Abstract
Ultrasound (US) is a widely available, low-cost, non-invasive, and safe medical imaging method that enables real-time observation. Ultrasound offers several advantages for dentomaxillofacial images, such as portability, the possibility of dynamic and repeated examinations, patient comfort, and availability. It is a useful tool for recognizing the temporomandibular joint (TMJ) structures and their involvement during the course of different pathological processes, such as articular disk displacement, joint effusion and cortical erosion. In addition to its diagnostic use, US has been proposed as an auxiliary tool in minimally invasive procedures for arthrogenic temporomandibular disorders (TMD) to achieve an accurate puncture, recognize joint spaces and reduce surgical trauma. While US is widely used for large joints to visualize internal structures and guide the injection, this technique has only recently gained popularity for the TMJ procedures. Hence, the literature on this topic is scarce.
The present review describes the potential advantages and the clinical technique of US guidance for TMJ arthrocentesis and intra-articular injection (IAI).
Keywords: ultrasonography, temporomandibular joint disorders, arthrocentesis, interventional ultrasonography
Introduction
Temporomandibular disorders (TMD) encompass a group of musculoskeletal and neuromuscular conditions that involve the temporomandibular joints (TMJs), masticatory muscles and associated tissues.1 Temporomandibular disorders have been categorized into myogenous (masticatory muscular problems) and arthrogenous (problems with the TMJ components), the latter including internal derangements, arthralgia, osteoarthritis, and osteoarthrosis, which can be manifested by TMJ pain, TMJ noises during jaw function, jaw deviation, and functional limitation.2
Temporomandibular disorders are a significant public health problem affecting approx. 5–12% of the general population, and they are the second most common musculoskeletal condition (after lower back pain).3 Temporomandibular disorders have been identified as the main cause of non-dental orofacial pain, with the most common symptoms being pain aggravated by mandibular function, limited mouth opening and joint sounds (described as “clicking”, “popping” and “crepitus”).1 Orofacial pain affects patients’ social functioning, and physical and psychological well-being. Likewise, the chronic nature of the pain substantially reduces quality of life,4 probably due to the anxiety, stress, depression, physical and social disability, impaired work capacity, decreased productivity, social costs, and reduced economic income, which underscores the need for medical attention.5
General therapeutic goals for TMD involve restoring function, reducing pain, improving quality of life, and reducing the need for future treatment. However, since pain is an individual experience and each patient is exposed to different risk factors, each case should receive a customized therapeutic approach. Additionally, the structural damage may present different degrees of progression, and therefore a therapeutic goal may be different for each patient.6 The management of TMD consists of a combination of medical-behavioral strategies, including non-invasive ones (i.e., patient education, relaxation techniques, coping strategies, home self-care programs, biobehavioral therapy, physical therapy, pharmacotherapy, and orthopedic therapy with occlusal appliances), and minimally invasive and open surgical procedures. In the majority of cases (75–90%), which are either joint or muscular TMD, positive results can be obtained from conservative and reversible interventions,7 but in patients refractory to conservative treatment and/or where anatomical-structural disorders are a substantial source of pain and limitation, minimally invasive procedures can be considered.8 Recent literature suggests that arthrocentesis, followed by the intra-articular injection (IAI) of different therapeutic agents, may be effectively used to treat arthrogenous TMD.2 During these procedures, needle insertion is traditionally performed based on anatomical landmarks (the blind technique), with a potential risk of damage to the surrounding structures. To improve the precision of the procedure and reduce potential surgical damage, US has recently been suggested as an aid to guide punctures during arthrocentesis and IAIs.
The aim of the present review is to describe the potential advantages and the clinical technique of US guidance for TMJ arthrocentesis and IAIs.
Methodology
An electronic search of the medical literature was performed on July 30, 2021 and revised on January 25, 2022. The search was carried out in the PubMed, Scopus and Google Scholar databases, using controlled vocabulary. The authors used both MeSh (Medical Subject Headings) terms and free-text keywords for searching relevant articles. The keywords used were: “temporomandibular joint disorders”; “arthrocentesis”; “injection”; “ultrasound”; and “ultrasonography”. The search strategy was adapted for each database. The search was limited to articles in peer-reviewed journals that were written in the English language. The process was repeated across all databases to ensure that no relevant articles were lost during the identification phase.
Studies conducted on patients (or cadavers) that received TMJ injections and/or arthrocentesis guided by US were considered for inclusion. Studies on humans of both genders without age limitation were taken into consideration. Studies included clinical trials (randomized and non-randomized), prospective and retrospective observational studies, case reports, case series, cadaveric studies, and technical notes, without restriction on the publication date. Only articles available as full texts that presented the descriptors in their title, abstract or main text were included. Narrative reviews, in vitro studies, duplicates between databases, and studies not reporting relevant data were excluded. No limits were applied with regard to the publication status. After verifying the availability of articles, the titles and abstracts of all the records obtained through the literature search were screened, and the full texts of the records meeting the inclusion criteria were retrieved for examination. After screening, the bibliography of the included studies and review articles on the subject were hand-searched for any missed references. All the reported outcomes and methods were identified, and they were recorded in a standardized data extraction sheet formulated in Microsoft Excel with information about: authors; the year of publication; the study design; the condition to be treated (a TMD diagnosis); the number of case subjects; the technique; the joint space (upper or lower); the US transducer; the drug injected; the number of control subjects; the route of US scanning; and the main results.
Results
Search results
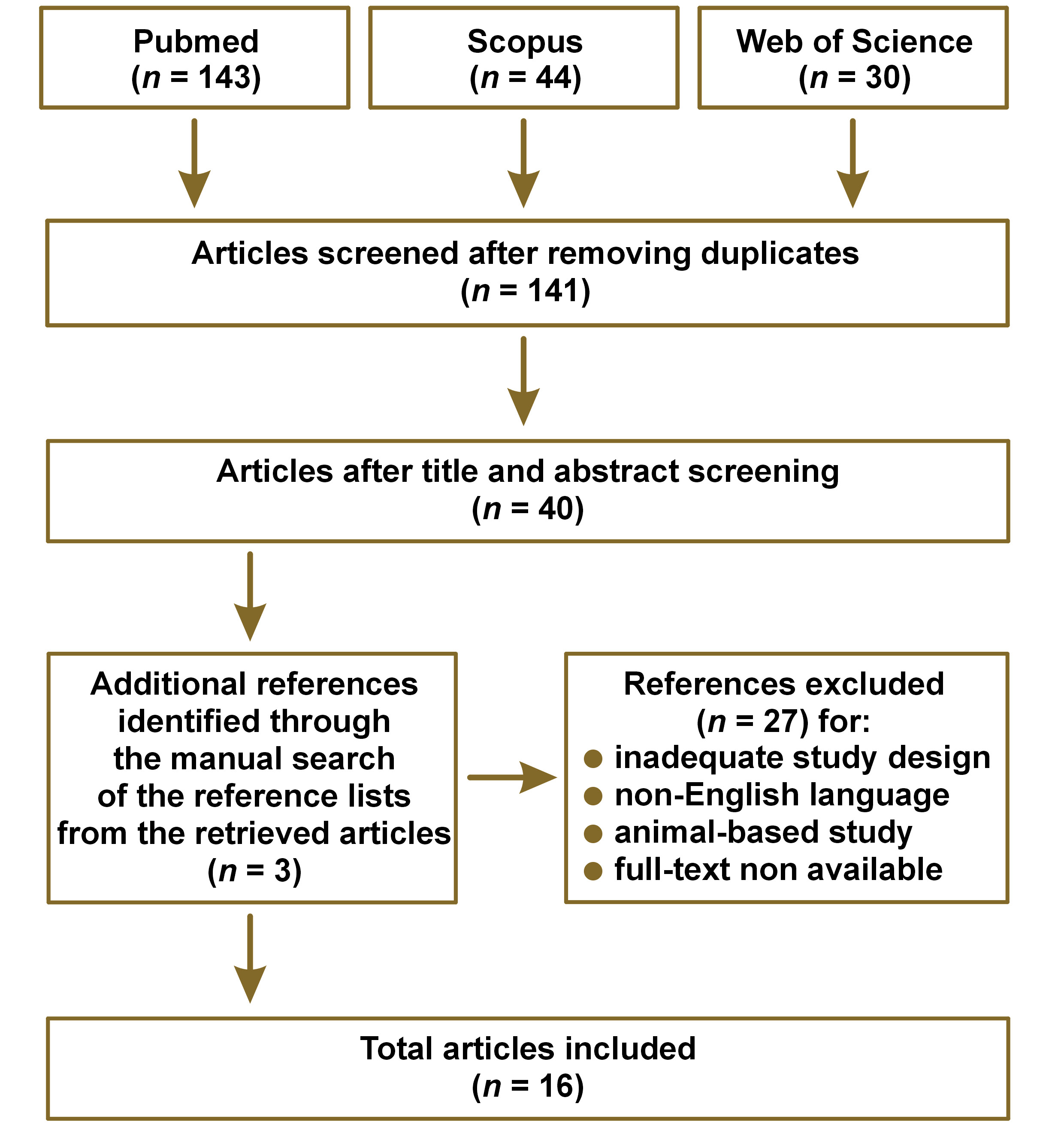
The flowchart for article selection is shown in Figure 1. After the removal of duplicate articles, a total of 141 records were identified, and then screened based on title and abstract. After the inclusion/exclusion criteria were applied, 13 articles were full-text reviewed and 3 additional records were identified through the manual search of the reference lists from the retrieved articles, and were added for a total of 16 articles. Among the selected articles, 4 were randomized clinical trials (RCTs),9, 10, 11, 12 1 was a non-controlled clinical trial (CT),13 3 were retrospective studies (RSs),14, 15, 16 1 was a case report (CR),17 2 were technical notes (TNs),18, 19 3 were cadaveric studies (Cad),20, 21, 22 and 2 were systematic reviews.23, 24 The details of the included primary studies are presented in Table 1.
Minimally invasive procedures for TMJ pain
The literature describing TMJ pain management suggests that non-invasive strategies should precede invasive procedures25; this conservative approach proposes to perform all non-interventional procedures before executing minimally invasive procedures, such as IAI and arthrocentesis to restore jaw function and relieve pain.2 The IAI of hyaluronic acid (HA) alleviates pain and the functional symptoms of TMD.25, 26, 27 However, other drugs, such as corticosteroids (CSs) and non-steroidal anti-inflammatory drugs (NSAIDs), can be used with satisfactory results.25 In a systematic review, Ferreira et al. reported that HA appeared to be more effective for pain resolution as compared to placebo or other therapies in arthrogenous TMD.26
Temporomandibular joint arthrocentesis (first described in 1991 by Nitzan et al.) is a simple, minimally invasive, inexpensive, and highly effective procedure that involves the irrigation of the upper joint space to remove the synovial fluid and inflammatory elements.28 Its main purpose is to clean the joint space, remove inflammatory products, release disk adhesions, reduce pain, and mobilize the joint, for which several techniques have been described in the literature.29 Şentürk and Cambazoğlu classified these techniques based on the number of punctures – either double-puncture arthrocentesis (DPA) or single-puncture arthrocentesis (SPA).30 Single-puncture arthrocentesis is subclassified by the number of needles into 2 categories: type 1 (single-needle cannula method); and type 2 (double- or dual-needle cannula method).29 Recent evidence suggests that SPA is as efficacious as DPA for pain reduction and mandibular range improvement; moreover, there is no superiority of SPA over DPA with regard to the secondary operator-related factors (e.g., the ease of operation, the operating time) and patient-related outcomes (e.g., the range of motion improvement, patient satisfaction).31, 32 In general, arthrocentesis can improve jaw function and reduce pain in patients with disk displacement without reduction and osteoarthritis. However, there are inconsistent findings about its possible superiority over other kinds of treatment for TMJ pain, with the exception of its superiority over splints.33 Furthermore, a meta-analysis by Al-Moraissi et al. showed that non-invasive procedures had significantly lower therapeutic quality in terms of pain reduction and improvement of mouth opening, which supports a paradigm shift in the treatment of arthrogenous TMDs.2 This recent evidence, although based on primary studies of very low to moderate quality, indicates that minimally invasive procedures (particularly in combination with the IAI of platelet-rich plasma (PRP), HA or CSs) are significantly more effective than the conservative treatment in reducing pain and improving mouth opening in the short and medium term in arthrogenous TMD cases. Therefore, minimally invasive procedures should be considered as first-line treatment.2 Nonetheless, a systematic review by Li et al. suggests that when conservative treatment fails, early arthrocentesis may result in the greatest improvement in mouth opening and pain relief; however, when it is applied as initial treatment, without attempting the conservative treatment at first, the outcome may be less satisfactory.34
Temporomandibular joint arthrocentesis seems to be very safe given that a minimal number of major complications have been reported, and the ones reported are generally transitory, mostly due to the effect of anesthetic drugs or the extravasation of fluids to the surrounding soft tissues.35 While the permanent complication rate is 0%, some short-term complications have been reported, such as facial nerve injury, preauricular hematoma, superficial temporal artery injury, the development of an arteriovenous fistula, joint bleeding, intracranial perforation, severe bradycardia, needle breakage inside the joint, failed needle insertion, the leakage of the washing liquid into the extra-articular space, damage to the joint surface, and allergic reactions.29 One promising strategy proposed to prevent some of these drawbacks is US guidance for needle insertion.
Ultrasound fundamentals
Ultrasound is a widely available, low-cost, non-invasive, and safe medical imaging method that enables real-time observation.19, 23 In this method, images are obtained based on the propagation and reflection of high-frequency sound waves in tissues. Ultrasounds are oscillating sounds with frequencies from 2 MHz to 20 MHz, which are beyond the upper limit that humans can hear.36 These sound waves are emitted by a transducer placed on the patient’s skin, combined with a water-soluble gel as a coupling agent.37 The transducer acts as a transmitter and a receiver of acoustic energy, and then transforms it into images.38 The emitted US waves are partly reflected when they pass through tissues, with a reflection coefficient that depends on the characteristics of different anatomical structures.
Ultrasound offers several advantages for dentomaxillofacial images, such as portability, the possibility of dynamic and repeated examinations, patient comfort, and availability.39 Sonograms (US images) are sections of the region of interest, of a particular thickness, generated along the face of the transducer, which are composed of different shades of gray, where the brightness/darkness depends on the frequency of the reflected echoes, which in turn depends on the ability of a tissue/structure to reflect or absorb sounds; this concept is known as echogenicity. In sonograms, tissues are classified according to their echogenicity: hyperechoic or echogenic (very bright) – highly reflective tissues, such as bone or cartilage; moderately echogenic (bright), such as glands; hypoechoic (fairly dark), such as blood vessels and muscles; and anechoic (very dark), such as liquids and air.36
A US examination is a procedure that is highly dependent on the skill and experience of the operator. Differences of opinion between researchers/clinicians may be due to the lack of standardization in the performance of the examination,40 probe selection and the configuration of equipment, all of which may generate differences in the interpretation of the results.41 Nevertheless, researchers have proposed the use of US as a promising screening tool for the evaluation of maxillofacial structures, such as TMJs.11, 36, 37, 39, 41
Ultrasonographic features of TMJ
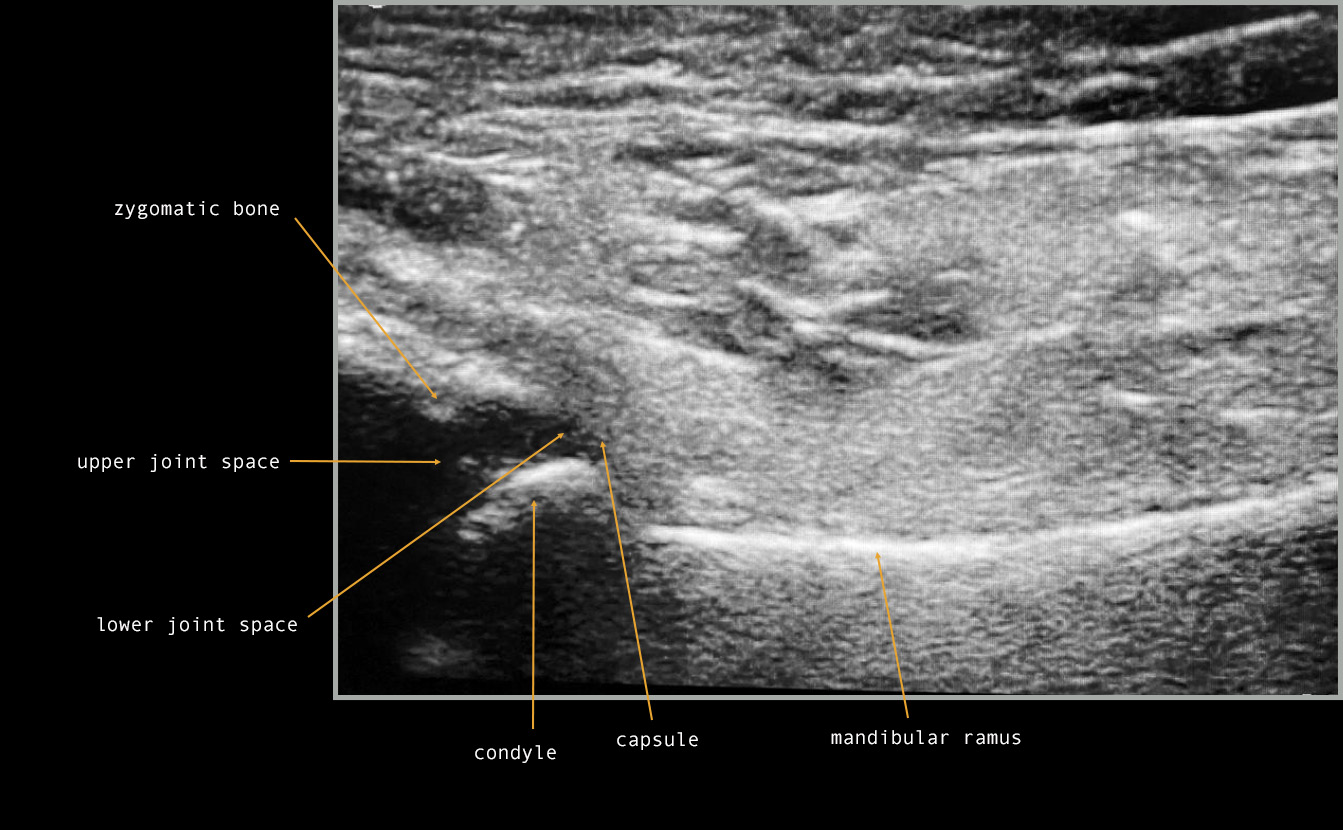
The TMJ area has some particularities, including a small examination area, limited access to deep structures and a high risk of sound reflecting from the bone tissue, which can make image interpretation very complex.38 Soft tissue visualization is severely limited by bone, as sound energy is almost completely absorbed by soft-tissue interfaces and the bone tissue. Thus, the external placement of the transducer enables only the acquisition of the lateral third of the joint, and only in the axial and coronal planes.37 Therefore, the main disadvantage of US in the TMJ area is the limited imaging of the upper and medial parts of the condyle and the disk; these structures are hidden by the acoustic shadowing caused by the rebounding and absorption of US waves by the zygomatic bone.12, 19, 20, 42 The TMJ images produced by US depend on the echogenicity of tissues as follows: the condylar head and the articular eminence are hypoechoic and appear black39; the bone margins are hyperechoic and appear white39; the connective and muscular tissues are isoechoic (an intermediate reflection of sound waves) and appear heterogeneously gray23, 39; the joint capsule surface is highly reflective of sound waves, creating a hyperechoic line (white)11, 23, 39, 42; the articular disk appears as a thin, hypo-to-isoechoic, homogeneous band11, 23, 42; articular fluid-filled spaces are hypoechoic and appear black,11, 23, 42 although these are virtual cavities that are generally not detectable unless joint effusion is present38; bone marrow is usually hypoechoic and appears black.38
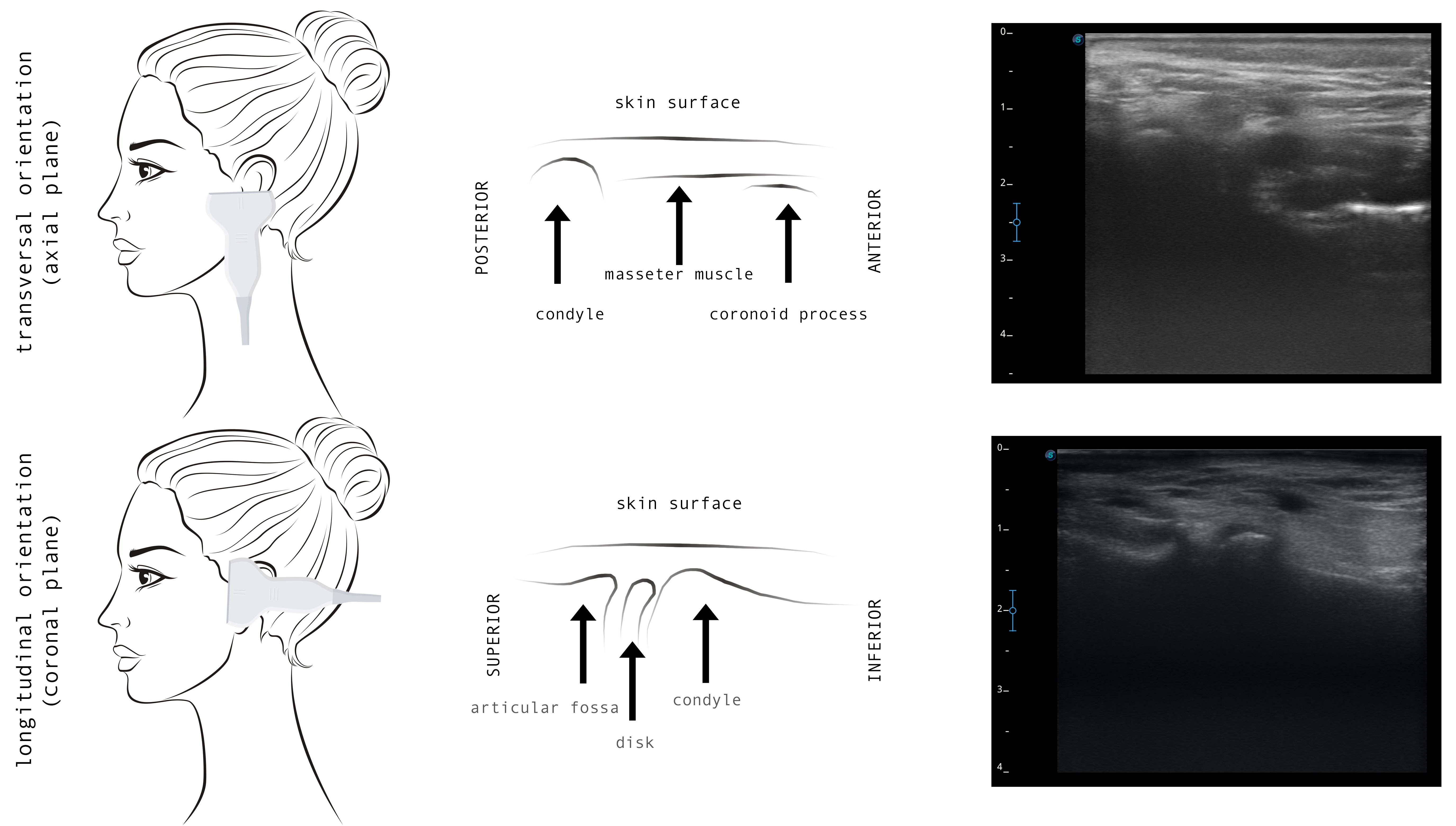
In most publications, TMJ US monitoring is based on the standardized protocol of Emshoff et al.43 Most studies have adopted similar protocols, which include transversal and longitudinal scans to evaluate the joint compartments in the coronal, axial and oblique planes (Figure 2).41 During the longitudinal scanning, the probe is placed over TMJ, perpendicular to the zygomatic arch and parallel to the mandibular ramus, and inclined until the best view is achieved; then static and dynamic evaluations are performed (Figure 3).38 The performance of the US diagnostics is outside the scope of the present review and has been extensively described for 3 main diagnostic domains: disk displacement; joint effusion; and cortical erosion.38, 40, 41, 42, 44 It has been suggested that US can complement a clinical examination as an initial evaluation tool.40
Ultrasound-guided minimally invasive procedures for TMJ pain
In addition to its diagnostic use, US has been proposed as a useful tool in interventional procedures, such as US-guided peripheral venous access, central venous access, abscess drainage, the aspiration of hip and shoulder joints, pleural effusions, paracentesis, and TMJ arthrocentesis.11 It has been suggested that US may allow more precise execution with real-time observation.45 The lysis and lavage of the upper joint space is an effective method for controlling TMJ pain, so identifying this space is important for a satisfactory procedure.11 However, the traditional blind technique (based on anatomical landmarks) requires experience to reach the upper joint space and carries a potential risk of damage to the collateral disk ligaments and the adjacent soft tissue, especially if multiple attempts are made.18, 20 Furthermore, the confirmation of the correct needle placement can sometimes be ambiguous in clinical practice.20 Given the complex TMJ anatomy, clinicians have used image-guided techniques to aid the verification of the needle position, and reduce potential damage to joint tissues and neurovascular structures, or needle penetration in the middle cranial fossa during minimally invasive procedures.12, 21, 23 Some image-guided techniques using magnetic resonance imaging (MRI) or cone-beam computed tomography (CBCT) have shown promising results; however, their routine use is not feasible in The MJ procedures due to cost and the need for a hospital environment.23 On the other hand, it has been postulated that US-guidance minimizes trauma to the joint, and improves the accuracy and efficiency of the procedure. Furthermore, real-time images, the lack of ionizing radiation and easy access make US a promising aid for minimally invasive TMJ procedures, such as arthrocentesis and IAI.23 While US is widely used for large joints to visualize internal structures and guide IAI, this technique has only recently gained popularity for the TMJ procedures. Hence, the literature on this topic is scarce. The articles regarding US-guided TMJ arthrocentesis or IAI available in PubMed, Scopus and Web of Science, published since 2010 are listed in Table 1 (the main characteristics are provided to facilitate the comparison of the studies). The uncontrolled RT by Parra et al. from 2010 was the first to report the accuracy of US-guided TMJ IAI; they observed that the needle was located intra-articularly in 91% of cases.14 Dayisoylu et al. (2013) were the first to describe a reliable technique for US-guided TMJ arthrocentesis, which was suggested to be “better than arthroscopy” with regard to cost-benefits.18
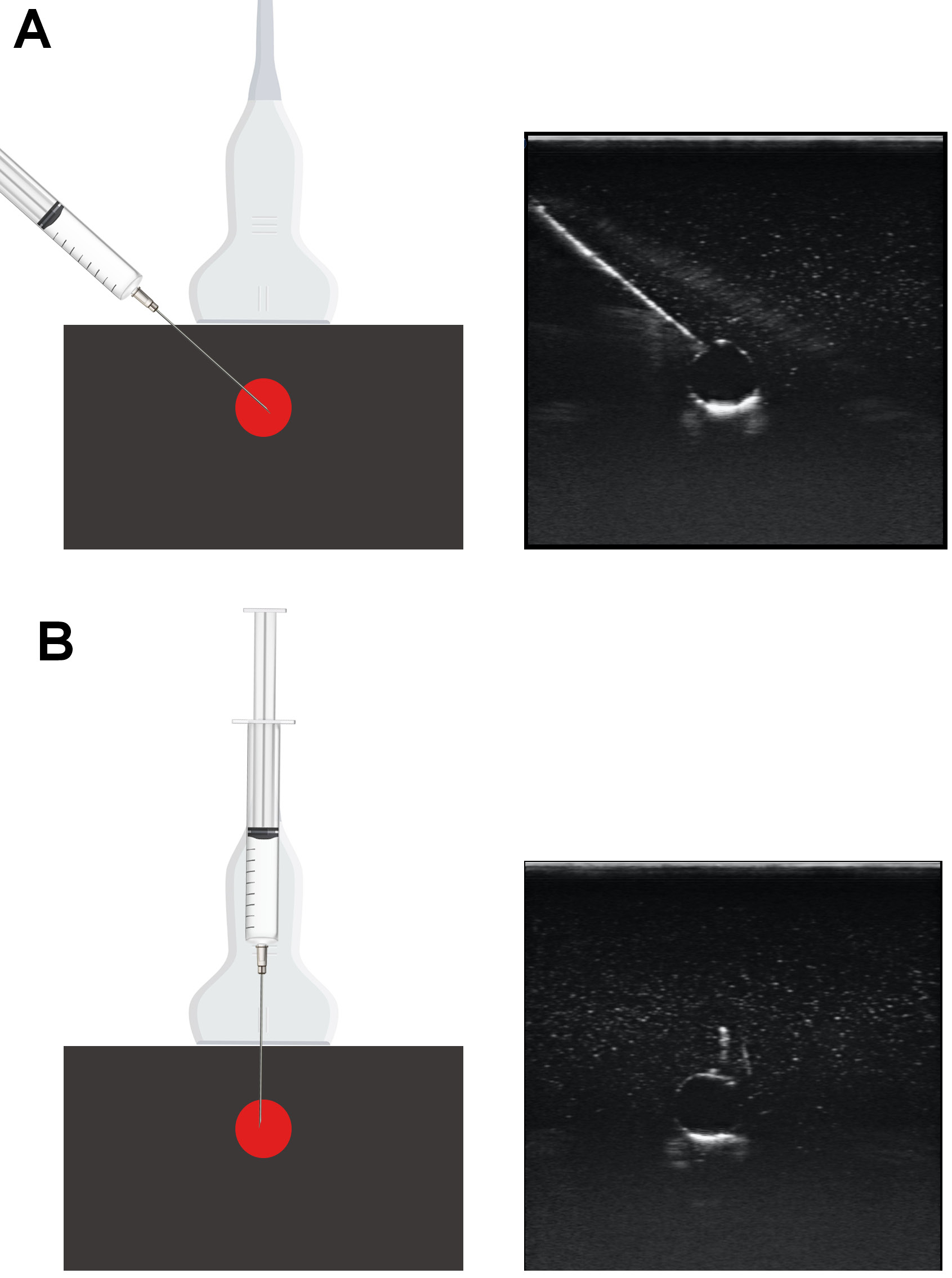
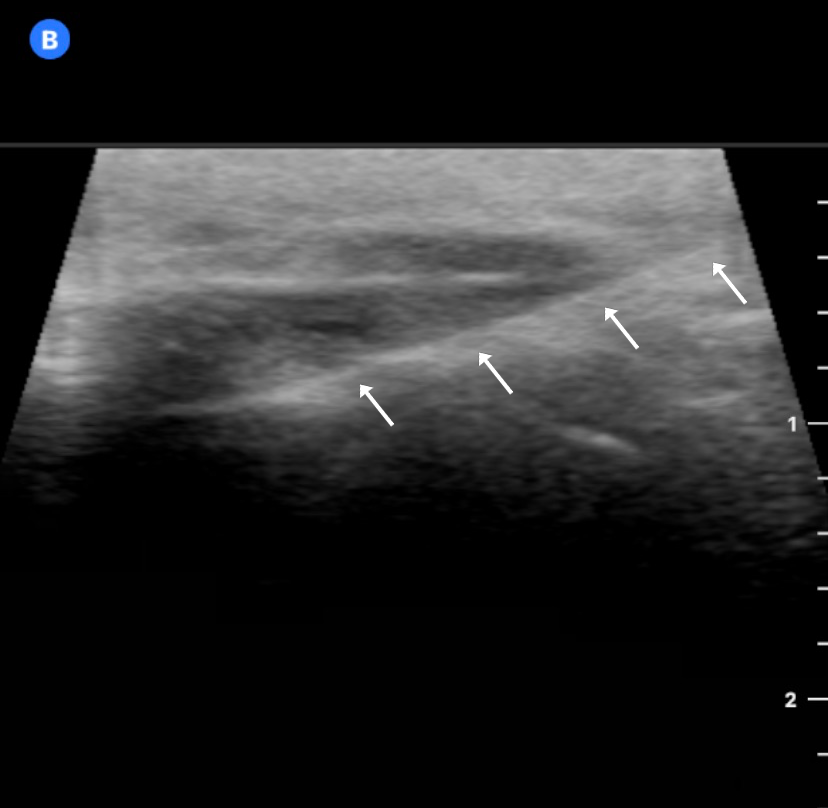
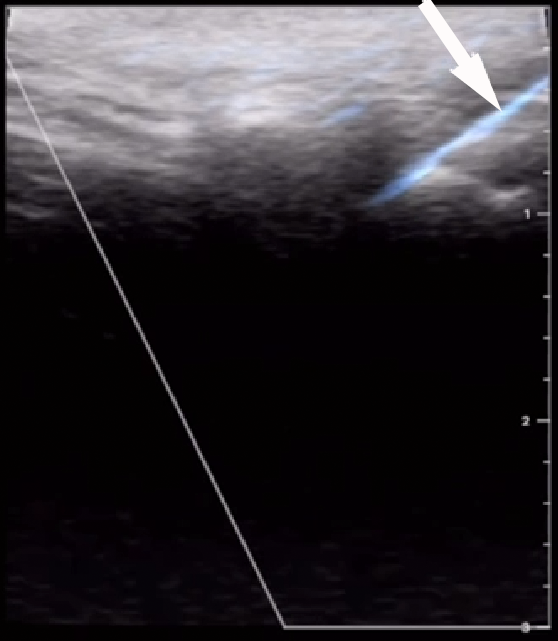
Ultrasound-guided punctures may approach the target (joints, vessels or nerves) from a position perpendicular or parallel to the US beam, referred to as ‘out-of-plane’ and ‘in-plane’, respectively (Figure 4). The in-plane approach enables the operator to visualize the needle shaft and tip, as it is directed toward the target, but it requires skill and may result in a false sense of security, despite having been demonstrated to result in faster and more accurate performance. On the other hand, the out-of-plane technique is more difficult and relies on tissue movement or fluid localization rather than strict needle visibility to confirm its position.46 In the TMJ US-guided injections using the out-of-plane approach, the correct position of the needle is achieved by extending and narrowing the joint space by the infiltration and aspiration of fluid, respectively.19 Champs et al. validated a longitudinal US-guided in-plane approach for TMJ IAI, in which the needle is inserted at an angle of 30°, with the US probe in the preauricular region, approx. 1 cm in front of the tragus, parallel to the mandibular ramus and perpendicular to the zygomatic arch.21 This technique proposes a direct visualization of the needle all the way to the joint with great precision and provides noticeably higher accuracy during puncture.21 Most clinical and cadaveric studies use the coronal route of scanning and in-plane needle insertion (Figure 5),9, 10, 11, 12, 14, 17, 18, 19, 20, 21 whereas other reports did not report these technical details.13, 15, 16
Most articles describing TMJ minimally invasive procedures (and daily clinical practice) are based on washing-out the upper joint space in both the US-guided and blind techniques. Nevertheless, some evidence has demonstrated that IAI directed to the lower or both TMJ spaces has a better effect than IAI into the upper space alone.47 Lower joint space injection is believed to be a difficult procedure because of a narrow space, a small volume and the ‘hidden’ location. The blind technique for lower joint space injection was described by Li et al.47 Clinical information on US-guided IAI into the lower joint space appears to be very limited.20 Levorova et al. reported a technique for US-guided TMJ intra-articular infiltration directed toward the lower joint space (Figure 6).19 Cha et al., in a cadaver-based study, observed that upper joint space injection showed a similar level of success for the blind and US-guided techniques.20 However, for the lower joint space, the US-guided technique had a significantly higher success rate (90% vs. 30%) and the blind technique was associated with a considerable proportion of unsuccessful/inappropriate injections to the lower joint space.20 To date, only 4 controlled CTs that compare the blind and US-guided techniques for TMJ arthrocentesis have been published.9, 10, 11, 12 Two of them used DPA9, 10 and the others used type II SPA11, 12 (the comparison of these studies is presented in Table 1). Şentürk et al., in a CT, reported the longest follow-up (1 year) in a comparison between the blind and US-guided techniques for TMJ arthrocentesis.12 The results show that US guidance is effective in type 2 SPA, as it aids the visualization of the needle during puncture; however, it did not resolve pain or improve the range of motion as compared to the blind technique.12 The clinical effectiveness of US guidance for TMJ arthrocentesis and IAI is mostly analyzed based on 4 aspects: pain reduction; the range of movement; needle positioning (or repositioning) attempts; and the total procedure time. The literature comparing US-guided arthrocentesis vs. the blind technique is scarce. Two systematic reviews have been published recently,23, 24 in which very similar conclusions were reached, since they both selected the same articles for the final analysis.9, 10, 11, 12 Both reviews found no significant differences in pain reduction and the maximum mouth opening, no conclusive results were observed in reducing needle repositioning, and also data on the potential to reduce the procedure time was inconclusive.23, 24 Although achieving access to the joint space occupies most of the surgical time, studies show that the total time is longer in the US-guided procedures, since a US examination itself requires additional time.9 These conclusions are shared by all studies, as some publications suggest that US guidance would improve the precision of needle placement, especially when the lavage of the lower joint space is performed.20 Cadaver-based studies observed that US-guided IAI and arthrocentesis techniques had a higher accuracy when the needle was located inside the joint spaces,20, 21 as they provide the image verification of having punctured the joint space and the real-time screen visualization of the distension of the space after infiltrating fluid.22 Antony et al. observed that the US-guided technique resulted in a significantly greater pain reduction in the immediate postoperative period.10 Bhargava et al. found that in type 2 SPA, US guidance minimized the number of attempts of needle manipulation as well as possible complications, and provided easier access to the upper joint space.11 Additionally, Anthony et al. suggested that in patients with obesity, US-guided arthrocentesis could be more precise in locating the joint spaces, whereas the blind technique arthrocentesis required multiple punctures to achieve successful lavage.10
Finally, from a clinical point of view, some technical suggestions can be made for the execution of US-guided TMJ intra-articular procedures12, 18, 19, 48: 1) always perform an initial US TMJ evaluation to observe anatomy in the coronal and axial views; 2) use high-resolution (over 12 MHz) linear probes22, 38; 3) administer a local anesthetic solution (lidocaine or mepivacaine, without a vasoconstrictor) with a 27-gauge needle into the TMJ capsule,48 otherwise, the auriculotemporal nerve blockage may be needed; 4) it is not necessary to use anatomical reference landmarks when puncture is guided by US imaging22; 5) after reaching the upper or lower joint spaces, HA, CSs or platelet concentrates should be injected slowly; 6) washing the articular space with saline or Ringer’s lactate solution if arthrocentesis is intended; 7) close the injection area using a sticking plaster with light pressure to avoid the formation of hematoma; and 8) use ice or cold-pack applications and NSAIDs after the procedure.48
Conclusions
This review summarizes the recent evidence regarding the use of US as an auxiliary tool in minimally invasive procedures for arthrogenic TMD. Ultrasound guidance has shown promising advantages; it reduces the number of needle placement attempts, minimizes trauma to TMJ, improves the accuracy and efficiency of joint injections, results in a significantly greater pain reduction in the immediate postoperative period, provides easier access to both joint spaces, and has a significantly higher success rate when lower joint space injection is attempted. Future research is required to confirm the impact US may have on the clinician’s performance, and the consequent benefit to the patient.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.