present study was to determine the prevalence of RMC and its dependence on patient gender, as well as the location of RMC (unilateral or bilateral), by using CBCT.
Material and methods
Two hundred consecutive CBCT examinations retrieved from the database of the Department of Dental and Maxillofacial Radiodiagnostics of the Medical University of Lublin, Poland, were analyzed by 2 independent observers (a fifth-year dentistry student and a dentist with 9 years of experience working in the Department of Dental and Maxillofacial Radiodiagnostics). The examinations were taken with a VistaVox S CBCT (Dürr Dental, Bietigheim-Bissingen, Germany). The inclusion criteria were patients ≥18 years old and good-quality X-ray examinations in the retromolar area (i.e., without distortion and any artifacts caused by metal restorations). The exclusion criteria comprised bone with any pathologies, such as cysts, tumors, inflammation, etc. The research group included 134 women and 66 men aged 18–55 years, with an average age of 30.82 years. The CBCT scans were analyzed in multiplanar reconstructions (coronal, axial and sagittal), using modern ergonomic image processing software VistaSoft (Dürr Dental) and the Coronis Fusion 4MP radiological diagnostic display system (MDCC-4430; Barco, Kortrijk, Belgium). Additionally, on the basis of the tangential view, the type of RMC was determined according to the classification of Patil et al.7
Results
Initially, 30 RMCs were found in the 200 scans. After comparing the results of the 2 independent observers, the more experienced researcher excluded 9 cases from the study, so RMCs were ultimately found in 21/200 subjects (10.5%). In all 21 cases, the canals were unilateral; in 13/21 (61.9%) patients, the RMC was on the right side, and in 8/21 (38.1%) on the left side. Among the 134 women, an additional canal was found in 7 cases (5.2%), while among the 66 men, an additional canal was found in 14 (21.2%) cases.
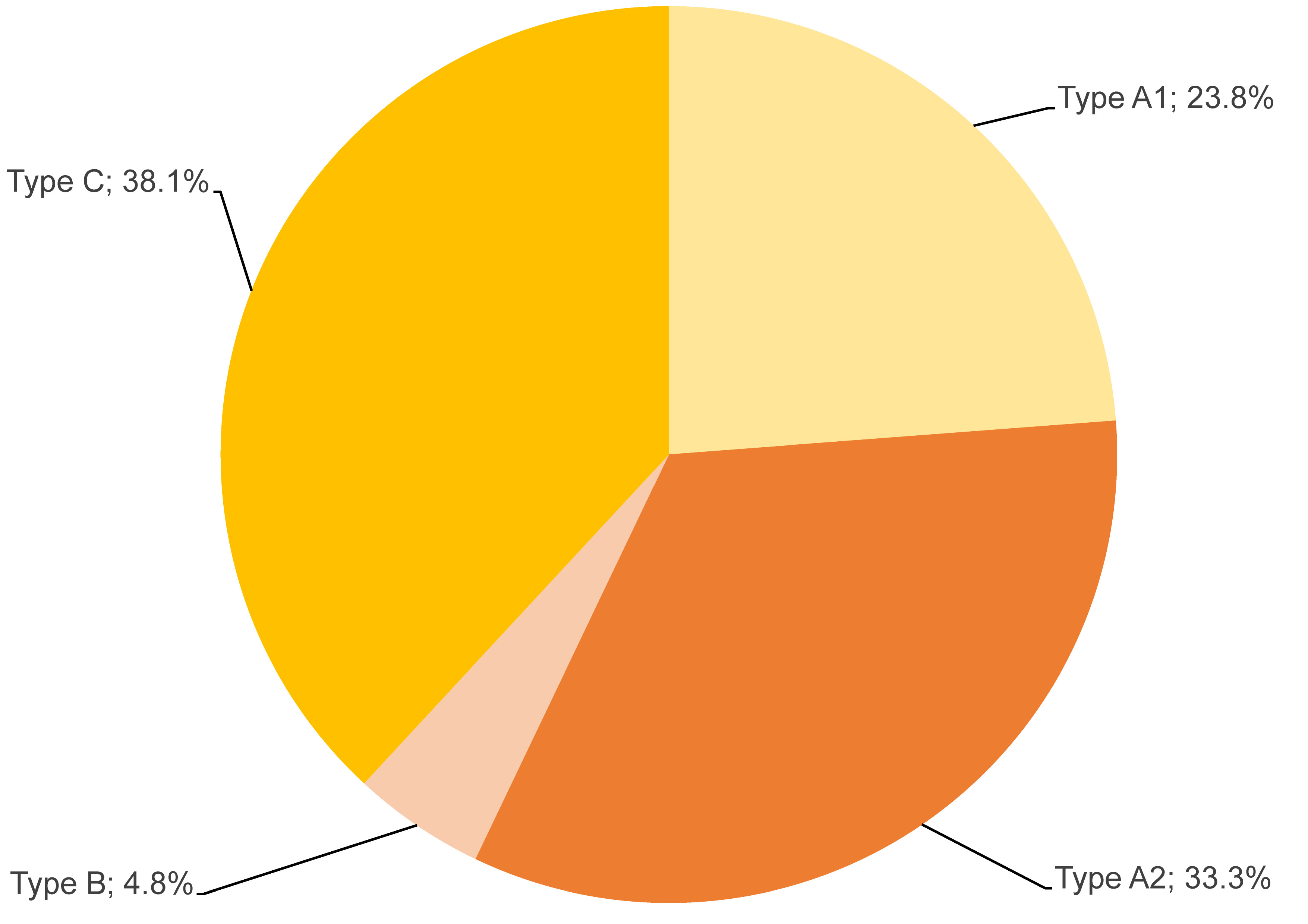
The results showing the prevalence of the types of RMC according to Patil et al.’s classification7 are presented in Table 1 and Figure 2. The examples of each type are presented in Figure 3.
Discussion
Numerous studies have used CBCT examinations to determine the prevalence of RMC,1, 2, 4, 5, 6, 11, 12 but none of them were focused on a Polish population. This research was based on CBCT examinations and revealed the presence of RMC in 10.5% of cases. In other studies, the prevalence of RMC ranges from 5.4% to 75.4%.4 Such a discrepancy can be attributed to several factors, including ethnic differences, environmental factors and genetic diversity, as well as the sample size of the study.
Ahmed et at. showed in their study that the incidence of RMC in CBCT images was 12%, with more identified on the left side (5%) than on the right side (7%).13 Hou et al.5 confirmed the presence of RMC in 25.9% of 657 patients.5 Depending on gender, RMC was observed in 11.6% of men and 14.3% of women. Unilateral RMCs were identified in 20.4% of patients, while 5.5% of the RMCs were bilateral.5 Von Arx et al. estimated the prevalence of RMC at 25.6%.6 According to Hou et al., the canal was found in the range of 8.5–52% in a Chinese population.5 In a Korean population, RMCs were observed in 8.5% of patients (38/446).14
In our study, the canal was always located unilaterally (61.9% on the right side and 38.1% on the left side), which is consistent with other studies that focused on the location of RMC.4, 5, 6, 15, 16
Taking gender into account, our results showed that RMC was more common in men. Out of the 66 examined men, 14 (21.2%) had RMC, while out of the 134 examined women, RMC was noted in 7 (5.2%) cases. A study conducted by Jamalpour et al. did not present a large difference in the occurrence of the canal depending on gender; they showed that RMCs were present in 10.3% of women and 16.7% of men.17 Narayana et al. studied 242 dry adult mandibles in an Indian population.18 Regarding gender, men tended to have RMC more often than women, but no statistically significant difference was found in this respect.18
Considering the types of RMC according to the classification of Patil et al.,7 the most common type of RMC found in our research was type A (57.1%), of which 23.8% were A1 and 33.3% were A2, followed by type C (38.1%), and then type B (4.8%).
A significant problem raised in the literature about the classification of the canal. Some authors believe that it is one of the variants of double or triple canals that depart from the main canal and end in the molar area, while other authors believe that it constitutes a separate structure.1
Cone-beam computed tomography, computed tomography (CT) and panoramic radiographs are used to detect RMFs and RMCs.4
In a study by Kim et al., only 25% of panoramic radiographs showed mandibular canals.2 Although panoramic radiograph images are frequently used for the preliminary planning of treatment, in some cases, it is recommended to extend the diagnostics by taking volumetric tomography. Cone-beam computed tomography more often visualizes the canal and makes it possible to trace its course, which is of great importance in clinical situations. The disadvantage of CBCT is related to the presence of artifacts, defined as discrepancies between the reconstructed visual image and the actual subject, which degrades the quality of these images.4 It also emits ionizing radiation and has limited contrast resolution.19 It is also possible to visualize RMCs on CT, but its use in dentistry is limited due to cost, availability, and the risk related to a higher radiation dose as compared to CBCT and X-rays.12 Furthermore, CT artifacts can include noise, motion, beam hardening, scatter, and metal artifacts. Cone-beam computed tomography is the preferred method due to its lower radiation dose, lower costs and a better detection of anatomical structures.4 It is safe and painless for patients of all ages. It is also better for analyzing the position and orientation of the surrounding structures.19
The ability to detect RMCs with panoramic radiography is limited. Cone-beam computed tomography can be useful in confirming the anatomical variations of the mandibular canal which cannot be visualized with panoramic radiographs. Panoramic radiography is less sensitive, lacks detail, and is characterized by irregular magnification, geometric distortion and the overlapping of anatomical structures. Another disadvantage includes ghost shadows, which are produced by the contralateral side of the mandible, the pharyngeal airway, the soft palate, and the uvula.4
In a study by Von Arx et al., out of the 31 canals observed with CBCT, only 7 were visible in the corresponding panoramic radiographs.6 In a case report, Kaufmann et al. presented a bilateral RMC that was observed on CT, but was not visible with panoramic radiography.20
Based on the literature, it can be concluded that the clarity of CBCT images is affected by artifacts, noise and poor soft tissue contrast.21 Magnetic resonance imaging (MRI) is the most appropriate modality for soft tissue diagnostics. In dentistry, MRI is particularly useful for diagnosing diseases of the temporomandibular joint (TMJ). Magnetic resonance imaging is the gold standard for diagnosis and treatment planning in the disorders of articular disk.22, 23 With the use of MRI, examinations are performed with closed and opened mouth, and mostly static images are taken with an uncomfortable and expensive instrument. Ultrasound (US) examinations overcome these limitations.24 This non-ionizing imaging method is less expensive, more comfortable for the patient, and can easily be used in a dental setting.23
Radiographic examinations are essential in diagnosis and treatment planning in dentistry, but panoramic radiography is less reliable than 3D images, and is not recommended for measurements due to the lack of repeatability.21, 25, 26, 27 Cone-beam computed tomography has a wide range of applications for evaluating dental fractures and cracks, measuring the size of periapical lesions, assessing bone density in lesion areas, conducting endodontic surgery, planning implants, and analyzing TMJs and resorption.28
High-resolution CBCT has become notably effective for confirming anatomical variations in the mandibular canal. It also makes it possible to precisely locate and view the mental foramen.29, 30
The occurrence of RMC affects treatment. Knowledge about its prevalence, topography and structure facilitates treatment, especially during all the procedures requiring the use of anesthesia. It is important to provide treatment in the retromolar area with caution to avoid the complications resulting from damage to its contents.1 Complications may arise from insufficient anesthesia, excessive bleeding, hematomas, and damage to the branches of the inferior alveolar nerve, which may lead to dysfunction of the innervated muscles.4, 11 Blood vessel injuries in the retromolar region during surgery may lead to excessive bleeding in the presence of RMC.31 Khoury and Hanser observed that 1.44% of their patients had heavy bleeding at the donor site.32 This bleeding can be locally managed by crushing the bone in the area occupied by the canal or filling the opening with bone wax or bone chips.32 During the elevation of the mucoperiosteal flap, damage may occur to the neurovascular contents of RMC. This leads to paresthesia of the areas supplied by the retromolar nerve.4 Prosthetic restorations (dentures or dental implants) placed distally to the retromolar area may impinge on the contents of RMC. This may cause discomfort and pain or paresthesia, and is especially significant in the elderly due to the alveolar bone resorption.12 Surgical procedures involving the retromolar region, such as dental implant surgery, impacted third molar extraction and sagittal split ramus osteotomy, can be more complicated.3 The most common complication after the removal of third molars is inflammation, especially during surgical extraction with root separation.33 There are reports suggesting that such surgery should be performed using a triangular flap, which reduces the risk of postoperative complications. It is also vital to focus on the bone structure of the mandibular alveolar process, especially in the retromolar area. Retromolar bone dissection should be limited, and bone removal at the base of the coronoid process of the mandible should be avoided.1
Due to the presence of the canal, anesthetizing the inferior alveolar nerve may result in insufficient anesthesia.11 This is called the ‘escape pain phenomenon’. This escape pain is due to the nerve contents of RMC.12 The Gow–Gates technique or the Akinosi method can be used to anesthetize the inferior alveolar nerve when RMC is present.4, 34, 35, 36, 37 However, these methods of anesthesia should only be used when traditional local anesthesia has failed.12
Conclusions
The present study showed that RMCs were not an infrequent structure. The prevalence of RMCs was 10.5% in the current research group. The most common RMC type in this Polish population was type A. In addition, there was a gender predilection in the studied group, as RMCs were more common in men (F:M = 5.2%:21.2%).
Ethics approval and consent to participate
Not applicable.
Data availability
All data generated and/or analyzed during this study is included in this published article.
Consent for publication
Not applicable.