Abstract
The ball attachments and their O-rings used for the retention and stabilization of overdentures showed a decrease in retention as the number of cycles increased. This fact resulted in a decrease in the retention of the prosthesis. The purpose of this study was to evaluate the fatigue resistance of ball attachments through a systematic review. An electronic search was performed using the Cochrane Library, LILACS, PubMed, ScienceDirect, and Web of Science databases. The search was conducted based on the PICOS framework. The inclusion criteria involved in the search comprised research articles written in English and published between the years 2000 and 2020. In the final selection, 18 articles were included in the review. Most of these studies performed the fatigue retention tests using parallel implants without angles. However, some studies used different angles to analyze the fatigue retention values. With the passage of time, the wear results in deformation and, as a consequence, a decrease in the retention of most attachments, leading to treatment failure. The main factor to be considered is the loss of retention of these components and their low durability. The loss of retention is due to large extent to the materials used to manufacture the attachments and O-rings, the size and angulation of the implants, and the length of the prosthesis. Future research is needed to further elucidate the reasons for the failure of the attachments.
Keywords: fatigue, dental implants, overdenture, dental abutment
Introduction
Dental implants are used to rehabilitate patients who have suffered from the loss of dental elements.1, 2 However, due to the chronic and continuous resorption process of the residual alveolar ridge, the installation of dental implants is limited due to reduced bone thickness or height and the need to perform bone grafts, increasing the number of surgical steps and making the treatment more expensive and difficult for patients to access, either because of purchasing power or medical problems.3, 4 Also, factors such as bone density, age, smoking habit, and systemic osteometabolic diseases can negatively affect the primary stability of the implant and lead to early loss or even contraindicate its installation.2, 5, 6
Primary stability is important to perform the immediate installation of the prosthesis, reduce the number of surgical steps and trauma, as well as to improve the aesthetic and psychology of patients.2, 7, 8, 9 To achieve good primary stability and a good prognosis, different factors must be taken into account.2, 10, 11 In 2021, Tardelli et al. evaluated the micro and microstructure of different implants and demonstrated that different geometries produce different results in primary stability and stress distribution.11 While in 2020, Antonelli et al. evaluated the influence of different surgical protocols on the achievement of primary stability in cancellous bone.2 Thus, taking these factors into account can improve the prognosis of the treatment using dental implants by reducing the probability of implant loss and, consequently, revision surgery with prostheses to support the dental implants.
Different modalities of rehabilitation for edentulous patients are described, among them, overdentures and fixed prostheses stand out.12, 13, 14, 15, 16 The overdentures are removable dentures that can be supported over teeth or dental implants and have good long-term success rates in rehabilitating patients suffering from total edentulism, especially of the mandible,17, 18, 19, 20 where the problems of stability and retention of prostheses cause a reduction in the quality of life and satisfaction of these patients.21, 22, 23, 24, 25 Compared to fixed complete dentures, overdentures are a better option due to their lower cost, relative simplicity, and providing the opportunity to remove the prosthetic device for cleaning by a third party, especially for patients with motor or cognitive problems.15, 26 In line with these advantages, overdentures are indicated for patients diagnosed with orofacial digital syndrome (OFD), such as Papillon–Leage–Psaume, as they have cleft palates in up to 50% of individuals affected by the disease and the most common dental anomaly is the absence of teeth.27, 28
Thus, using overdentures as a form of rehabilitation in patients can lead to a significant improvement in their quality of life from a psychological point of view due to the presence of teeth in patients with agenesis and improved aesthetics in patients with malformations or the absence of teeth. From a nutritional point of view, overdentures can improve masticatory functions leading to the ability to eat harder foods such as vegetables. In regards to oral health, overdentures provide temporary closure of cracks during feeding by the prosthesis, as well as the ability to remove the appliance to perform oral cavity and appliance hygiene to maintain adequate oral health.29, 30, 31, 32
Overdentures can be supported by implants or the remaining natural teeth. The advantages of preserving and using the remaining teeth include a reduced need for surgeries to install implants, bone grafts due to bone scarcity makes the treatment less costly, in addition to preservation of alveolar bone, the periodontal ligament, proprioception, and good masticatory efficiency.33, 34, 35, 36 However, several factors such as age, bone and mucosal tissue, hygiene, number, and position of remaining teeth must be taken into account when choosing whether the treatment will be performed on the remaining teeth or implants and the retention system.27 The most important thing to consider is the personalization of the treatment to benefit and prolong the rehabilitation of individual patients as much as possible.
Currently, various types of attachments are used in retention systems.37, 38, 39, 40, 41 The splinting system, for example, uses a bar and clip-type as the group without splinting uses magnetic attachments, a locator, a double crown, and a ball,42 which is most commonly used.21
The advantages of using a ball attachment include ease of hygiene, requires less space than the bar system, lower cost, and simpler technique for installation and use.43, 44 The functional movements of the insert and removal of the prosthesis, in addition to the parafunctional habits, microbiota, and oral cavity, make up the main disadvantages of this system, resulting in loss of retention over time and the need for frequent replacement and maintenance,24, 45, 46, 47, 48 mainly in implants that are not parallel.44
However, the anatomical limitations, bone quality of the patient, and the technical experience of the dentist can reduce the parallelism of the implants. Implants in unfavorable positions generate lateral forces that, in excess, can cause early failure of the implants, sharp wear, and fracture of prosthetic components.43, 44
Other factors can lead to wear and deformation of attachments, such as overdenture instability, diet, muscle strength, and high concentrations of stress at the ball attachment as a result of stress that comes from functional or parafunctional habits. This load can increase the wear speed of the O-rings and, consequently, retention loss.49 In addition, it is noteworthy that patients with parafunctional habits may present with temporomandibular disorders (TMD) involving the stomatognathic system, especially the masticatory muscles and the temporomandibular joint (TMJ), which can generate pain, restriction of movement, and consequent decrease in the quality of life of these patients.50, 51, 52, 53 Joint inflammation of the synovial membrane is responsible for the pain, which is caused by excessive use of force within the TMJ. This can cause stretching and twisting of the joint capsule, surrounding disc tissue, and ligament, as well as osteoarthritis.53
In addition, loss of ball attachment retention can occur due to differences in the surface and strength of the different materials used, such as metal, nylon, and plastic. The different properties of these surfaces promote quicker wear of the components as well as a reduction in their resistance.18, 54 Deformation, wear, and degradation increase the internal diameter of the O-rings leading to a loss in retention. This is mainly due to a lack of contact between the parts, which reduces the coefficient of friction, and consequently, the O-ring slides and comes off with a lower holding force.46, 55
The study of a material’s properties is fundamental to understanding how wear occurs and causes a loss or increase in fatigue resistance and retention of the ball attachments and their O-rings. The literature also contains gaps in the study of the physical, chemical, and biological properties of these materials. Most studies cite the loss of retention as a consequence of deformation. However, few studies specifically mention how the process develops and how to avoid it, this gap in knowledge fails to provide a clinically meaningful analysis of dental materials. Through clarification of these answers, we hope to find a solution to the main problem experienced when using this type of attachment, which is the loss of retention.
Thus, studies on the fatigue of ball attachments and their O-rings are necessary for the researcher and clinician to be able to rely on results based on scientific evidence when selecting the correct attachment. In addition, understanding a material’s main disadvantages, seeking to reduce them, and exploring alternatives and solutions benefit patient care which highlights the importance of this research.
This study aimed to evaluate the fatigue resistance of ball attachments and their components, such as O-rings and capsules, through a systematic review. Also, we tried to answer the question: “What are the reasons fatigue of the ball attachments occurs?” To help researchers and dentists select or make the ideal prosthetic component based on physical, chemical, mechanical, and biological properties to enhance durability and prolong the treatment time of patients with supported overdenture implants.
Methods
Protocol and registration
This research was conducted and structured in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses protocol (PRISMA),56 and was registered in the Open Science Framework (osf.io/6839h).
Eligibility criteria
The criteria for this review were made using the PICOS framework: Population – ball attachments and their components; Intervention – fatigue of the attachment; Comparison – different models of ball attachments and their components untested and tested; Outcomes – reasons leading to fatigue; and Study design: in vitro studies. The question answered with this research is: “What are the reasons fatigue of the ball attachments occurs?”
As inclusion criteria, only articles that contemplated ball attachments and methods that used O-rings or their respective capsules were selected. It included tests on fatigue, published in English from 2000 to 2020, and only research articles were considered. The exclusion criteria were articles that did not include ball attachments, especially in relation to their prosthetic components, such as O-rings and capsules, and that did not include fatigue retention tests.
Information and search strategy
An electronic search was performed using the Cochrane Library, LILACS, PubMed, ScienceDirect, and Web of Science databases with the terms “overdenture” AND “ring” AND “fatigue”, “overdenture” AND “attachments” AND “fatigue”, “overdenture” AND “retention system” AND “fatigue”, and “overdenture” AND “abutments” AND “fatigue” to find articles whose main theme was evaluating causes of fatigue for ball attachments used in overdentures.
The searches included in this study were carried out manually by the researchers. A reference management program (Mendeley Desktop, London, UK) was used to remove duplicate references to facilitate the reading and final selection of articles.
Study selection
This research was conducted in two principal phases. In the first step, two reviewers independently, (M.R.C) and (A.L.B), screened the titles and abstracts to identify eligible studies. The second step after the eligibility studies was identified required all collaborators to read the full texts that met the inclusion criteria. With the potential studies identified, the two reviewers discussed with the coordinator (A.C.R) to decide if the studies were to be included in this review.
Data collection process
The data extracted from the papers are in Table 1, which includes the authors, year of publication, aim, number of samples, number of cycles, and the results of the fatigue tests.
Assessment of the risk of bias
The risk of bias was classified as low risk when the article was very clear and anything could alter the results, unclear when we needed to justify if this was valid for the article, or high risk when there was a serious risk of altered results. The articles were classified according to the methodological quality of included studies by the Joanna Briggs Institute.57
Results
Study selection and characteristics
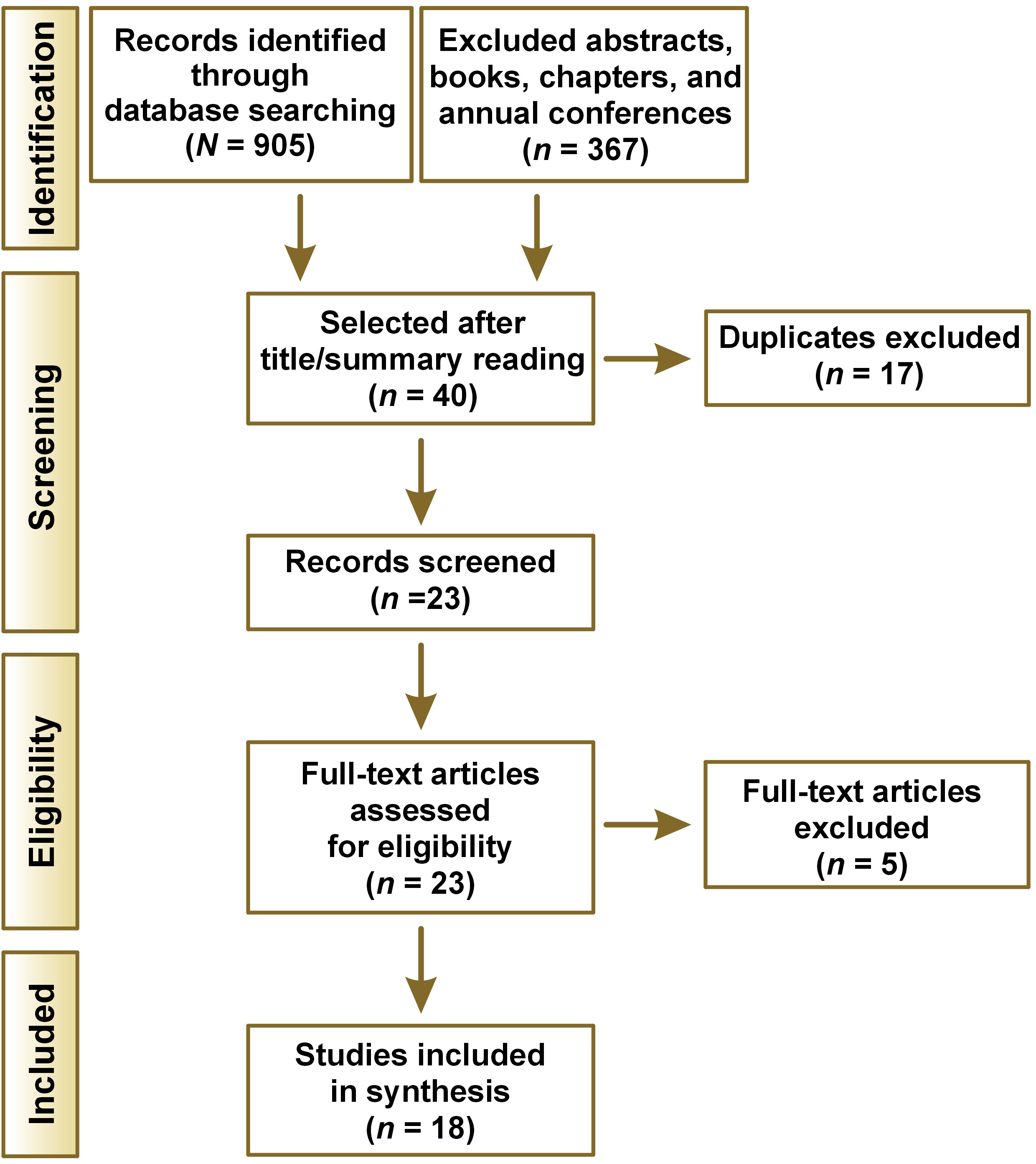
The search for articles is detailed in the PRISMA diagram model (Figure 1). The databases identified a total of 905 articles, of which 367 were excluded as they were from book chapters and annual conferences. Thus, 538 articles were left to read the titles and abstracts. of these, 40 articles were selected. of the 40 remaining articles, duplicates were excluded, and only 23 articles remained. The remaining 23 articles were read in full, and those that did not meet the inclusion criteria were excluded, which resulted in the selection of 18 relevant articles.
Risk of bias
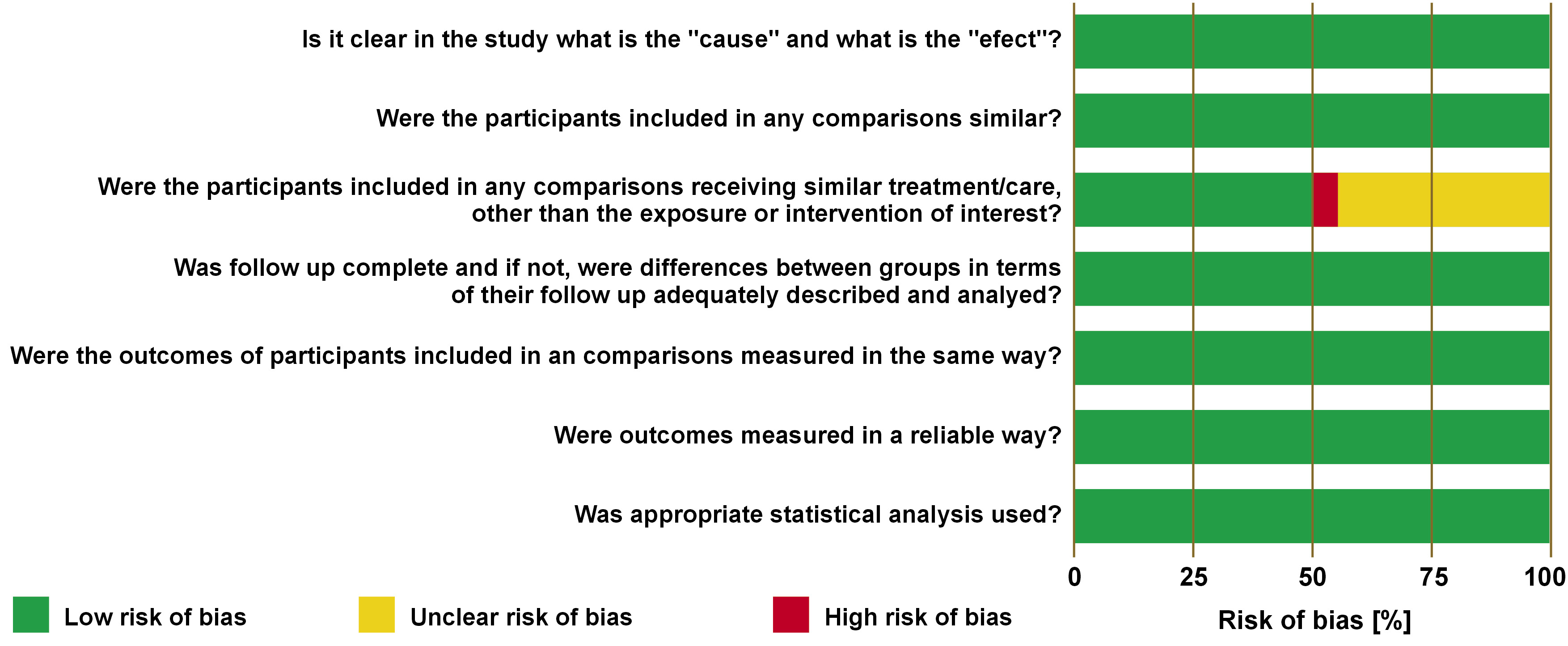
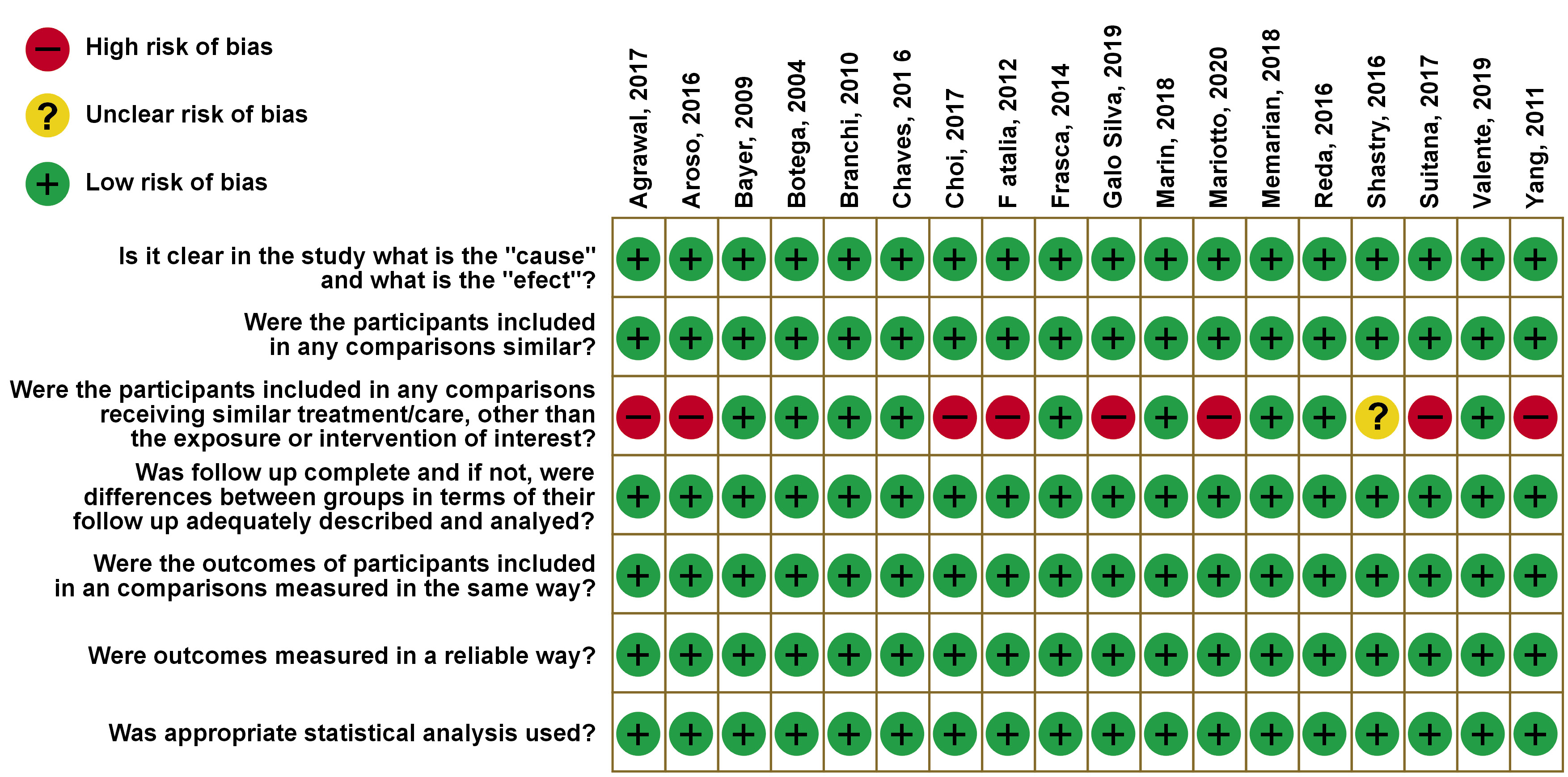
The risk of bias is analyzed following the Joanna Briggs Institute Critical Appraisal Checklist for Quasi-Experimental Studies. Seven questions were analyzed using the answer: high risk, unclear, or low risk (Figure 2 and Figure 3). The questions consisted of the following: Is it clear in the study what is the ‘cause’ and what is the ‘effect’? Were the participants included in any similar comparisons? Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest? Was follow-up complete and if not, were differences between the groups in terms of their follow-up adequately described and analyzed? Were the outcomes of participants included in any comparisons measured in the same way? Were outcomes measured in a reliable way? Was appropriate statistical analysis used?
The principal high risk of bias found in 8 studies was for the question: “Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest?” This is due to the different angles used to determine fatigue resistance in the articles of Aroso et al.,42 Choi et al.,23 Sultana et al.,44 and Yang et al.,43 and also for the thermocycling analysis made by Agrawal et al.,18 Galo Silva et al.,58 and for the Mariotto et al.,59 because they used cleansing solutions to evaluate the fatigue. These are facts that can alter the results in comparison to other studies. One study showed “unclear risk” due to the method used to evaluate the results of the retention. Shastry et al.55 made 100 pulls for the results rather than the cycles that simulate the months like the other studies.
Results of individual studies
The matrix that had the largest decrease in retention in seven studies after the fatigue tests were conventional O-rings.22, 47, 48, 54, 58, 60, 61 One study demonstrated that the ball system presents higher fatigue retention values when the direct capture technique of the O-ring was performed compared with the indirect technique.18 Two studies demonstrated that O-rings made of nitrile had stable retention under cycles.21, 45
Three studies presented matrices with different polymers, such as teflon, polyacetal, polytetrafluoroethylene (PTFE), polyethylene terephthalate (PET), and polyethylene. Three of them – PET, polyacetal and teflon – presented better results with higher retention values.24, 58, 61 One study demonstrated that PET had increased retention through immersion time in distilled water, alkaline peroxide, and sodium hypochlorite.59
One study compared plastic against a metal capsule. The metal material had higher retention and no significant retention loss over time.62 Another study demonstrated that noble alloys displayed an additional retention of 50% in the first 250 cycles, with a small increase until cycle 5,500.61 However, in three different matrixes made of gold, one study showed that the retention values were stable or slightly decreased, but not increased.55 Two studies showed a decrease in retention using titanium material.61 Three studies with angled implants in the fatigue tests showed that with increases in the angle, the decrease in retention is greater.42, 43, 44
Discussion
A limitation of this review was that only in vitro research was used, this fact is because it’s hard to analyze material properties. Due to the heterogeneity of the studies included, it was not possible to perform a meta-analysis. However, all articles included in this systematic review presented analysis and results about the fatigue and retention values of the ball attachment and their components.
Considering cases where all factors are equal, the choice of attachment should be ideally selected based on its composition. Thus, for the selection of the best materials for making components, fatigue resistance becomes an important analysis since it demonstrates which materials can be used for this purpose, clarifying the physical, chemical, mechanical, and biological properties of these, so that the goal is the long-term durability of the treatments.
Allied with the materials, the prostheses must be built in an ideal occlusal-centric relationship, so that the positioning of the condyles is always correct. This avoids an even earlier wear of the prosthetic components caused by a poor occlusal relationship and TMD caused by trauma, parafunctional habits, stress, muscle dysfunction, and bone morphological changes that cause symptoms such as muscle spasms, pain, and changes in joint position and disc displacement due to mandibular malposition.53, 63 Special attention should be given to patients who have already suffered fractures of the mandible, such as the condyle, because they may present facial asymmetry and malposition of the condyle when in contact with the mandibular fossa if they are not treated properly.63 Thus, building the complete denture or overdenture within the correct pattern of centric and occlusal relationships is essential. This allows the homeostasis of the region to be maintained and the rehabilitation treatment to have a good prognosis that does not damage the structures, which will act on different planes.
Treatment with overdentures, whether on teeth or implants, is important to rehabilitate patients. They are beneficial in patients whether they are partial or totally edentulous patients, patients with syndromes such as OFD, which is characterized by the presence of a cleft palate with hypoplastic or even total or partial absences, or patients with TMD such as disc displacement.27, 28 The overdentures, in these cases, can act as a therapeutic treatment, acting to stabilize the disc, close the cleft palate, and improve facial aesthetics and occlusal stability.63 However, special attention must be given to this treatment modality, mainly due to the large number of procedures that are necessary in cases with OFD syndromes, therefore, there must be a very cohesive integration between dental specialties such as endodontics, surgery maxillofacial, prosthesis, and implantology, to achieve effective treatment and prevent early failure of the attachment/prosthesis system.27
With the passage of time, deformation and, therefore, a decrease in the retention of most attachments leads to treatment failure.64 Several studies with parallel implants, angled implants, and innovative capsules were inserted into this systematic review to see how each material reacts to fatigue testing.
The literature reports that values between 5 N and 7 N are sufficient to retain and stabilize an overdenture prosthesis in position during its use.65 Several materials are used to manufacture ball attachments, and the change in material alters the results of the tests, which have different properties.18 In addition, the study method, using parallel implants or not, also produces different results. These differences made it impossible to prepare a meta-analysis, on the other hand, the heterogeneity of the studies adds value to the discussion of research and provides us with important information about different materials used for ball attachments.
Different materials were used for ball attachments,21, 45, 61, 62 which is favorable for discussion since there are numerous O-rings and capsules available on the market. The O-ring is usually composed of nitrile, characterized by its resistance to wear, compression, and corrosion which is the principal factor in the stable retention of this attachment.60 There are also ball attachments made only of metal, which gives greater retention to the system. Other materials that are stable under fatigue resistance are metal systems that use a gold alloy for the retaining component. This alloy presents ductility and malleability that will promote adaptation and maintenance of the contour, which confers retention stability.45, 66 However, its main disadvantage is its high cost, which makes treatment with overdentures more expensive, which takes away one of its main advantages compared to fixed prostheses, for example.45, 66
Polyamide compound O-rings have also been evaluated in this systematic review. These showed a higher retention result than conventional O-rings made of nitrile. This is because polyamide has characteristics such as chemical impact and abrasion resistance, besides offering flexibility, temperature resistance, and dimensional stability. These characteristics can be used to explain the greater stiffness of this type of O-ring.21 Furthermore, matrix and patrix dimensions also influence attachment retention. Larger patrices present higher retention values compared to attachments with smaller dimensions, using the same matrix for both.45
According to several studies that analyze fatigue resistance, it has been demonstrated that with an increase in the number of cycles in the trials, retention tends to decrease in the vast majority of ball attachments, as demonstrated by Fatalla et al.,60 Chaves et al.,48 Reda et al,22 and Memarian et al.47 This fact can be explained by the increase in surface roughness, which can cause plastic deformation of components as the number of cycles increases and consequently there is a reduction in retention.48, 67 Furthermore, this decrease may be due to the different compositions of the plastic materials, as well as the size and shape of the capsules used. Another fact to be considered is the presence of micro-movements, especially if we use parts of different brands in the same retention system.47, 68
Since most current ball attachments suffer from loss of retention, new studies have shown that new attachment designs are made to solve the main problems related to them. As demonstrated by Valente et al.24 and Galo Silva et al.,58 capsules composed of Polyacetal and PET presented with higher retention than the commercial metal O-ring used in their studies. This fact can be attributed to the increase in the roughness and hardness of polymeric materials, as well as the thermal expansion that may have occurred during the experiment, in addition to the design and intrinsic properties of polymers.24, 58 Complementing this analysis, Galo Silva et al.58 and Shastry et al.54 performed thermocycling after fatigue tests and obtained different results, where the capsule made with PET showed an increase in retention, probably due to its thermal stability property.69
It is known that all prostheses on implants should be sanitized so that the treatment is effective and does not have periodontal and peri-implant problems or even loss of dental implants since bacteria can adhere to these materials.70, 71 There is also the possibility that bacteria such as Candida albicans, Streptococcus mutans, and Staphylococcus aureus present in the oral cavity can cause severe diseases, such as bacterial endocarditis, aspiration pneumonia, or generalized infections of the respiratory tract.72, 73, 74, 75 The cleaning and ability to remove the overdenture is an advantage, especially for patients with syndromes, cognitive problems, and patients who have difficulty opening their mouths due to problems such as hyperplasia of the coronoid process, which makes adequate oral hygiene of the prosthetic device unfeasible.27, 28, 76 However, these materials may cause changes in prosthetic components, such as loss of retention, retention gain, or even no alteration, as demonstrated by Mariotto et al., who submitted retention capsules made of polymeric materials in sanitizing solutions and fatigue tests.59 The results obtained are because of the intrinsic characteristics of these materials, which can be hardened with repetitions and solutions, increasing their retention, as well as chemical resistance which will prevent a loss or gain of retention.77
The present systematic review aimed to demonstrate the main reasons that lead to ball attachments and their components to fatigue and treatment failure. Several factors must be taken into account, especially the understanding of the mechanical, chemical, and biological properties of materials, which will be in continuous contact with different temperatures, substances, and forces. Allied with these factors, there is the correct choice of treatment, whether it will be performed with dental implants or natural teeth. This must be guided by strict criteria, observing the different problems that patients may be associated with, such as syndromes, dysfunctions, degree of hygiene, and motor dexterity, so that the treatment has an effective prognosis, increases the quality of life, preserving or restoring health, and has a cost compatible with the patient’s wishes and possibilities. In any case, overdentures and their attachments present a significant improvement in quality of life, aesthetics, masticatory efficiency, retention, and stability, which makes them an excellent rehabilitation option.
Conclusions
The main factor to be considered about fatigue resistance is the retention of these components and their low durability. The loss of retention is due largely to reasons such as the materials that compose the attachments and O-rings, size, angulation of the implants, and time of use of the prosthesis. The mechanical properties had a greater impact on the retention stability of attachments. Thus, the answer to these questions is only possible provided that further research is carried out to understand the biomechanical behavior of the materials and new components to be proposed to provide shorter clinical time spent by the professional with regard to maintenance and that the patient has a lower cost of treatment.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets and all supplementary materials generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.