Abstract
Cholelithiasis is one of the most common gastrointestinal diseases, which often manifests asymptomatically. Statistically, up to 20% of the global population is affected by gallbladder diseases. The prevalence of these conditions rapidly increases with the patient’s age. Obstructive sleep apnea (OSA) is a sleep-related breathing disorder that causes pharyngeal airway collapse, hypopnea and snoring. It is estimated that nearly half of the global population suffer from OSA. Cholelithiasis and OSA are separate medical conditions. However, they both affect a significant part of the general population, have tremendous impact on patients’ overall health, and share common risk factors, pathophysiology and disease development.
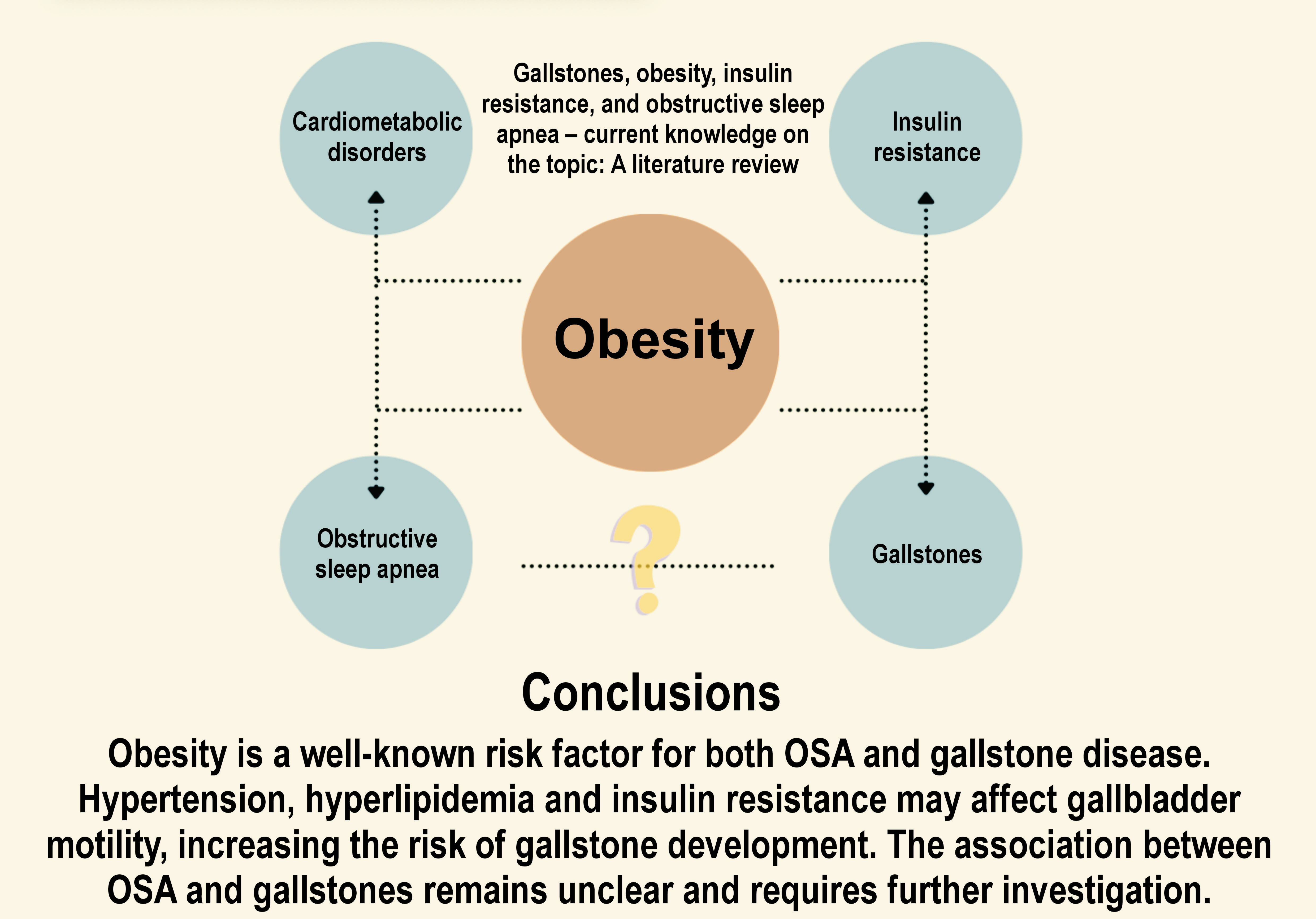
Thus, the aim of this brief narrative review is to summarize and update the current knowledge on the link between gallstone disease and OSA regarding the prevalence of obesity and insulin resistance in patients with both OSA and cholelithiasis.
Keywords: obesity, insulin resistance, obstructive sleep apnea, gallstones, cholelithiasis
Introduction
Gallbladder diseases are among the most frequent gastrointestinal conditions, with a prevalence estimated at 20% in the general population. The prevalence increases with age, constituting a significant burden to healthcare system.1, 2 Gallbladder diseases include, among others, cholelithiasis, cholecystitis, choledocholithiasis, cholangitis, cysts, polyps, and malignancies.3
The diagnosis of gallstones requires the use of non-invasive imaging techniques, such as abdominal ultrasound, computed tomography (CT) of the abdomen and magnetic resonance cholangiopancreatography (MRCP). The invasive techniques, including endoscopic retrograde cholangiopancreatography (ERCP), are chosen as the preferred therapeutic method.1, 2
The treatment of gallstones can be divided into preventive and minimally invasive procedures (e.g., endoscopic or laparoscopic) or urgent treatments that can be either minimally invasive or traditional, depending on patient’s clinical status according to the established guidelines or algorithms.4 Laparoscopic cholecystectomy, the invasive procedure, is estimated to be one of the most prevalent surgical interventions worldwide.5 However, it is a standard to refrain from performing surgical procedures in asymptomatic patients, with a few rare exceptions.6
Obstructive sleep apnea (OSA) is a sleep-related breathing disorder caused by pharyngeal airway collapse. Airway collapse can result in obstructive apnea, hypopnea and snoring.7 The incidence of OSA is constantly rising and is estimated to be between 3.0% and 49.7% in adults depending on sex, population characteristics and study methodology.8 Benjafield et al. estimated that globally, almost 1 billion adults aged 30–69 years have mild to severe OSA, and 425 million adults aged 30–69 years have moderate to severe OSA.9 The gold standard tool in OSA diagnosis is a whole-night polysomnography (PSG). The most common risk factors for the condition include increased weight, male sex and advanced age. Although cholelithiasis and OSA are separate medical disorders, they frequently coexist and affect a significant part of the general population. These conditions have a tremendous impact on patient’s general health, and they often share common risk factors, pathophysiology and disease development.
Thus, the aim of this narrative review is to summarize and update the current understanding of the association between gallstones and OSA.
Material and methods
A comprehensive literature search was conducted using the PubMed®, Scopus and Web of Science databases. The search was limited to articles published between 1990 and 2024. The keywords and phrases used included “gallstones”, “obstructive sleep apnea” and “insulin resistance”. The articles in English concerning the relationship between OSA and gallstones were included. The case reports and non-peer-reviewed articles were excluded from the analysis. A total of 46 studies covering various aspects of gallbladder disease, OSA, insulin resistance, obesity, and their interrelations were reviewed. Table 1 presents a summary of the key findings from the literature.
Results
Development of gallstones
Cholelithiasis is a condition characterized by both clinical and biochemical abnormalities caused by disruptions in bile production and drainage. It can occur anywhere along the biliary tract, from the intrahepatic bile ducts to the opening of the bile ducts into the duodenum in the greater papilla.10, 11, 12, 13, 14 Bile duct diseases have already been diagnosed 3,000 years ago. During archaeological research conducted in Egypt, stones in the gallbladder were found in the mummy of a priestess living in the 11th century BC. However, it was Soranus of Ephesus who first described the symptoms of mechanical jaundice in the 2nd century AD.10
Two main types of gallstones are distinguished: cholesterol stones (90%); and pigment (black, brown) stones (10%). According to the classification based on location, stones can be located in the gallbladder, common bile duct or intrahepatic bile ducts. Gallbladder stones are mostly cholesterol derivatives produced due to insufficient biliary cholesterol turnover. Turnover homeostasis can be disrupted as a consequence of hepatic hypersecretion of cholesterol, rapid phase transitions, intestinal factors, and gallbladder hypomobility. Pigment gallstones are produced as a result of bile stasis, bacterial infection, hepatic hypersecretion of bilirubin, and genetic factors.11, 15 There is a direct correlation between body fat and cholesterol synthesis. Excessive production of cholesterol results in its excretion into the bile, where it is concentrated. This process, in turn, leads to the formation of gallstones.16
Gallstones occur more frequently in women than in men. The main cause of cholelithiasis is metabolic syndrome. The acronym 4F, an abbreviation for “fat, female, fertile, and forty”, is commonly used to enumerate the factors that contribute to the development of cholelithiasis.16 Other risk factors include hyperinsulinemia, insulin resistance, type 2 diabetes, and obesity. Moreover, reduced physical activity and excess caloric intake play a pivotal role in the development of gallstones.2
Regarding the limited body of literature on this topic, the existing studies suggest a link between sleep disorders, obesity and gallstones. Seminal research conducted by Chen et al. assessed the cumulative incidence of gallstones in the OSA cohort compared with the non-OSA cohort.17 Patients with OSA had an increased risk of gallstones (adjusted hazard ratio = 1.53, 95% confidence interval (95% CI) = 1.16–2.03) after adjustment for age, sex, hyperlipidemia, diabetes, hypertension, chronic obstructive pulmonary disease (COPD), stroke, and coronary artery disease (CAD).17 However, a previous study was subject to limitations regarding a relatively small number of obesity cases in the OSA cohort.
Insulin resistance
Insulin resistance has been previously linked to metabolic disorders, including visceral obesity, dyslipidemia and endothelial dysfunction.18 Gallbladder removal (cholecystectomy) has been associated with a frequent manifestation of insulin resistance. This observation has given rise to the theory that the gallbladder is responsible not only for storing and concentrating bile produced in liver but also for metabolic and hormonal regulation.19 The relationship between insulin resistance and OSA has garnered increasing interest from the medical community. Excess fat accumulation in obese individuals results in disrupted fat tissue metabolism, a condition referred to as lipotoxicity.20
Lipotoxicity has been associated with impaired glucose and insulin metabolism, resulting in the disruption of metabolic pathways in both adipose tissue and peripheral organs. The condition has an influence on pancreatic, hepatic, muscular, and cardiac functions. Metabolic alterations related to lipotoxicity impact intracellular signaling and hormonal regulation. An extensive literature review showed that insulin resistance leading to diabetes mellitus and obesity is associated with dysregulation of metabolic pathways, including protein kinase C pathways that influence serine phosphorylation,21 the c-Jun N-terminal kinase (JNK) pathway21 and glucose transporter (GLUT)-4 receptor trafficking.22
GLUTs are transmembrane proteins that transport glucose across the cell membrane. The activation and translocation of these proteins is facilitated by insulin. Insulin resistance increases GLUT-4 receptors in adipocytes present in the heart, brain and skeletal muscles. Obesity, which is associated with visceral adiposity and insulin resistance, increases cardiometabolic risk. However, a large retrospective cohort study from Poland found that obesity is not an independent predictor of return of spontaneous circulation (ROSC) in patients experiencing out-of-hospital cardiac arrests (OHCAs).23
In a PSG-based study, Michalek-Zrabkowska et al. confirmed that OSA is a risk factor for insulin resistance.8 Several studies remain in agreement with these results.24, 25 In general, insulin resistance is crucial in the early stages of type 2 diabetes mellitus development.26 The association of type 2 diabetes with OSA, which has been widely discussed in recent literature, is an independent risk factor for sleep disordered breathing (SDB) and disease progression.27 Moreover, insulin, acting as a growth factor, promotes the expression of genes involved in inflammation.28 Excess body fat leads to chronic systemic inflammation and dysregulation of metabolic pathways, and can result in insulin resistance, pancreatic β-cell dysfunction and atherosclerosis.29
Obesity
Obesity is a major public health problem. According to the World Health Organization (WHO), approx. 39% of adults are overweight and 19% are obese (body mass index (BMI) ≥ 30 kg/m2).30 The condition is strongly associated with numerous disorders, including diabetes mellitus, gallstones and OSA.31 Reduced physical activity and excess caloric intake are the main exogenous factors causing obesity. As a result, there is an elevated propensity for cholesterol synthesis in the liver, which results in an increased risk of gallstone development.2 However, studies have shown that cholecystectomy can increase susceptibility to obesity.16
As previously mentioned, obesity is one of the risk factors the development of OSA. Increased neck circumference has been classified as an indicator of obesity and OSA. Fat deposits around the neck in obese patients can result in the narrowing of the upper airway,32 potentially leading to oxygen desaturation.
In the diagnosis of OSA, questionnaires are often used to obtain possible diagnoses, with the STOP-Bang questionnaire being one of the most widely utilized screening tools. Furthermore, neck circumference and BMI are strongly related to OSA.33 However, PSG and respiratory polygraphy remain the gold standard for the assessment of hypoxia and the severity of sleep fragmentation.
Gastric bypass surgery is a weight reduction procedure that is approved in specific cases. Moreover, glucagon-like peptide-1 (GLP-1) analogues are gaining importance in weight loss management. As a result of bariatric procedure and GLP-1 treatment, rapid weight reduction can be achieved. However, weight loss exceeding 1.5 kg per week has been observed to result in the formation of new gallstones in approx. 25% of patients.34 Nonetheless, prophylactic cholecystectomy is not advised due to complications, unless symptomatic gallstones or intraoperative abnormal findings of the gallbladder are presented.35, 36
The benefits of weight loss outweigh the risks of possible complications, including gallstone formation.37 Weight reduction is considered an important component of treatment in patients with OSA38 and other cardiovascular diseases, and is associated with a decrease in cardiovascular risk.
Discussion
The main symptoms of gallstones are abdominal pain and hepatic colic. There are 3 stages of cholecystitis: mild; moderate; and severe. Patients with mild symptoms are treated acutely when symptoms occur. The main recommendations focus on changing eating habits. Patients exhibiting moderate to severe symptoms are eligible for surgical interventions. However, the predominant risk factor continues to be obesity, which is also associated with cardiometabolic disorders and OSA.
Hyperinsulinemia, insulin resistance and dysregulation of metabolic pathways have a pro-inflammatory potential and can lead to the development of type 2 diabetes, obesity and systemic metabolic dysfunction.39 Hence, the present review suggests that excess development of fatty tissue constitutes the potential link between OSA and gallbladder diseases.
The main question refers to the potential impact of OSA on the risk of gallstone formation. Firstly, OSA can activate enzymes involved in triglyceride synthesis, including sterol-regulatory element-binding protein 1 (SREBP-1) and stearoyl-coenzyme A desaturase-1 (SCD-1).40 Triglyceridemia is related to obesity and insulin resistance, which can lead to impaired gallbladder motility.41 It is noteworthy that hypertension, which occurs concurrently with OSA in most cases, inhibits gallbladder emptying through an increase in sympathetic tone, resulting in an elevated risk of gallstones.33 Moreover, OSA has been demonstrated to cause systemic inflammation via intermittent hypoxia, sleep fragmentation and insulin resistance.42 Respiratory events are followed by arousals in OSA patients, thus resulting in sleep fragmentation. Sleep fragmentation is defined as repetitive short interruptions of sleep.43 In PSG, it is expressed by the arousal index (AI) that measures the number of arousals per hour. Sleep fragmentation can lead to several metabolic and physiological disturbances, including hyperinsulinemia, dysregulation of the lipid profile, increased sympathetic nervous system activity, and hypertension. These factors may contribute to an elevated risk of gallstone formation. In summary, both intermittent hypoxia and sleep fragmentation may increase the risk of cholelithiasis in patients with OSA.
Adipose tissue produces key signaling molecules that significantly influence the development of various diseases, many of which are closely linked to a patient’s psychological state. Notably, both OSA and gallstones, conditions associated with adipose tissue dysfunction, can substantially impact quality of life (QOL).44, 45
To assess QOL in patients with gallstones, numerous scales have been designed. Previous studies have attempted to evaluate patient’s subjective QOL after cholecystectomy, with most reporting notable improvements post-surgery.2
Sleep quality, a fundamental component of overall well-being, is strongly associated with QOL. Altered sleep patterns impair daily functioning and can exacerbate underlying health conditions. In this context, the somatic symptoms associated with chronic cholelithiasis, such as persistent abdominal pain, can contribute to a decline in sleep quality, further decreasing patient’s QOL. This observation highlights a potential feedback loop where gallstone-related symptoms negatively affect sleep, which, in turn, may lead to the deterioration in the perception of health and well-being.
Sleep quality is a subjective and objective form of patient’s sleep evaluation. Numerous conditions can disrupt the overall sleep architecture, including chronic pain associated with somatic disorders, OSA, psychiatric conditions, infections, and musculoskeletal disorders. While PSG remains the gold standard tool for sleep evaluation, self-reported questionnaires are widely used and accepted in both clinical practice and research. Several tools such as the Sleep Apnea Quality of Life Index (SAQLI), the Functional Outcomes of Sleep Questionnaire (FOSQ), and the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) are approved for the evaluation of OSA-related QOL. As anticipated, QOL in patients with OSA is inversely related to the severity of apnea symptoms.46 However, continuous positive airway pressure (CPAP) therapy, the gold standard therapeutic device for moderate to severe OSA, has been observed to enhance patients’ QOL.44
The evidence suggests that gallstone disease and OSA independently, and potentially synergistically, contribute to diminished QOL. This effect may be mediated by similar underlying mechanisms, including chronic inflammation, increased sympathetic activity, and metabolic dysregulation. The question of whether CPAP reduces the risk of gallstone formation remains open due a paucity of research on the topic. In the present study, we aimed to investigate and evaluate the association between OSA and gallstones. To the best of our knowledge, only 1 observational study previously raised concerns about the presence of gallstones in OSA patients.17 However, this study was published recently, and the awareness of the comorbidity of these 2 medical conditions is still an area of increasing attention.
Conclusions
Obesity is a well-established and commonly recognized risk factor for both OSA and gallstone disease. However, other metabolic disturbances, including hypertension, hyperlipidemia and insulin resistance may impair gallbladder motility and promote gallstone development through increased sympathetic nervous system activity, systemic inflammation, and altered cholesterol and triglyceride biosynthesis.
In conclusion, the association between OSA and gallstones is poorly described in the literature and remains unclear. Further research is required to:
– explore the biological mechanisms linking OSA to gallstones, particularly the role of metabolic, inflammatory and hormonal pathways;
– investigate the long-term effects of obesity and insulin resistance on gallstone formation in individuals with OSA;
– examine the impact of OSA treatment, such as CPAP, on the risk or progression of gallstones;
– conduct large-scale, longitudinal studies to better understand the temporal relationship between these conditions and their interaction over time.
Ethics approval and consent to participate
Not applicable.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Use of AI and AI-assisted technologies
Not applicable.