Abstract
Background. Local anesthesia (LA) is commonly used for pain control in clinical dental practice. However, it is often perceived as the most painful part of the treatment and the factor leading to the avoidance of dental care. Hence, research on better means of pain management is being conducted.
Objectives. The aim of the study was to evaluate and compare pain perception using the No Pain III™ computer-controlled local anesthesia delivery (CCLAD) system and the conventional syringe, for inferior alveolar nerve block (IANB) in children.
Material and methods. Thirty children aged 6–12 years were included in the study. Children were randomly allocated into 2 groups by the flip of a coin. Group A received LA by conventional syringe and group B received LA by No Pain III™, on the contralateral side. Physiological parameters including blood pressure (BP), heart rate (HR) and respiratory rate (RR) were assessed at baseline, during the deposition and after the deposition of LA. A subjective evaluation of pain perception was assessed using the Wong–Baker FACES Pain Rating Scale (WBS). The measured values were subjected to statistical analysis.
Results. A statistically significant difference was observed between group A and group B for pain perception using the WBS, systolic BP and RR.
Conclusions. The use of the No Pain III™ CCLAD system resulted in reduced pain perception and better acceptance when compared to the use of the conventional syringe, for IANB in children.
Keywords: children, pain perception, inferior alveolar nerve block, computer-controlled local anesthetic delivery system, Wong–Baker FACES Pain Rating Scale
Introduction
The use of local anesthesia (LA) in dentistry has greatly reduced the pain and discomfort associated with various dental procedures in children. Local anesthesia is considered one of the best methods to perform intraoral operative and surgical procedures in children. However, delivery of LA and needle puncturing of the mucosa are uncomfortable. Local anesthesia is often perceived by children as the most painful part of treatment, and in some instances as the only painful part, which can lead to the avoidance of dental care.1 Pain can result from the mechanical trauma of needle introduction into the site of injection, or from the sudden distension of the tissues due to the rapid discharge of syringe contents. Pain can also be caused by the stimulation with the first few drops of the LA solution.2
Conventional syringes are commonly used in dentistry, as their utilization is cost-efficient and less technique-sensitive. However, while using a conventional syringe, the dentist must simultaneously control the movement of the penetrating needle and drug infusion variables. If they are unable to precisely control both activities, the injection technique will be compromised and this can lead to painful insertion or inadequate deposition.3 Several methods have been suggested to overcome conventional techniques of LA administration and to reduce pain caused by the administration of LA agents. Computer-controlled local anesthesia delivery (CCLAD) systems are one such method that has been introduced to reduce pain and anxiety of dental patients during LA delivery.1 The unit uses a microprocessor and an electronically controlled motor to deliver the anesthetic solution. Additionally, it uses a sterile disposable handpiece that does not look like a syringe, which greatly reduces fear and anxiety. Furthermore, this new system eliminates the manual pressure required by the operator to administer injections by generating a precisely controlled anesthetic flow rate. The combination of reduced distension of tissues and controlled flow rate results in a virtually imperceptible injection.4
To assess pain perception during dental anesthesia, various objective and subjective parameters have been used.5 Objective assessment can be performed by recording physiological parameters such as blood pressure (BP), heart rate (HR) and respiratory rate (RR) during the administration of LA. Subjective pain assessment can be done with the aid of non-verbal reporting, which has been used principally in clinical research to measure pain intensity.6
The present study was undertaken to evaluate and compare pain perception using the No Pain III™ CCLAD system and the conventional syringe, for inferior alveolar nerve block (IANB), a technique that is commonly carried out during treatment procedures in clinical pediatric dentistry. The null hypothesis was that there is no difference in pain perception between the No Pain III™ CCLAD system and the conventional syringe for IANB in children.
Material and methods
The present study was carried out in the Department of Pediatric and Preventive Dentistry of Terna Dental College, Navi Mumbai, India. Ethical clearance was obtained from the institutional Review Board of Ethics at Terna Dental College, Navi Mumbai, India (approval No. TDC/IRB-EC/95/2014).
Inclusion and exclusion criteria
The inclusion criteria for the study were children aged 6–12 years requiring LA by IANB on both sides of the mandibular arch for various dental procedures. Other criteria for inclusion in the study were a score of I according to the American Society of Anesthesiologists (ASA) Physical Status Classification System, no previous exposure to dental anesthesia and a Frankl behavior rating between 3 and 4. Exclusion criteria were children requiring unilateral IANB, patients with a Frankl behavior rating between 1 and 2, and those who were medically or mentally compromised.
Sample size calculation
The calculation of sample size was carried out using G*Power 3 analysis (v. 3.1.92; Heinrich Heine University Düsseldorf, Germany). The effect size was 0.5, the α error probability was 0.05 and power (1-β error probability) was 0.80. The calculated sample size included 30 children.
A total of 30 children aged 6–12 years who attended the outpatient department were selected for the study. Parents or guardians accompanying children were briefed about the procedure in the local language and written informed consent was obtained.
Study design
The study had a crossover design. The treatment under LA was carried out in 2 subsequent visits with a gap of 7 days. The sequence and LA administration method were randomly assigned to each child. The randomization was achieved by the flip of a coin to allocate the mode of the first local anesthetic delivery system (No Pain III™ CCLAD system or conventional syringe) to each subject. The children received LA by a single trained operator and on their subsequent visit they received the second local anesthetic delivery system (No Pain III™ CCLAD system or conventional syringe) on the contralateral side of the same arch (a crossover design).
The selected samples were divided into 2 groups. Group A underwent LA administration by conventional syringe and group B had LA administered using the No Pain III™ CCLAD system. Pre-anesthetic baseline monitoring of BP, HR and RR was performed using a Contec™ CMS6000 Patient Monitor (Contec Medical Systems Co. Ltd., Qinhuangdao, China).
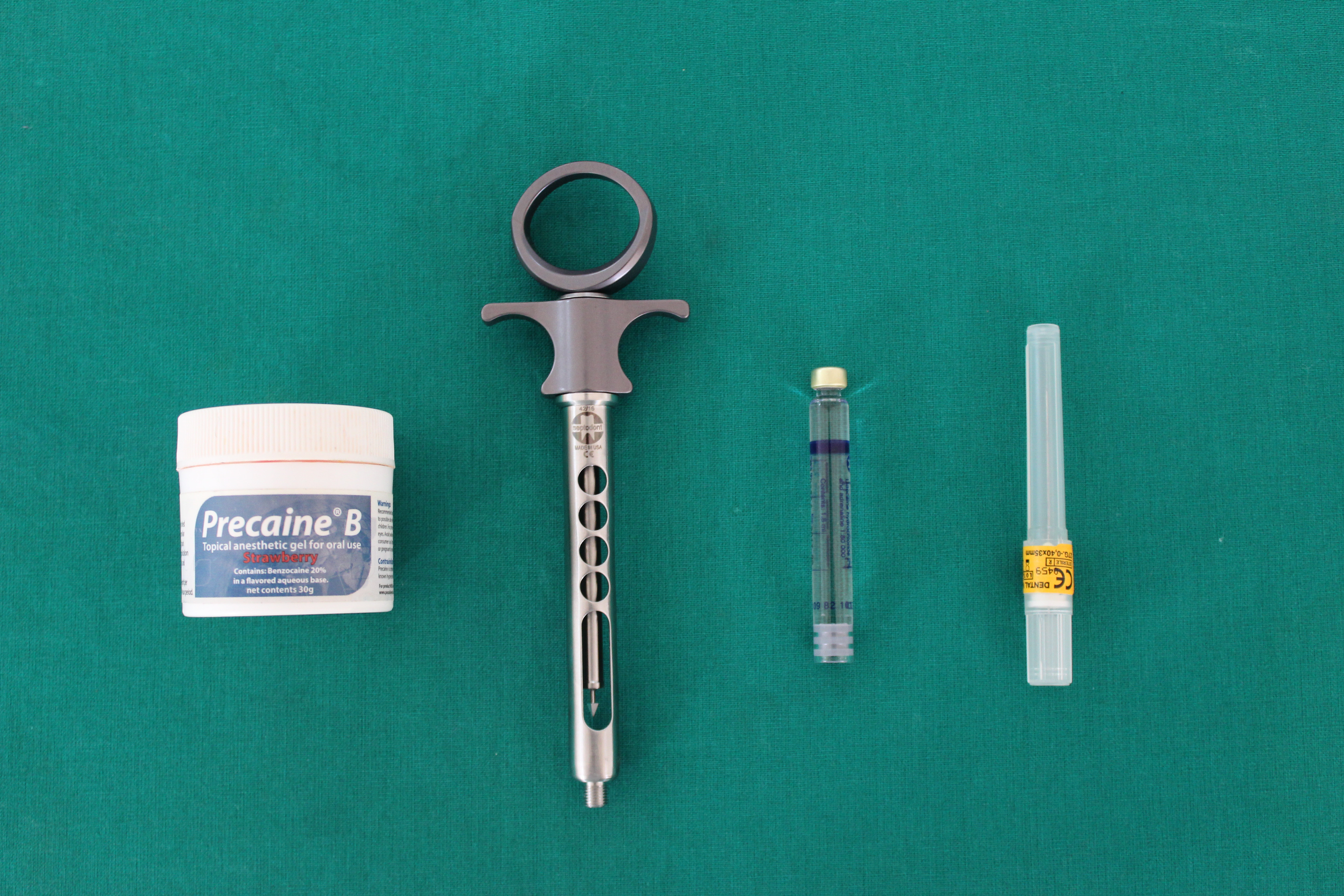
All procedures were performed by a single trained operator. Topical anesthetic gel Precaine® B (Pascal International, Bellevue, USA) was applied using a cotton pellet at the site of injection. After waiting for 1 min, IANB was performed. In group A, the conventional syringe (aspirating syringes; Septodont Healthcare Pvt. Ltd., Panvel, India)7, 8 was used with the LA solution in the form of cartridge (Lignospan Special consisting of 2% lidocaine with 1:80,000 epinephrine; Septodont Healthcare Pvt. Ltd.) and with a 27-gauge needle (0.27 mm × 35 mm, Septoject™; Septodont Healthcare Pvt. Ltd.) (Figure 1).
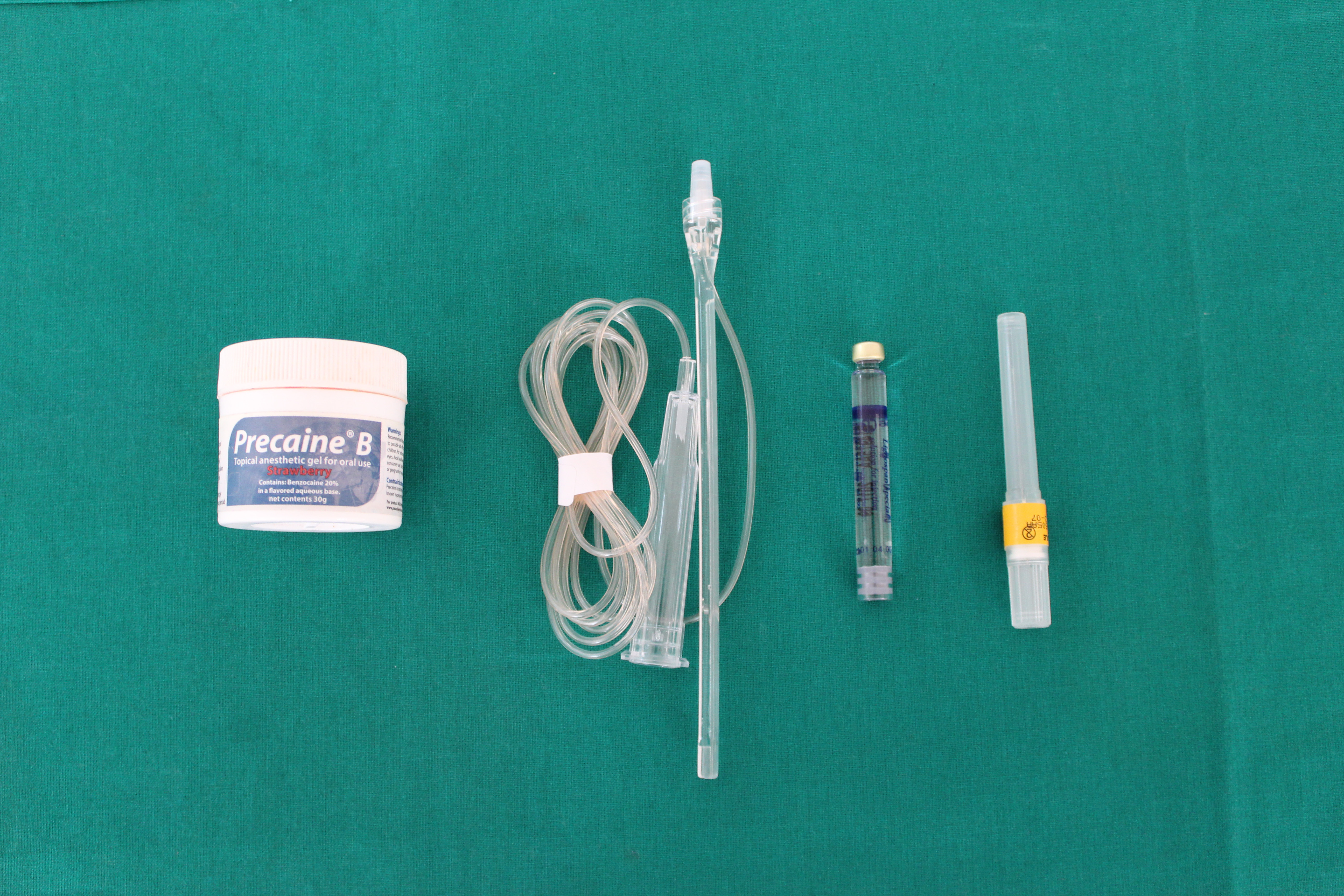
In group B, the No Pain III™ CCLAD system (KMG, Busan, Korea) was used for LA administration, which comprised of a disposable component, a handpiece component and a computer-controlled unit. The handpiece was an ultra-light pen-like handle that was linked to an anesthetic cartridge with plastic microtubing. The procedure was followed as per the manufacturer’s instructions (Figure 2, Figure 3). The delivery of a 1.8-mL single-use Lignospan anesthetic cartridge was done at slow speed, regulated by a pedal.
Blood pressure, HR and RR were recorded at baseline, during the deposition of LA and after the deposition. A subjective evaluation (self-report) of pain perception during the LA injection was assessed using the Wong–Baker FACES Pain Rating Scale (WBS). The scale consists of 6 different facial expressions numbered from 0 to 5 (no pain to intense pain). Patients were asked to select only 1 face to indicate the degree of pain they felt after the LA injection.
Statistical analysis
Obtained data was entered into a Microsoft Excel spreadsheet and subjected to statistical analysis using SPSS v. 17.0 software (SPSS Inc., Chicago, USA). A paired t-test was used to evaluate WBS scores between the 2 different groups, after the deposition of LA. Repeated measures analysis of variance (ANOVA) was used to compare vital parameters (BP, HR, RR) at baseline, during the deposition of LA and after the deposition, in both groups.
Results
The study population consisted of 30 children, 14 boys and 16 girls. Children were aged between 6 and 12 years, with a mean age of 9 ±1.8003 years. Because of the crossover study design, all 30 children were subjected to IANB using both the conventional syringe and the No Pain III™ CCLAD system.
Subjective evaluation of pain perception using the Wong–Baker FACES Pain Rating Scale
In the evaluation of children’s pain perception using the WBS Scale, group B showed lower pain scores compared to group A. The difference was statistically significant (p < 0.05) (Table 1).
Assessment of physiological parameters
Table 2, Table 3, Table 4 show intergroup comparisons of physiological parameters, including BP, HR and RR at baseline, during the deposition of LA and after the deposition.
Blood pressure
Comparison of BP values indicated that group A had increased systolic BP during the deposition of LA when compared to group B. The difference was statistically significant (p < 0.05) (Table 2). However, the difference in diastolic BP was not statistically significant.
Heart rate
Comparison of the mean HR values between group A and group B is shown in Table 3. No significant differences in HR were observed between both groups at various time intervals.
Respiratory rate
Comparison of RR between both groups indicated that RR increased during and after the deposition of LA in group A when compared to group B. The difference was statistically significant (p ≤ 0.05) (Table 4).
Discussion
Pain is an unpleasant sensation that is often associated with actual or potential trauma or tissue injury.9 Kaufman et al.10 reported that the injection of the area in the oral cavity was directly related to pain and perceived discomfort. Palatal and IANB injections are more painful than local infiltration, mental nerve block or periodontal ligament injection.8 However, IANB is the most frequently used injection technique for achieving LA during mandibular restoration and surgical procedures. Therefore, the IANB technique was used to compare pain perception between the No Pain III™ CCLAD system and the conventional syringe.
No attempt was made to match the CCLAD and conventional groups by gender, since previous studies in children comparing CCLAD and conventional syringes have shown no difference in pain sensation between males and females.11
In the studies by Tahmassebi et al.11 and Gibson et al.12 each child was assigned to either the CCLAD or the conventional syringe group. The authors reported that the use of the CCLAD system resulted in significantly less disruptive behavior when compared to the conventional syringe.
In the current study, the children served as their own control, wherein at the first appointment one LA administration method was used, and the other method was performed on the subsequent visit. This study is in agreement with those of San Martin-Lopez et al.13 and Langthasa et al.14
Pain perception was evaluated after the deposition of LA using the WBS.15 When the 2 methods were compared using this scale, statistically significant differences were observed between group A and group B, indicating better patient acceptability towards CCLAD (No Pain III™). Since there was a difference in the mean values between both groups, the null hypothesis was rejected. These results are in accordance with studies conducted by Langthasa et al.14 and Goyal et al.16 In contrast, studies conducted by Asarch et al.17 and Koyutürk et al.18 found no difference in the pain rating between the CCLAD and the conventional syringe.
Assessment of physiological parameters
Blood pressure
Akinmoladun et al.19 and Meyer20 hypothesized that increased HR and alterations in BP during dental procedures are due to endogenous catecholamine release resulting from emotional stress, and are not a pharmacological effect. Meanwhile, Tolas et al.21 and Meechan et al.22 considered cardiovascular responses to dental treatment under LA to be influenced more by the anesthetics. In addition, pain may cause BP to rise due to the release of endogenous catecholamine.23
Heart rate
Changes in HR are expected to reflect patient responsiveness to procedures, especially during stressful experiences. According to Dowling,24 HR increases in response to the application of pain. It has been suggested that mean HR increase during the deposition of LA is due to the fact that an alarm reaction is initiated by the hypothalamus. This results in vasodilatation and causes an increase in the release of endogenous epinephrine and norepinephrine that subsequently increases HR and cardiac output.25 The above findings were in accordance with the study conducted by West et al.26
The results of the present study indicate that mean HR was higher during the deposition of LA by both conventional syringe and No Pain III™. In contrast to our findings, studies conducted by San Martin-Lopez et al.13 and Bansal et al.2 showed lower HR using a computer-controlled delivery system compared to conventional methods. These differences may be due to the pen-like design of the studies, which was virtually pain-free, more predictable and less threatening to the patients.
Respiratory rate
In agreement with the results of the present study, Nicholson et al.27 and Langthasa et al.14 concluded that the CCLAD system was more acceptable and less anxiety-inducing compared to the conventional method. According to Pashley et al.,28 painful sensation during any needle injection comes from administering an anesthetic solution too rapidly or with too much force. They also stated that with a conventional syringe, the volume flow and pressure parameters cannot be precisely controlled, which results in difficult, erratic and uncomfortable injections. According to Nusstein et al.,29 CCLAD maintains a constant positive pressure on the flow of anesthetic solution, thereby yielding a virtually pain-free needle insertion. Furthermore, the improved tactile feedback, visibility and automated aspiration achieved with CCLAD allow for concentration on needle positioning and patient interaction.2
Studies have been conducted using other types of computer-assisted anesthesia. The study conducted by Berrendero et al.7 compared the Calaject CCLAD system with the conventional anesthesia. This study concluded that the majority of children reported significantly less pain with the CCLAD system.
One of the important reasons for preference towards CCLAD is that it lowers the pain of injection as well eliminates the visual stimulus of dental syringes. The expense of buying new syringes and disposable attachments, the length of injection time, the need to change work routines, and the additional space needed for the device, remain limiting factors for its widespread introduction into clinical practice.30
Limitations
A larger sample size should have been selected to observe changes in pain perception. Also, the difference in duration of LA deposition could have been considered. Furthermore, the objective assessment of pain perception in children using physiological parameters could have been analyzed using different types of CCLAD systems.
Conclusions
From the present study, it can be concluded that pain perception in children was reduced while using the NoPain III™ CCLAD system when compared to the conventional syringe for IANB anesthesia.
Ethics approval and consent to participate
Ethical clearance was obtained from the institutional Review Board of Ethics at Terna Dental College, Navi Mumbai, India (approval No. TDC/IRB-EC/95/2014). Written informed consent was obtained from all participants.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.