Abstract
Background. Awake bruxism (AB), characterized by repetitive jaw muscle activity during wakefulness, is often associated with stress, anxiety and depression.
Objectives. The aim of the study was to examine the long-term relationships between psychological distress, resilience and AB behaviors during stressful periods. To this end, a longitudinal, within-subject design of the study was used.
Material and methods. A repeated-measures design was employed to evaluate 136 individuals. The participants underwent 2 assessments: the baseline evaluation conducted at the onset of an armed conflict (phase 1); and the follow-up evaluation, performed 1 year later, when the conflict remained ongoing (phase 2). Each subject served as their own control. At each phase of the study, the participants completed a self-report questionnaire, the Oral Behavior Checklist (OBC), which addressed self-awareness of performance of teeth grinding, teeth clenching, tooth contact, and/or mandible bracing while awake. A score of 2 and above on any of the questions indicated positive awareness of the presence of AB behaviors. The additional questionnaires referred to subjects’ ability to cope with stress adaptively, their ability to recover from stress, perceived stress, screening for depressive and anxiety symptoms, and screening for adjustment disorder and post-traumatic stress disorder (PTSD).
Results. A significant increase in teeth clenching was apparent during phase 2. The subjects’ ability to cope with stress in an adaptive manner, as well as their perceived stress levels, increased the likelihood of AB behaviors during both phases (odds ratios ranging from 11% to 27%).
Conclusions. Awake bruxism behaviors in general, and teeth clenching in particular, should be considered as possible stress-relieving behaviors.
Keywords: coping, resilience, psychological distress, awake bruxism, AB
Introduction
Awake bruxism (AB) is defined as repetitive jaw muscle activity during wakefulness, characterized by continuous or recurrent tooth contact and/or bracing or thrusting of the mandible.1 Studies on AB have transitioned from perceiving bruxism as merely a pathological condition to recognizing it as physiological masticatory muscle activity. Bruxism has the potential to act as a risk factor for certain medical conditions, but it can also serve as a protective factor.2, 3 A recent update to the 2018 consensus on bruxism assessment provided a glossary of all constituent terms used in the definitions of unspecified, sleep and awake bruxism that have been published previously.4 With a global prevalence of 16–32%, AB represents a significant concern for healthcare professionals.5 Tooth contact is considered to be the most prevalent AB behavior.6, 7
Awake bruxism is influenced by psychological, biological and genetic factors.8, 9 Psychological factors associated with AB include personality traits, such as neuroticism and somatization,10 anxiety, depression,11 and stress sensitivity.12 Widespread stress can be attributed to various sources, including the coronavirus disease 2019 (COVID-19) pandemic, natural disasters and war. During the pandemic, there was a notable increase in the prevalence of bruxism and temporomandibular symptoms. The impact of the pandemic on temporomandibular disorders (TMD) and AB was more extensive than initially expected.13, 14
The physiological response to stress is primarily mediated by the hypothalamic–pituitary–adrenal (HPA) axis, which serves as the body’s central stress response system. Chronic stress can lead to the dysregulation of the HPA axis, characterized by prolonged activation of the HPA axis, which in turn disrupts cortisol regulation, leading to a decline in both physical and mental health.15 The neural substrates underlying chronic stress responses may differ markedly from those involved in acute stress reactions, often engaging distinct limbic, hypothalamic and brainstem circuits. An individual’s response to stress, whether acute or chronic, is shaped by a constellation of factors, including genetic predisposition, early life experiences, environmental influences, biological sex, and age. The contextual framework within which stressors are encountered plays an important role in determining whether the resultant stress responses are adaptive or maladaptive.16 A meta-analysis performed by Chemelo et al. revealed a significant association between stress and bruxism.17 However, the authors emphasized that the quality and reliability of the evidence are low, and signaled the necessity for additional studies to understand this relationship more comprehensively.17
Recent research suggests that AB may play a positive role in stress coping. This finding is compatible with the hypothesis of mastication as a means of relieving psychological tension,10 which indicates that bruxism might serve as an adaptive mechanism for managing stress, rather than simply being a pathological consequence.
War, one of the most intense stressors, significantly affects mental health by inducing severe stress and anxiety, even among individuals not directly involved in combat. Since the terrorist attack on Israel on October 7, 2023, the notion that the nation was experiencing national trauma was suggested. This trauma was believed to cause long-lasting implications for the future.18
Initial results indicated that within the first 3 months of the armed conflict, 68% of the participants were identified as having adjustment disorder, a maladaptive response to stressors that typically occurs within 3–6 months of the stressful stimulus.19 Subjects with adjustment disorder exhibited less muscle relaxation and more teeth clenching and grinding than those without the disorder. The armed conflict has been continuing for over a year, leading to an increased incidence of more severe stress-related conditions, such as post-traumatic stress disorder (PTSD). Several studies have documented the escalating prevalence of PTSD among the Israeli civilian population following October 7, 2023.20, 21, 22
To date, there is a limited understanding regarding how the same individuals respond to prolonged stress regarding AB.17 Such understanding can be achieved through longitudinal studies examining AB under prolonged stress conditions. The ongoing conflict in Israel creates conditions for studying the impact of prolonged, population-wide stress on AB behavior. A previous study compared 2 different groups of subjects during different periods of time (one group was examined during peaceful time and the other during the beginning of the armed conflict).19 The present study adopts a different approach and attempts to evaluate the same group of subjects twice (a within-subject design), during the armed conflict. Specifically, the objective was to longitudinally monitor subjects’ AB behavior from the initial months of the armed conflict through a one-year period, during which the conflict remained active. Additionally, the aim of this study was to examine the long-term relationships between psychological distress, resilience and AB behavior.
The hypothesis of the study posits that there will be an increase in AB behaviors between phase 1 and phase 2. This increase will be mediated by stress, anxiety, depression, and resilience.
Material and methods
Population
To investigate intraindividual change, the study utilized a repeated-measures design, evaluating the same cohort of participants at 2 distinct time points across a 12-month interval. The study population comprised a convenience sample of dental students aged >18 years from the Maurice and Gabriela Goldschleger School of Dental Medicine at Tel Aviv University, Israel, the largest academic institution in the country. The university’s student body includes individuals from diverse ethnic, cultural and social backgrounds, including Jewish, Muslim, Christian, secular, and Orthodox groups.
The data collection was conducted independently by 3 dental students (AYC, NV, MZ) to minimize researcher bias. Participants were approached twice during 2 different time periods (phase 1 and phase 2). Each subject served as their own control. No financial compensation was provided for participation. The exclusion criteria were diagnosed neuromuscular and/or joint diseases, confirmed depression, and trauma to the head or jaw during the past 6 months.
The study received ethical approval from Tel Aviv University (approval No. 0009558-2). Written informed consent was obtained from all participants.
Phase 1
The data was collected in January 2024. This period has been marked by significant stress, extending over a duration of 3 months following the terrorist attack that occurred on October 7, 2023, and persisting throughout the subsequent armed conflict and massive missile attacks on the Tel Aviv area.
Phase 2
Participants who were assessed in phase 1 were reapproached 1 year later, in January 2025. The ongoing armed conflict and the continuous missile attacks on civilian population centers (occurring both during daytime and night) led to prolonged exposure to stress, which resulted in high levels of uncertainty, insecurity and instability.
Tools
The following questionnaires in Hebrew were administered to the participants via Google Forms links:
– self-report regarding the performance of 4 AB behaviors (teeth grinding, teeth clenching, tooth contact, and/or mandible bracing) while awake, based on the last month.23, 24, 25, 26 The questions were part of the Oral Behavior Checklist (OBC). The validity of the OBC was proven in several studies.27, 28 The version used in the present study is part of the official Hebrew version of the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) Axis II.29, 30 The response scores range from 0 (none of the time) to 4 (all of the time). A score of 2 and above on any of the questions indicated positive awareness of the presence of AB behaviors;
– Brief Resilience Coping Scale (BRCS), which is a component of the Standardized Tool for the Assessment of Bruxism (STAB).31 The BRCS evaluates an individual’s ability to cope with stress adaptively, emphasizing their capacity to use coping strategies with flexibility and persistence to tackle problems, even when faced with stressful situations. The participants were asked to rate how well specific statements described their behaviors or actions using a scale from 1 (does not describe me at all) to 5 (describes me very well). The BRCS is unidimensional, representing 1 latent factor.32 The total score, ranging from 4 to 20, can be categorized into low (4–13), medium (14–16) and high (17–20) resilience coping33;
– Brief Resilience Scale (BRS), which evaluates the ability to recover from stress. It comprises 6 statements, rated on a scale from 1 (strongly disagree) to 5 (strongly agree). The total score ranges from 6 to 30, and when divided by 6, can be categorized as low resilience (≤2.9) or normal/high resilience (≥3.0)34;
– Patient Health Questionnaire-4 (PHQ-4), which is part of the official Hebrew version of the DC/TMD Axis II.20 The PHQ-4 is a reliable and valid tool for screening depressive and anxiety symptoms in both clinical and non-clinical populations.35 The total score ranges from 0 to 12, and is typically assessed using the following cut-off scores: normal (0–2); mild distress (3–5); moderate distress (6–8); and severe distress (9–12);
– Perceived Stress Scale-10 (PSS-10), which is used worldwide, and the validity and reliability of which have been proven in numerous studies.36 An official Hebrew version of the questionnaire was used.37 The questionnaire measures the frequency of stress experienced over the past month through 10 items, with responses ranging from 0 (never) to 4 (very often). The total score ranges from 0 to 40 and can be categorized as low stress (0–13), moderate stress (14–26) and high stress (27–40)38;
– ultra-brief version of the Adjustment Disorder New Module (ADNM-4), which serves as a brief screening tool to assess symptoms of adjustment disorder.39 The participants were asked to indicate the frequency of items on a 4-point Likert scale, ranging from “never” to “often”. A score of 8.5 or higher is recommended for the diagnosis of subjects with adjustment disorder40;
– Primary Care PTSD Screen for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (PC-PTSD-S), is a validated screening tool designed to identify individuals in primary care who may have probable PTSD. It was collected during phase 2 only, and it aligns with the diagnostic criteria from the DSM-5. The PC-PTSD-5 is a 5-item screening tool designed to identify individuals with probable PTSD.41 The responses are scored on a scale from 0 to 5. A cut-off point of 4 ideally balanced false negatives and false positives for the overall sample and for men. However, for women, a cut-off point of 4 resulted in a high number of false negatives. In some cases, a lower cut-off point is considered, as performance parameters may vary depending on the sample.42
Statistical analysis
The sample size calculation, based on a medium effect size of d = 0.5, a statistical power of 80%, a two-tailed significance level of α = 0.05, and an assumed correlation between measurements of 0.5, required the collection of responses in both examination periods from a minimum of 27 participants.
Multiple Wilcoxon signed-rank tests were used to compare psychological and behavioral variables between phases. Logistic regression analyses were performed to determine which psychological self-report measures showed the ability to predict subjects’ awareness of AB behaviors at each of the time phases.
To assess the robustness of the findings, a series of sensitivity analyses were performed. First, the behavioral and psychological outcome variables were re-evaluated using paired t-tests alongside the primary Wilcoxon signed-rank test to verify the consistency of results under parametric assumptions. Second, to guard against false discovery, the Benjamini–Hochberg correction, at a false discovery rate (FDR) of 0.05, was applied. Third, the internal consistency of psychological scales was verified using Cronbach’s alpha. Finally, the estimation of the robust effect size was calculated using Cohen’s d.
The statistical analyses were performed using the IBM SPSS Statistics for Windows software, v. 29 (IBM Corp., Armonk, USA) and Jamovi v. 2.6 (https://www.jamovi.org/download.html).
Results
Population
During the 1st phase, 150 students completed the self-report questionnaires. Of the initial group, 136 subjects consented to participate in the follow-up evaluation during the 2nd phase (91% response rate, 62.5% female, mean age: 28.4 ±3.7 years). The data indicates that 46% of the subjects were single, while the remaining subjects were either married or living with a spouse. The mean number of children per participant was 0.3, with the mean age of the youngest child being 2.16 ±2.15 years. The reasons for not participating in the 2nd phase were absence at the time of data collection (sick leave, military service recruitment, etc.) and/or reluctance to participate due to lack of interest.
Oral behaviors
A large majority of the participants demonstrated awareness of AB behaviors in both phases (67.6% and 75.7%, respectively). The difference between the phases did show statistical significance.
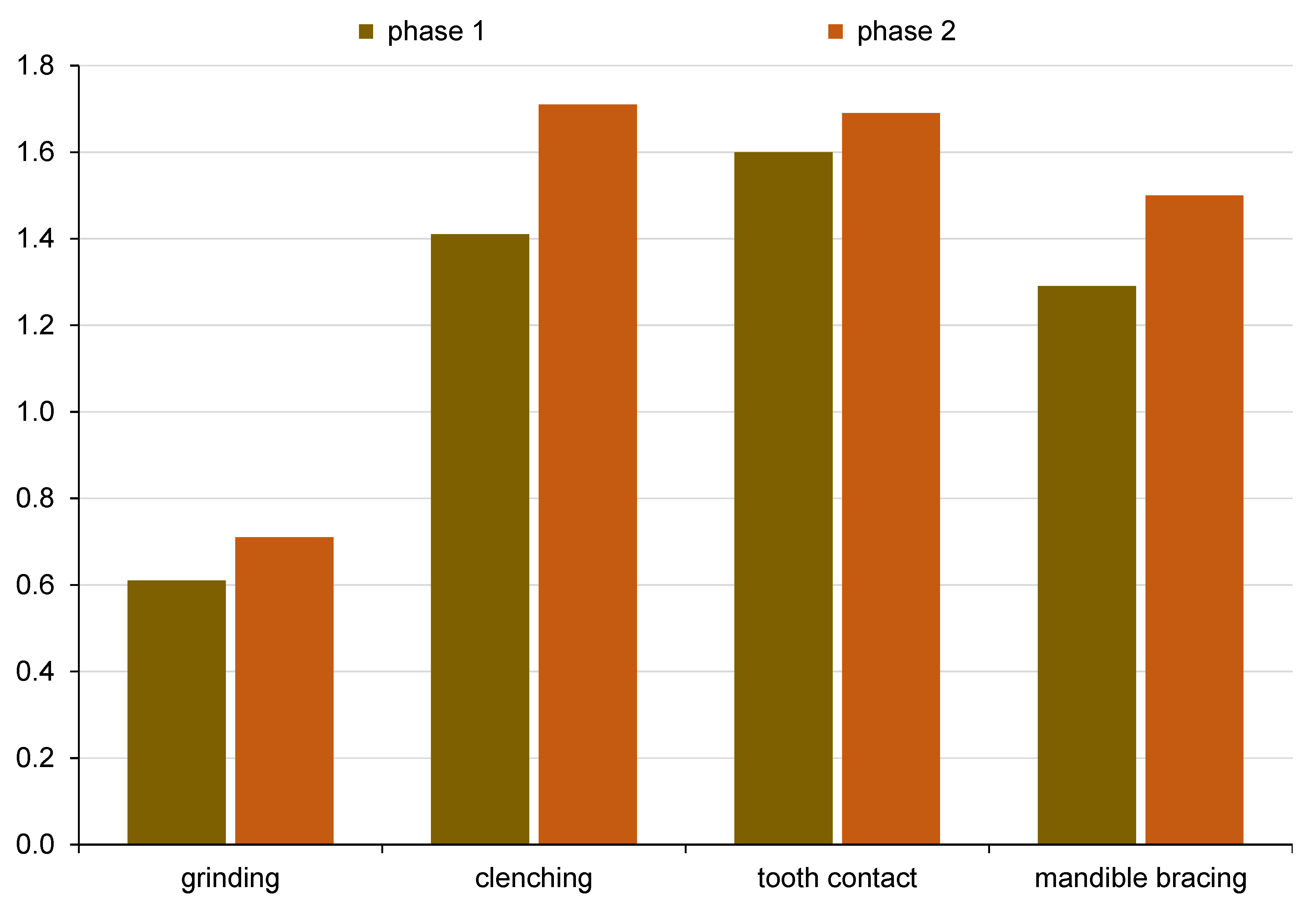
To examine changes in different AB behaviors from the 1st to the 2nd phase, the Wilcoxon signed-rank test was performed. The analysis revealed no missing values in either variable. Initial analyses indicated a statistically significant increase in clenching behavior (Z = −2.361, p = 0.018), with no significant changes in grinding (p = 0.372), tooth contact (p = 0.424) or mandible bracing (p = 0.107). Following the Benjamini–Hochberg correction, only clenching remained significant (Table 1, Figure 1). The paired t-tests largely confirmed the findings from the Wilcoxon test, thereby increasing confidence in the results.
Self-report psychological measures
The reliability of self-report psychological measures (Chronbach’s alpha) was as follows (phase 1 and 2, respectively): PHQ-4 – 0.85, 0.87; ADNM-4 – 0.82, 0.81; BRCS – 0.70, 0.66; BRS – 0.73, 0.77; PSS-10 – 0.89, 0.91; PC-PTSD-S (2nd phase only) – 0.67.
In general, subjects in both phases reported moderate stress levels (PSS-10), presented mild distress levels (PHQ-4), demonstrated medium ability to cope with stress adaptively (BRCS), and displayed normal or high ability to recover from stress (BRS).
To evaluate the differences between the 1st and 2nd phases across the 5 psychosocial measures, the Wilcoxon signed-rank test was used. The analysis revealed no missing values in either variable. The raw p-values indicated a significant change for ADNM-4 (p < 0.001), BRCS (p = 0.047) and PSS-10 (p = 0.003), while other measures did not reach the level of statistical significance (all p > 0.05). Following the Benjamini–Hochberg correction, only ADNM-4 and PSS-10 retained statistical significance (Table 2). The paired t-tests largely confirmed the findings of the Wilcoxon test, thereby increasing confidence in the results.
The study revealed no significant differences in AB behaviors between participants with high scores (≥4) on the PC-PTSD-S (78.6% reporting AB behaviors) and those who attained scores below 4 (75.4% reporting AB behaviors), with only a 3.2 percentage point difference (2nd phase). The results remained similar when a cut-off point of 3 was applied (78.4% vs. 75.4%, respectively).
Multivariate logistic regression
To determine which psychological self-report measures could predict participants’ awareness of AB behaviors, logistic regression analyses were conducted for each phase. Initially, each variable was evaluated through a series of binomial logistic regression models. The variables that demonstrated significant predictive ability were incorporated into the multiple logistic regression models (Table 3).
In both the 1st and 2nd phases, an increase in BRCS was associated with a higher probability of AB behaviors (rise by 26% and 27%, respectively). An increase in PSS-10 led to an 11% and a 16% rise, respectively, in the odds of AB behaviors.
In the 1st phase, the model explained 14% of the variance in the dependent variable (Nagelkerke’s R² = 0.14). In the 2nd phase, the model explained 21% of the variance in the dependent variable (Nagelkerke’s R² = 0.21).
Discussion
Bruxism remains a considerable diagnostic and therapeutic challenge due to its complexity and incomplete understanding of its pathophysiology. This persistent uncertainty underscores the necessity for the continuous exploration of novel therapeutic strategies.43 For example, a study that examined the effect of TMD treatment on self-reported sleep bruxism (SB) and AB found that subjects who received a combination of counseling and other treatments exhibited an increase in the frequency of AB bracing, potentially attributable to increased awareness of the condition.44
The present study employed a longitudinal design in a real-life stress context, namely an armed conflict. Although the associations between stress and AB have been demonstrated previously, longitudinal follow-up of subjects over a period of time enables the observation of how variables change within individuals under stressful conditions. Given that the study participants are the same individuals, any differences between subjects are minimized. This methodological approach enables the focus on temporal changes. Longitudinal follow-up studies on AB are scarce, although some recent research has attempted to address this issue.45
The current study examines a gap in our understanding of AB behaviors, namely how individual AB patterns and associated psychological aspects change when exposed to prolonged stress. The study examines a real-world scenario of shared, prolonged stress exposure among all participants.
The second phase of the study revealed that teeth clenching was the only behavior to exhibit a statistically significant increase. Of the 4 studied AB behaviors (tooth contact, mandible bracing, teeth clenching, and teeth grinding), only 2 present repeated masticatory muscle activity and forceful tooth contact (teeth clenching and teeth grinding). Unlike teeth grinding, which is rarely reported during waking hours (frequency ranging from 0.1% to 1.0%, based on the designated Ecological Momentary Assessment (EMA) approach), teeth clenching is markedly more frequent (frequency ranging between 2.0% and 11.2%).46 Physiologically, teeth clenching activates a neural pathway within the sympathetic adrenomedullary axis, which leads to the release of norepinephrine. Norepinephrine plays a crucial role in physiological stress responses, potentially counteracting the activation of the HPA axis.12 Under conditions of sustained stress, teeth clenching may constitute a protective behavioral adaptation that assists in the regulation of stress response.
Despite the extended conflict and ongoing physical threats to the population, the participants reported only moderate perceived stress levels (PSS-10), which further decreased during the second evaluation phase. During periods of prolonged stress, individuals may become psychologically habituated to stressors, yet their physiological response systems may remain sensitized, maintaining the relationship between bruxism and stress.47 The moderate perception of stress and mild distress levels in the present study may be a result of the subjects’ ability to recover from stress (normal to high scores, as measured by the BRS). Israeli society, constantly exposed to security tensions and alerts, appears to be relatively resilient and demonstrates high stress recovery capabilities.48
The decrease in the prevalence of adjustment disorder during the second phase is not unexpected. The disorder involves a maladaptive response to stressors that typically occur within 3 months and resolve within 6 months. The data for the first phase was collected 3 months after October 7, 2023, during extremely stressful events, while the data for the second phase was collected a year later, when adjustment disorder might have been either resolved or transformed into more severe PTSD.
Post-traumatic stress disorder is a mental health condition triggered by the exposure to a traumatic event, such as war. Subjects diagnosed with PTSD have a higher prevalence of TMD diagnoses compared to controls.49, 50, 51 Several studies have noted an increasing occurrence of PTSD among the Israeli civilian population following October 7, 2023.21, 22 In the present study, subjects who scored highly on the PC-PTSD-S (cut-off points of ≥3 or ≥4), as well as subjects with scores below the cut-off point, reported a high prevalence of AB behavior (>75%). This observation referred to the 4 studied behaviors (teeth grinding, teeth clenching, tooth contact, and/or mandible bracing). In the present study, reports were collected within 15 months of the ongoing conflict, a timeframe that may account for the elevated prevalence of AB behaviors. This may partially explain the lack of significant differences between PTSD-positive and PTSD-negative groups. Another possibility is that AB behaviors and PTSD may constitute distinct and independent responses to stress, rather than being causally linked.
The management of stress is highly influenced by individual coping strategies. Saczuk et al. showed that subjects with SB use maladaptive coping strategies more frequently than subjects without SB.52 Soto-Goñi et al. demonstrated that awake bruxers display more adaptive coping strategies than subjects who do not manifest bruxism symptoms.10 Although the BRS and BRCS are conceptually linked in measuring aspects of resilience, these instruments assess distinct phases within the adaptive response to stress. The inclusion of both scales enables the examination of whether recovery capacity and adaptive coping processes exhibit differential relationships with AB behaviors, thereby providing a more nuanced understanding of resilience mechanisms. The BRCS has been developed to assess individuals’ propensity to adopt adaptive coping strategies in response to stress.33 This scale evaluates individuals’ ability to adapt to and manage challenging situations, in contrast to the BRS, which focuses on resilience as the capacity to recover from stress.34 The overlap between the two reflects the complex and multifaceted nature of resilience.
The findings of the present study suggest that both perceived stress and resilient coping are associated with subjects’ AB behaviors. Perceived stress has been identified as a significant contributing factor to the occurrence of AB and its clinical manifestations.53 Popescu et al. demonstrated a meaningful correlation between stress and AB, recommending that stress be incorporated as an essential factor in the evaluation of bruxism.54 These results are consistent with our findings and support including stress-related measures in the STAB tool.
While the capacity for stress recovery, as measured by the BRS, demonstrated clear effects, the influence of resilient coping strategies (BRCS) and the manifestation of depressive and anxiety symptoms (PHQ-4) appeared comparatively less pronounced. As previously indicated, AB behaviors in general, and teeth clenching in particular, may play a positive role in stress coping. Specifically, mastication serves as a means of managing psychological tension.10 In a literature review, Kubo et al. claimed that chewing is a useful stress coping mechanism, because it alters the functions of the HPA axis and the autonomic nervous system.55 Furthermore, it can minimize stress-induced changes in the hippocampus and hypothalamus.55 Maciejewska-Szaniec et al. demonstrated that sequence variants in genes related to stress coping may be correlated with AB susceptibility via an elevated perceived stress level.53 A recent review suggested that stress, as an initiating factor, increases muscle tone, and when this increase rises to 10–20%, it may cause a bruxism event, in addition to reducing the pain threshold.12
The present findings indicate that both perceived stress and resilience coping increase the likelihood of AB behaviors. The finding that subjects’ tendencies to cope with stress in a highly adaptive manner (BRCS) increase the odds of AB seems paradoxical, as it suggests that AB behaviors may be part of the body’s stress regulatory system, possibly providing proprioceptive feedback that contributes to the modulation of stress responses.55 Awake bruxism behaviors serve as a form of adaptive, albeit unconscious, behavior that may help individuals maintain functionality during stressful periods and/or may act as a compensatory mechanism for inadequate psychological coping resources, acting as a physical outlet when cognitive coping strategies are insufficient.56 Alternatively, subjects under stress may be more conscious of their AB behaviors, which could result in over-reporting.
Unfortunately, numerous parts of the world are afflicted by armed conflicts (e.g., Ukraine, Colombia, Africa). The impact of prolonged stress caused by wars on AB behaviors may affect the lives of millions. Individuals diagnosed with bruxism exhibit a high prevalence of TMD, with global co-occurrence rates estimated at approximately 17%, though these figures vary across different regions.57 Recently proposed shortened screening tools for TMD and bruxism enable a better assessment of these conditions by general dentists.58 Enhanced awareness of AB behaviors, alongside the implementation of lifestyle-based therapeutic interventions such as modifications to daily routines, sleep hygiene and dietary habits, may offer general benefits,43 particularly for individuals exposed to sustained stress.
Limitations
The sample of our study consisted of dental students from a single academic institution. Even though the student body in the Dental School is quite diverse, including individuals from different ethnic, cultural and social backgrounds, the highly specific cohort may limit the generalizability of the findings. Regrettably, no information was collected regarding factors such as smoking and/or sleep quality. Moreover, AB behaviors were assessed through single-point self-report and not as a combination of single-point self-report with the EMA approach, as recommended by the recently introduced STAB.31 While the single-point self-report method represents a valid and accessible means for evaluating bruxism behaviors, the EMA approach offers a more detailed real-time report on AB behaviors.59 The self-report assessment of AB may be subject to recall and over-reporting bias. The longitudinal follow-up design, in which each subject serves as his or her own reference for comparison, presents some advantages, but further longitudinal studies using more accurate tools to define AB (e.g., electromyography) are necessary to explore these issues more thoroughly.
Clinical importance
Personal stress management techniques serve as essential coping mechanisms when facing prolonged adversity. Awake bruxism behaviors in general, and teeth clenching in particular, may play a positive role in stress coping and serve as a means of managing psychological tension.10 As teeth clenching involves forceful occlusal forces, it may lead to adverse results such as abfractions and tooth fractures.1, 60 Accordingly, subjects who engage in such stress coping behaviors should be provided with preventive interventions and subjected to ongoing clinical monitoring to mitigate long-term health consequences.61
Conclusions
Perceived stress and an individual’s capacity to use coping strategies with flexibility and persistence in addressing problems during stressful situations increase the likelihood of exhibiting AB behaviors over extended periods. The results suggest that AB behaviors in general, and teeth clenching in particular, may play a role in stress coping.
Ethics approval and consent to participate
The study received ethical approval from Tel Aviv University in Israel (approval No. 0009558-2). Written informed consent was obtained from all participants.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.