Abstract
The management of complex dental trauma can be modulated according to the emergencies that may arise over time. Clinical management of transverse root fractures may require different therapies based on situations, such as delay and error in the treatment of an avulsion trauma associated with apical third root fracture, patient’s poor compliance, or external and internal root resorption. The primary aim of this article was to review studies regarding root fractures in the permanent dentition and root fracture management. The secondary aim was to present the inflammatory reaction and the complications (i.e., infections) that may occur if the International Association for Dental Traumatology (IADT) guidelines are not followed. In addition, a scenario is devised in which endodontic surgery, despite the baseline patient’s conditions and negative prognosis, can help to inhibit the inflammatory root resorption and allow the preservation of soft and hard tissues within a long follow-up from the injury, for the purpose of demonstrating the next possible implant-prosthetic rehabilitation.
Keywords: dental trauma, avulsion, root fracture, apicoectomy, scanning electron microscopy
Introduction
Avulsion of a permanent tooth occurs in 0.5–3% of all tooth injuries. It is most common in young permanent dentition and it mainly affects the maxillary central incisors.1 Tooth avulsion injuries are common in childhood and adolescence as a result of accidental falls, road accidents and shocks in sports.2 Numerous studies have shown that tooth avulsion is one of the most serious tooth injuries and, compared with other types of dental injuries, its long-time prognosis is highly dependent on the actions taken immediately after the trauma. In most situations, replantation is the treatment of choice, but this cannot always be performed immediately. Moreover, the prognosis of a tooth injury depends mainly on the management of the dental trauma and is closely related to the complexity of the injury itself.
Dental avulsion management must adhere to the international guidelines.3 Timeliness of the procedure, preservation of the tooth on a physiologic storage medium, adherence to the date of root canal treatment and proper splinting are of fundamental importance to prevent inflammatory root resorption and ankylosis caused by infection of root canal system and by damage and loss of viability of periodontal ligament (PDL) cells.4
The complexity of a tooth trauma depends on the simultaneous presence of multiple lesions on the same tooth element, such as a tooth avulsion associated with a root or crown fracture, or the presence of a bone wall fracture. Transverse root fractures may occur as a concurrent injury with crown fracture, concussion, subluxation, lateral luxation, extrusion, or avulsion of the coronal fragment. The most common concurrent injuries are concussion and subluxation. Unfortunately, studies reporting the incidence of the various dental injuries have not reported how often these concurrent injuries co-occur with root fractures.5, 6 Additionally, these injuries almost always occur at a young age due to the greater liveliness of children.7
The trauma is often connected not only to the teeth but also to the jaw and, more specifically, to the temporomandibular joint (TMJ). The traumas to the TMJ can cause temporomandibular disorders that may last for a long time along with occlusion modification, pain and facial asymmetry.8, 9 Orofacial traumas can be clinically less evident and cause only enamel loss, but over a long time they can cause hypersensitivity of the tooth or loss of pulp vitality.10, 11 To prevent dental or TMJ trauma in certain risk categories, such as subjects who practice extreme sports or patients with high risk factor, the use of a mouth guard is recommended.12
Patients with increased overjet, amelogenesis problems, syndromic patients, as well as neurological (epilepsy) or psychiatric patients commonly suffer from dental trauma. For example, syndromic patients are at high risk of severe malocclusions, dental malformations and poor oral hygiene due to the lack of collaboration13 that can cause destructive caries which lowers tooth resistance.14, 15, 16, 17, 18
In cases of trauma, it is essential to inform patients and their caregivers about the therapeutic protocols and follow-up periods. Nowadays, information can easily be distributed via the Internet and telemedicine.19, 20, 21
The complexity of dental avulsion cases requires an appropriate multidisciplinary therapeutic approach, which must consider periodontal, orthodontic, surgical, and prosthetic issues. A long-term prognosis, entailing the need to face various clinical scenarios (e.g., tooth ankylosis, loss of bone support, implant rehabilitation in adulthood) should also be taken into account.22, 23 In most cases, the replantation of the tooth and its preservation over time help to protect the alveolar bone around the site of the trauma and may offer significant long-term advantages in preparation for definitive implant-prosthetic treatment.24
The primary aim of this article is to review the literature regarding root fractures in the permanent dentition and their management. The secondary aim is to present the complications that may occur if the international guidelines are not followed.
Material and methods
A narrative literature overview to discuss the management of dental root fractures was carried out. Case definitions and classifications, diagnostic considerations, and the clinical protocol of the emergency management and inflammatory reaction were reviewed and analyzed.
Root fractures
Epidemiology and classification
Dental root fracture involves the dentin, cementum and pulp. The fractures can be vertical or transverse.1, 5 Vertical fracture usually requires tooth extraction and prosthetic rehabilitation. Transverse root fracture can be oblique with varying orientations and is classified as: i) fracture of the apical third of the root; ii) fracture of the middle third of the root; iii) fracture of the coronal third of the root that can be: a) subcrestal; or b) supracrestal.
Physiological responses and healing
According to Andreasen et al.,1 the existing physiological responses of the tooth and its associated tissues to root fractures are as follows:
– healing with hard dental tissue interposition;
– healing with connective tissue interposition;
– healing with bone and connective tissue interposition; and
– no healing with inflammatory granulation tissue interposition in the fracture line, as a result of pulp necrosis and infection of the pulp space in the coronal fragment.
The pulp and PDL cells are stimulated only in the first case, and in 0.5–7% of cases almost complete restitutio ad integrum is achieved.1 The infection of the canal system and necrosis of the apical and coronal fragments of the tooth are the reasons for the lack of healing in 22% of teeth with root fractures.6
Emergency management
Emergency management depends on the displacement of the coronal fragment and the level of the root fracture.6
Lateral luxation or extrusion of the coronal fragment require repositioning back into the sockets. If the avulsion of the coronal fragment has occurred, it should be managed as a tooth avulsion.6
The management of root fractures in the apical and middle thirds, as well as those that are subcrestal in the coronal third of the root, require the same conservative protocol. However, supracrestal fractures in the coronal third are managed differently.6
Clinical protocol
Repositioning and splinting
If the coronal fragment is displaced, it should be repositioned, and a splinting should be applied. Splints should be made by stainless steel wire bonded with composite resin to the labial surface of the affected tooth and to 1 or 2 teeth on either side of the affected tooth. Splints should restrict the movement of the coronal fragment. Rigid stabilization offers the best conditions for healing and, if present, a splint also stabilizes the fracture of alveolar bone. The recommended duration of the splint use is from 4 weeks up to 4 months.6
Root canal treatment
Since the prognosis for pulp recovery is favorable, root canal treatment should not be initiated at the emergency appointment. The clinical approach is to “wait and see”. Moreover, maintaining the pulp vitality allows for the possibility of healing with hard dental tissue interposition.6
Antibiotic therapy
Antibiotics are not indicated unless the coronal fragment has been avulsed.6
Follow-up
Regular follow-up is essential and should be performed at 4-week intervals while the teeth are splinted, and then at 3-month intervals for the first year.6
Management of the inflammatory reaction and complications on an infectious basis
Clinical cases may present with varying degrees of complexity that may not always be diagnosed in the time frame indicated in the International Association for Dental Traumatology (IADT) guidelines. In fact, if the guidelines are not followed, infectious complications may occur, which often require a more complex clinical strategy, such as the removal of broken apices due to the lack of improvement or endodontic surgical resection.
Complications of infection
On some occasions, patients are diagnosed only after a significant amount of time has passed since the injury. The vast majority of these are patients of developmental age (i.e., adolescents or young adults). In such situations, it is not possible to follow the management protocols included in the IADT guidelines. Dental trauma and its incorrect management can lead to consequences with a major impact on dental esthetics and oral health-related quality of life. Dental trauma may involve the 2 maxillary central incisors and a fracture of the apical third of the roots, fracture of the alveolar process on the palate or buccal side, or a complete tooth avulsion of the coronal fragment.
Infections may occur if the international guidelines for the treatment of root fractures are not followed, in particular, if the teeth are dry stored after the avulsion, and then are reimplanted and splinted using a fixed orthodontic splint, as well as if the patient does not undergo endodontic treatment to remove the splint. The most frequent infections are repeated abscess episodes that affect the teeth involved in the trauma. The results of clinical examination show spontaneous pain and dull sound of the involved teeth upon percussion, light teeth extrusion, poor oral hygiene and mobility evaluated based on Miller’s classification. In such cases, routine radiological examinations (intraoral X-ray images) are prescribed.
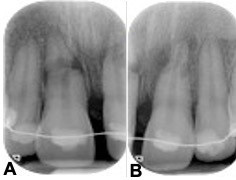
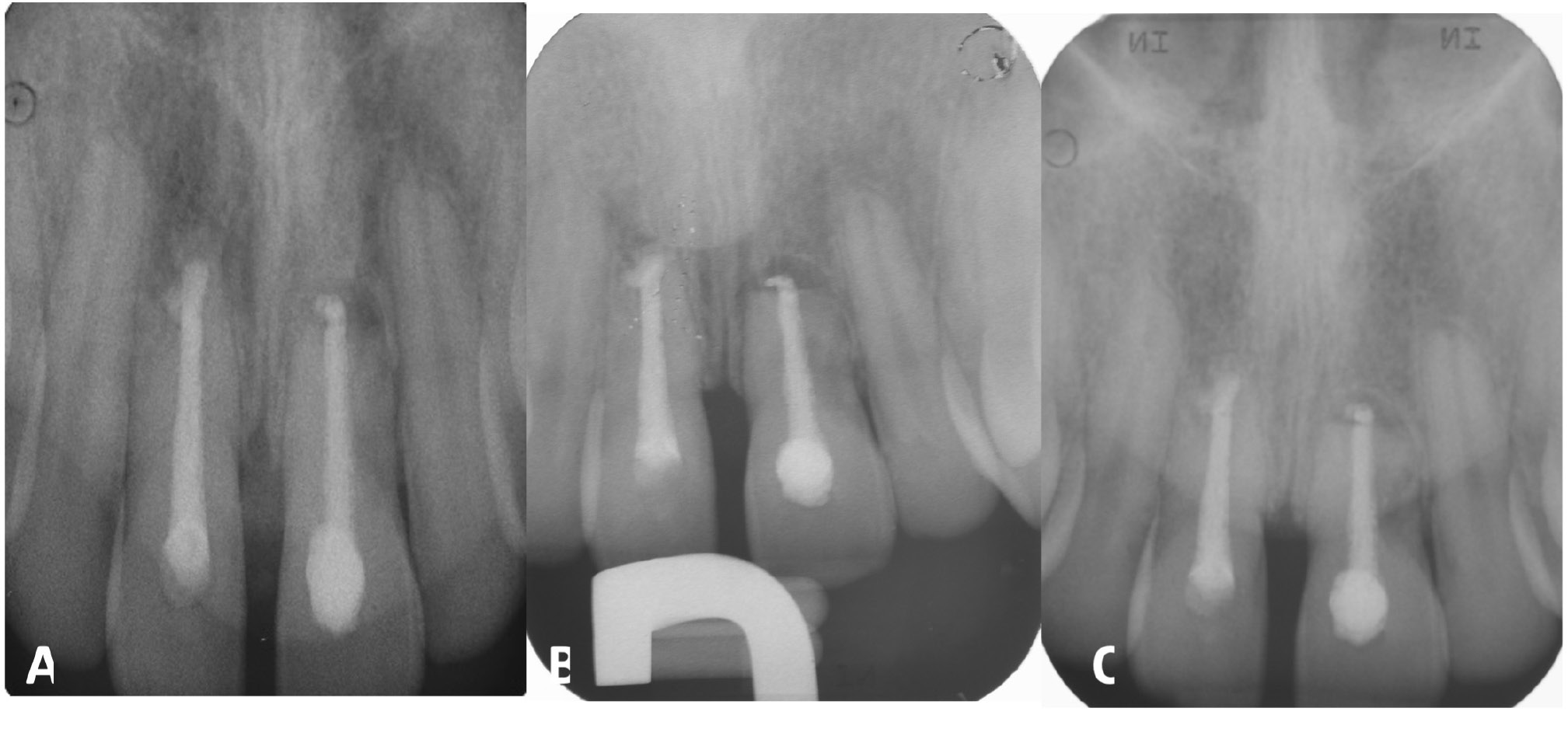
The radiological aspect of no healing is shown in Figure 1. No healing occurs if the pulp of the coronal fragment becomes necrotic and infected, with interposition of granulation tissue that extends into the adjacent bone and evidence of radiolucency extending laterally. Figure 1 also shows external inflammatory resorption in the apical third of the root and signs of bone periapical radiolucency.
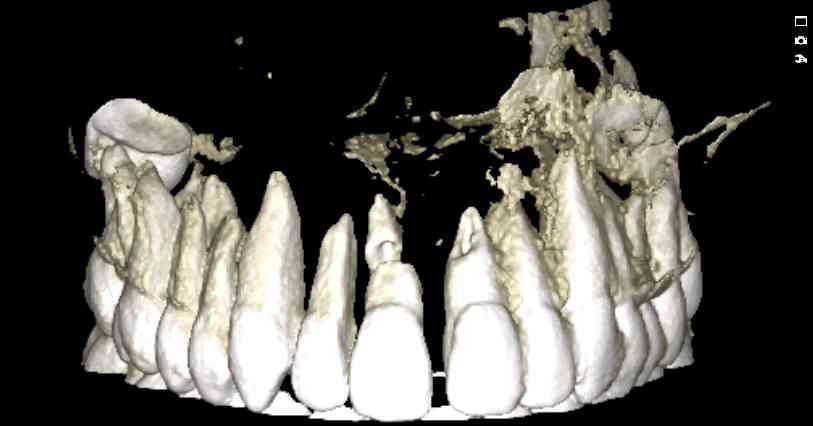
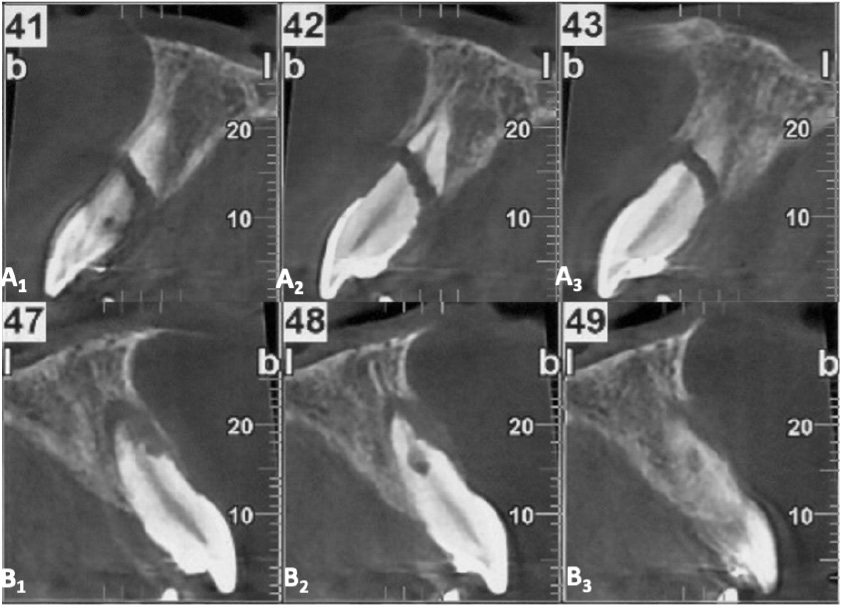
Cone beam computed tomography (CBCT) may often be required as a follow-up to assess the involvement of surrounding tissues, the amount of external and internal root resorption on the involved teeth, the anatomy of the root fracture of the apical third, and displacement of the coronal segment. Figure 2 and Figure 3 illustrate CBCT parasagittal images that confirm the results of the intraoral radiographs. The diastasis between the coronal and apical fragments of #11 appear to be more evident on the fracture line and the presence of a “new apical foramen” is highlighted. In addition, areas of external inflammatory resorption on the apical fragment are evident and the fracture line appears jagged. The images relating to #21 appear suggestive for external inflammatory resorption, particularly on the vestibular side, which is the site of concomitant bone inflammation in the parasagittal image #48. Internal pulp resorption can also be observed at the apical third of the root.
Endodontic surgical resection
in cases of persistent infections
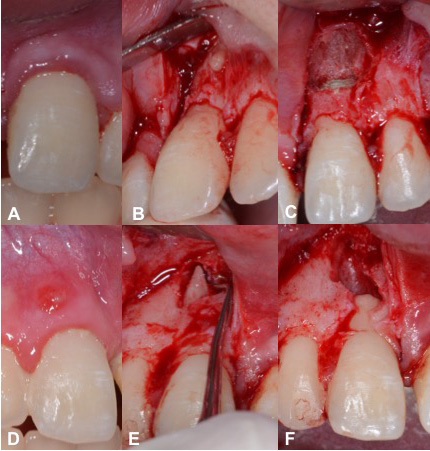
The inflammatory reaction that results in no healing is caused by the infection of the root canal system. In cases of root fracture, the infection occurs at the fracture site rather than in the periapical tissues. The coronal fragment has a “new apical foramen,” which is now situated at the fracture line rather than at the apical end of the root. Root canal therapy of the coronal fragment can be initiated and calcium hydroxide intracanal medication can be administered. If symptoms persist (i.e., abscess episodes and/or mucous fistula), an apicoectomy can be performed. Figure 4 shows the fractured apical root fragment being removed and retrograde closure of the new root apex,25 which in one case is at the apicectomy level #11 and in the other at the root fracture line #21.26, 27
Inflammatory root resorption and its effects
on the morphology of dental hard tissue
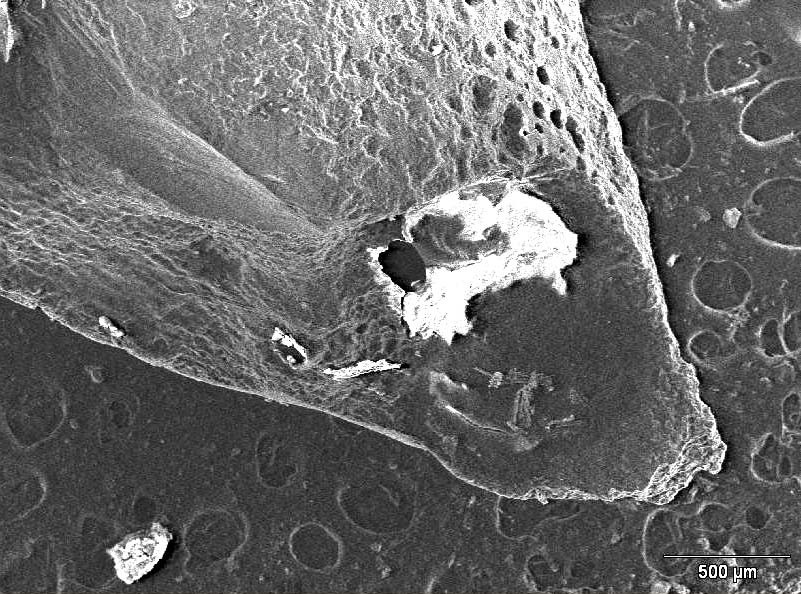
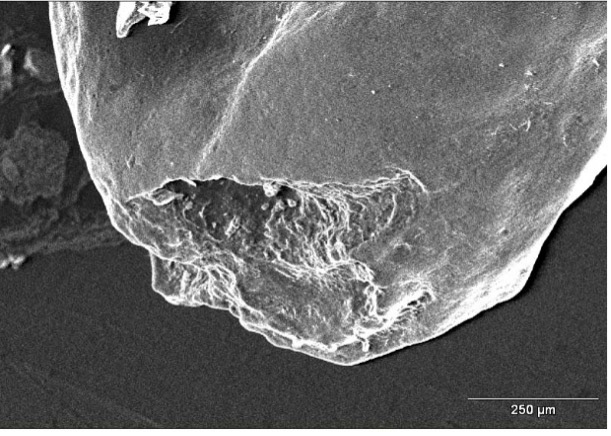
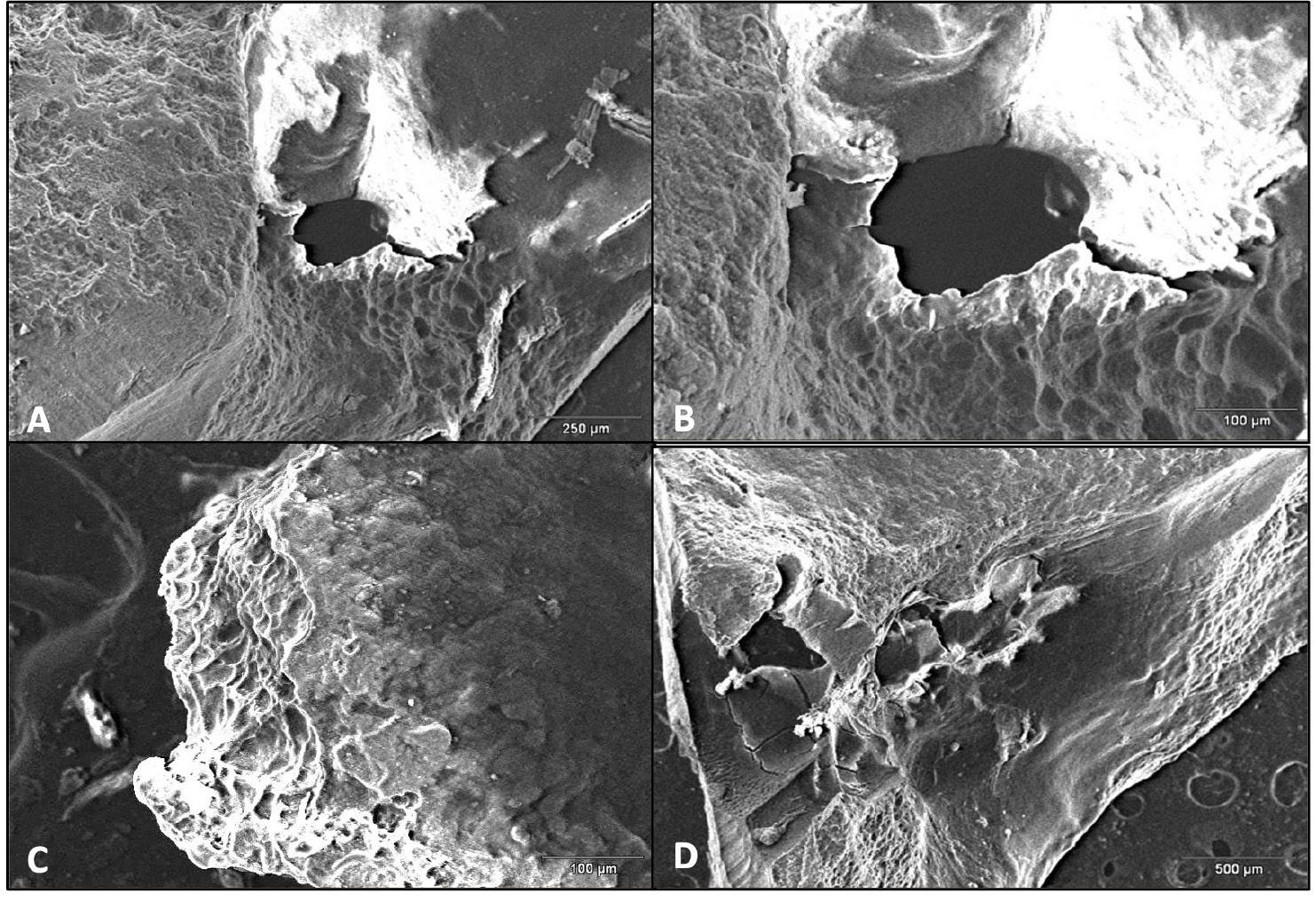
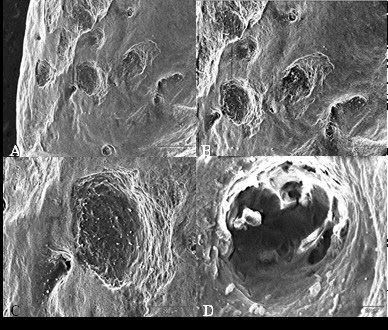
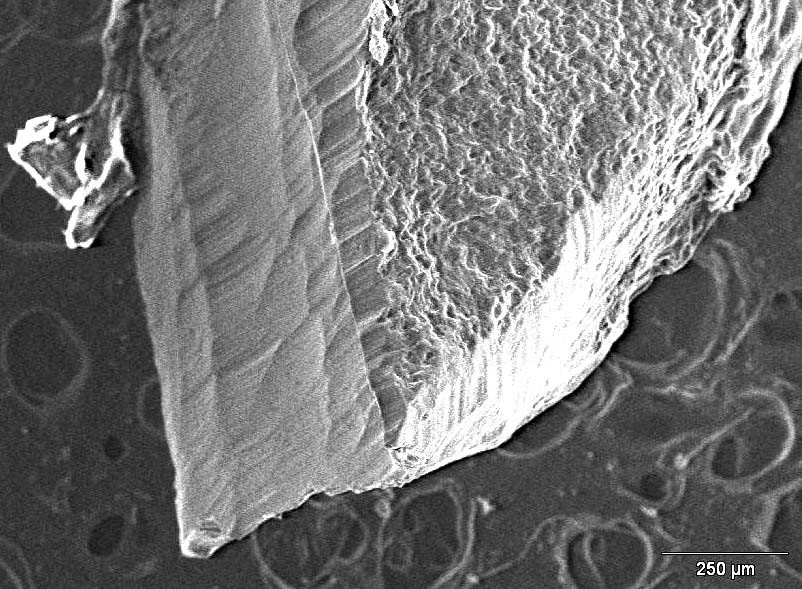
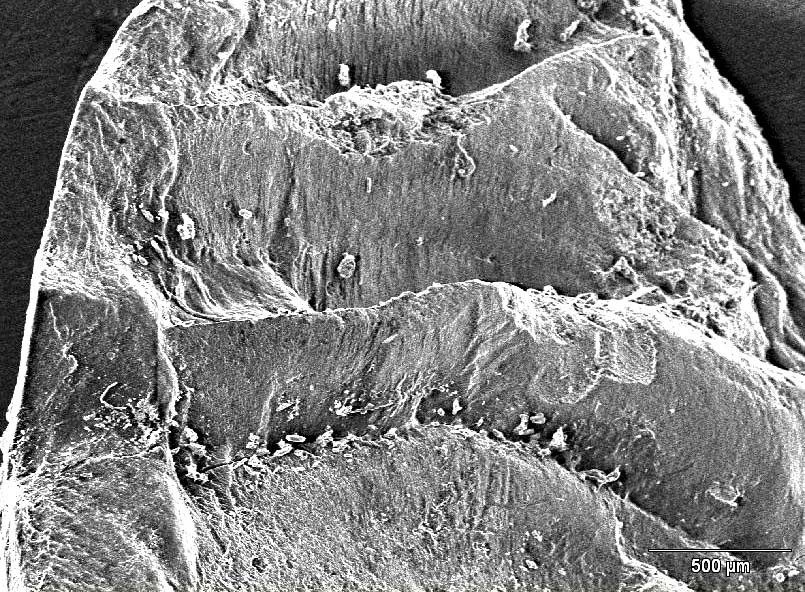
Resorption following infection may affect both the coronal and apical fragments. Additionally, involved root surfaces include the outer surfaces and it is not uncommon to for internal resorption to occur. Scanning electron microscopy (SEM) is an important technological aid for the analysis of the surface of the roots that are removed during endodontic surgery. Scanning electron microscopy enables the analysis of root morphology and the description of anatomy after resorption. The images presented in this review were captured with a SEM Hitachi Model S2460N (Hitachi, Tokyo, Japan) microscope with an acceleration voltage of 20 kV beam, and current of approx. 70 µA. The images present the SEM analysis of the surfaces of the fractured apical portion of #21 and the excised apical portion of #11. Interestingly, the area of the fracture of the apical fragment shows a geometric organization with vertical faults. As demonstrated earlier, fracture resistance is influenced by several factors, such as density, the diameter and the degree of obliteration depending on the patient’s age, presence of dentinal tubules and dentin microcomposition, which displays lower fracture resistance in deeper layers.28, 29
Figure 5 and Figure 6 show the root apexes of 2 excised fragments. On the root surface of tooth #21 (without root fracture), clear external resorption areas are visible even at lower magnification (×40); the same areas of resorption are less visible on the surface of tooth #11 at a higher magnification (×110). This indicates that the degree of external resorption was higher for #21 than #11.
The areas of resorption of tooth #11, that presented with the fracture of the third apical portion of the root, are more limited and shallower than those observed on the root surface of tooth #21, which has been completely avulsed, where the resorption was more aggressive and the lesions appeared to be diffuse, destroying the root surface (Figure 7, Figure 8).
Figure 9 and Figure 10 show the surface of the 2 removed apical fragments of tooth #21 and #11, respectively. Interestingly, the surface of the fracture that is visible on the apical root fragment removed during the apicoectomy of #11 is characterised by the presence of regular steps, reflecting a repetitive pattern.
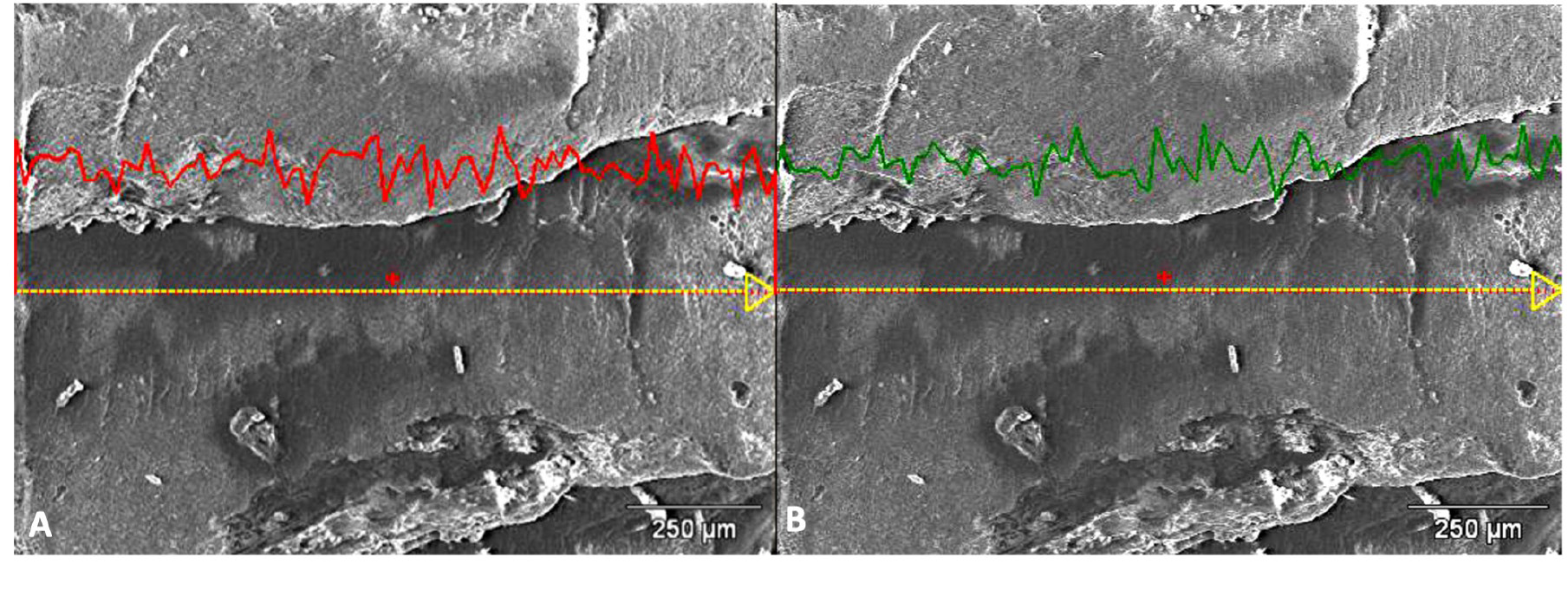
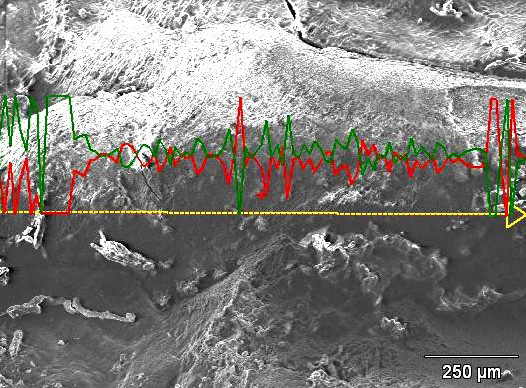
Micrographs are taken and energy dispersive spectroscopy (EDS) analysis is performed in the step regions in order to provide further information on fracture modality. Chemical analysis (microanalysis) with SEM can be performed by measuring the energy distribution and X-ray intensity generated by an electron beam on the sample using the EDS. This enables to identify and quantify the chemical elements in a given surface. The analysis indicates the percentage changes in the composition of phosphorus (P) and calcium (Ca) along the selected line, respectively, on the horizontal side (Figure 11) and on the vertical side (Figure 12) of one of the steps visible on the fracture surface. The point analysis, carried out at 7 measuring points selected along the tested lines, also confirms the stability of the P and Ca percentages. The analysis of microanalytical maps of the element distribution clearly emphasizes the heterogeneity in the transition areas between the horizontal and vertical parts.
Follow-up management
Follow-up should be performed at 4-week intervals while the teeth are splinted, and then at 3-month intervals for the first year. If no adverse clinical findings are evident, the annual visits should be arranged for the subsequent 5 years. Then, the tooth should be reassessed every 3–5 years. Follow-up visits are necessary to monitor pulp vitality, PDL cells vitality, periodontal status, and optimal oral hygiene maintenance through percussion, palpation, mobility tests, and periapical radiographs.30 Pulp vitality must be assessed at every follow-up visit using cold and electric tests.31
Periodontal ligament cells need to be monitored to ensure that they remain healthy. They are assessed with periapical radiographs, percussion, palpation, and mobility tests. Periodontal probing is recommended in all cases with coronal third root fractures and when an apicectomy has been performed.25 Patients must maintain excellent oral hygiene to avoid bacterial contamination of the root canal system.32
Figure 13 and Figure 14 show periapical radiographs at 6 months after the 1st (Figure 13) and 2nd apicoectomy (Figure 14A) and at 24 (Figure 14B) and 30 months (Figure 14C) after the trauma, with complete remission of clinical and radiographic symptoms.33
Discussion
The complexity of dental trauma results from several co-occurring elements that contribute to an increase in risk factors and a reduction in the long-term prognosis of the involved dental elements. The simultaneous presence of avulsion, apical third root fracture, non-compliance with the treatments according to the guidelines and, consequently, the early appearance of clinical signs of infection and inflammation define a complex clinical picture. Managing complex injuries requires a holistic approach that involves different dental professionals at different time points to guarantee the functionality and aesthetics of trauma areas.6, 34, 35, 36
This paper focused on the management of transverse root fractures in dental trauma. Epidemiology and classification of transverse root fractures, as well as the physiological responses to healing, emergency management and clinical protocols were presented. Injury management often involves clinical situations that are far from approved guidelines and protocols. Indeed, it may be necessary to treat a patient with dental trauma and a concomitant fracture outside the recommended and guideline-prescribed times and procedures..
Maintaining optimal oral hygiene is essential and should be checked at all follow-up visits. In the case of apicectomy or root fractures, the new root is shorter and the plaque must be constantly controlled. Plaque formation within the gingival sulcus is a long-term risk factor that can lead to the penetration of bacteria along the periodontium and infection of the root canal system. In order to avoid possible infections, it is extremely important to maintain optimal oral hygiene conditions in the first phase of healing and during the splinting period. This can be achieved through the topical application of concentrates of Camellia sinensis and ozonated olive oil, which are effective in controlling the clinical indexes of periodontal disease and gingivitis.37, 38, 39 The reduction of pain and maximum compliance with the necessary therapies can be achieved through the use of a holistic medicine approach, as recently demonstrated using photobiomodulation, kinesiology taping, and the use of lactoferrin to implement bone regeneration processes.40, 41, 42, 43
On the other hand, the irreversibility of infectious phenomena, such as inflammatory resorption, despite endodontic treatment undertaken even a long time after the injury, emphasizes the importance of obtaining sterility of the root canal system as soon as possible. Sterility is essential to avoid triggering progressive inflammatory resorption or ankylosis, and the lack of healing between the apical and coronal fragments in cases of root fractures.44, 45, 46, 47 The latter clinical scenario suggests a necessary modulation of therapeutic choices towards interventions to guarantee the durability of the teeth involved in the trauma within the oral cavity.
Conclusions
Teeth with transverse root fractures present a favorable long-term prognosis if the fracture is subcrestal and localized in the apical and middle third of the root. Providing the best conditions for healing, repositioning and stabilization of the fragment is very important. However, when a transverse root fracture is accompanied by other injuries, such as the avulsion of the coronal fragment, the degree of treatment difficulty increases and the long-term prognosis decreases. In different clinical scenarios, healing response was suboptimal and patients had pulp necrosis, delayed treatment due to a lack of compliance and infectious complications. Difficult cases can be managed with root canal treatment and recommendations exist for these surgical therapeutic solutions that allow for the longest maintenance of the teeth. The choice of the therapeutic solutions can impact future implant-prosthetic rehabilitation by preserving soft and hard tissues.
Ethics approval and consent to participate
Informed consent was obtained from both the caregivers and the patient.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.